Sometimes, as a parent, you might notice your child struggling to keep up with everyday tasks—handwriting remains jagged even after months of schooling, tying shoelaces feels like climbing Mount Everest, or navigating the chaos of sports day becomes distressing rather than delightful. Questions start whirring in your mind: Is my child just taking a little longer, or is there more to these stumbles? These concerns are not rare—and, in fact, they touch a sizeable number of families. Developmental Coordination Disorder is a term gaining increasing attention among paediatricians and educators alike, precisely because it gives language and context to motor difficulties that otherwise appear mysterious or frustrating for both parents and children. Far from being a reflection of intelligence or motivation, these challenges stake their roots in the way the brain organizes movement. Early identification opens the door for understanding, targeted support, and nurturing a child’s confidence—paving the way for participation, learning, and joy in daily life. Here, every question finds a response: What is this condition? Why does it happen? How can we help children thrive despite it? And, most importantly, what steps are truly effective in creating a nurturing, growth-oriented environment?
Recognising Developmental Coordination Disorder in children
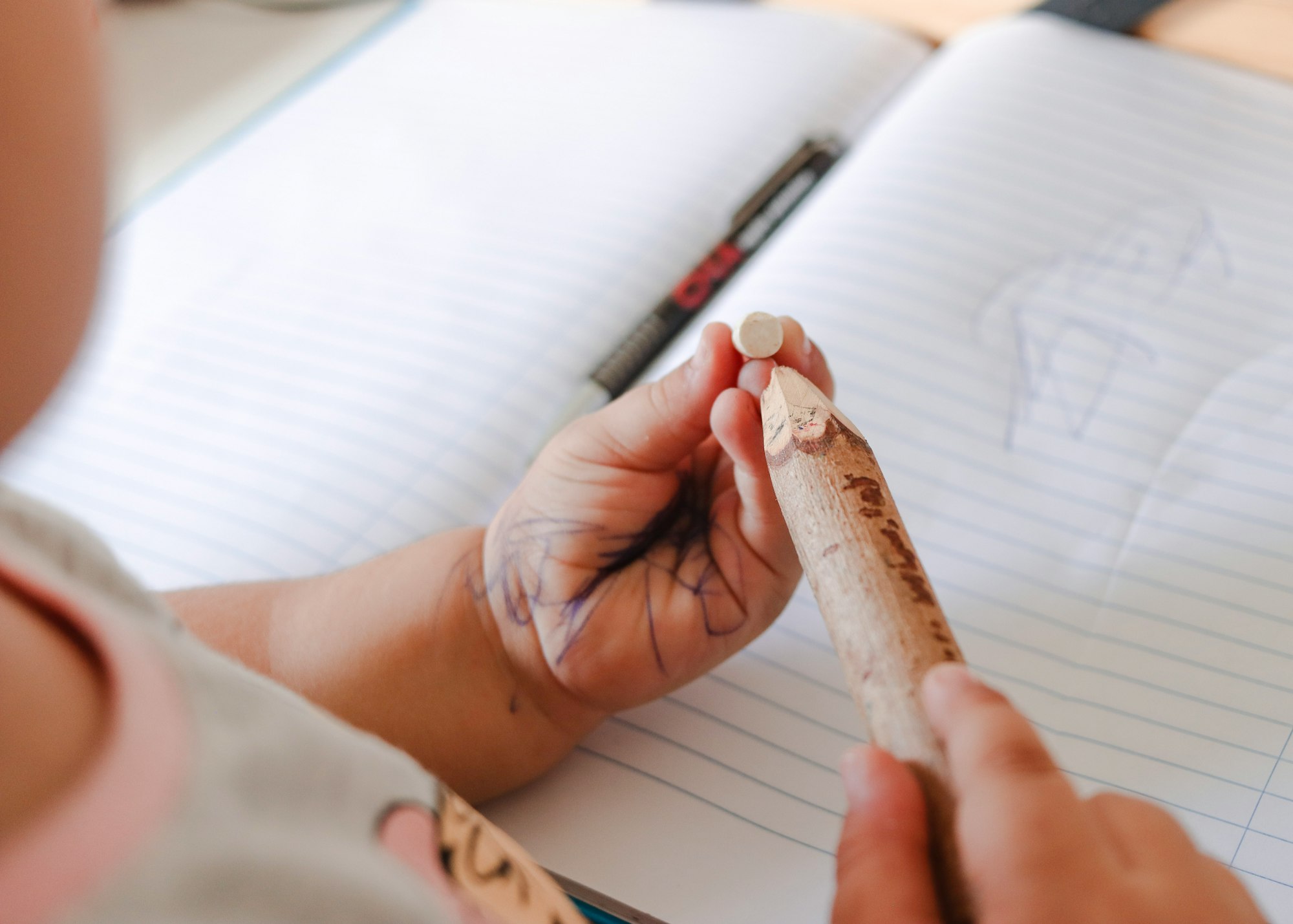
The phrase Developmental Coordination Disorder might sound technical, but the lived experience is clear-cut. Imagine a 7-year-old, bright and curious, yet their pencil seems to have a mind of its own. Buttoning a shirt? Chaotic ballet of fingers. Running on the playground? More often, an unintended tumble. Medically, this is a neurodevelopmental disorder focusing on one core feature: persistent difficulties in acquiring and performing coordinated motor skills—both fine (think thread and needle, drawing shapes) and gross (skipping, jumping, catching a ball).
Contrary to the myth of clumsiness equating to laziness, children with DCD are putting in as much effort—sometimes more—than their peers. What distinguishes Developmental Coordination Disorder is not a lack of will, but a brain circuit that constructs movement differently. Notably, intellectual faculties are usually intact, sometimes even exceptional in areas unrelated to movement, such as verbal skills or social understanding. Most often identified after age five (when reliable assessment is possible), the disorder affects around 5–6% of school-age children—meaning at least one child in nearly every classroom experiences this.
Boys appear in diagnostic statistics more, although research debates whether this difference reflects genuine prevalence or simply the biases in noticing and referring children. It’s important to remember: girls can, and do, experience DCD, sometimes without the recognition or support boys receive.
Why does early recognition matter? Because the longer Developmental Coordination Disorder goes undiagnosed, the more likely a child is to encounter not only practical obstacles, but also emotional burdens—frustration, loss of self-confidence, social withdrawal. Pinpointing DCD early ushers in a cascade of positive changes: strategic intervention, supportive environments, and, most importantly, a family and school system equipped to celebrate every victory.
The nature of DCD: what it is—and what it isn’t
A common misconception is to classify DCD as a disease—something one can catch or cure. Not so. Developmental Coordination Disorder fits into the family of lifelong, neurologically based conditions. It stems from persistent differences in how the brain connects and instructs muscles to execute deliberate, planned movements: holding cutlery, copying notes, brushing teeth. This isn’t a fleeting delay or a habit to be outgrown next month; it’s a different pattern of neural development.
Yet DCD doesn’t paint all abilities with a single brushstroke. Intelligence? Spared. Creativity? Often vibrant. The child who dreads hockey may pen brilliant stories or fascinate everyone with their imaginative play. The focus here is intentionally selective: the challenge lies in motor planning, muscle coordination, and the fine choreography of actions, not in memory, imagination, or reasoning.
Symptoms and Indicators of Developmental Coordination Disorder
How does DCD show up at home or in the classroom? The signs are sometimes subtle, sometimes glaring. A child with Developmental Coordination Disorder will, by definition, find fine motor tasks—handwriting, buttoning, tying laces—out of reach, or at least far harder than their peers. The letters on the page squirm unevenly; paper tears with every scissor attempt. Eating with a spoon may be laborious, and sports morph into a tableau of slips, trips, and missed catches.
It doesn’t end with schoolwork. Self-care routines—dressing, grooming, eating—might take longer, require more adult help, and elicit a fair share of sighs at home. Motor planning, the brain’s way of stringing together movement sequences efficiently, is distinctly affected, causing children to move awkwardly or with visible slowness, particularly under time pressure or when distracted.
These practical hurdles have social ripples. When participating in games seems unattainable, children may avoid group activities, withdrawing rather than risking embarrassment. And with every misunderstood struggle or impatient reaction from adults, the seeds of low self-worth take root. Families who notice these patterns can make a world of difference, simply by recognising that these are not failures, but the hallmarks of a distinct developmental trajectory.
Causes and Origins: Peering into the Brain
Why does Developmental Coordination Disorder occur? The origins are layered, not fitting a single genetic test or environmental checklist. Modern neuroimaging points to subtle, yet meaningful, differences in areas like the parietal cortex, cerebellum, and frontal cortex. These regions collectively construct the “map” for movement—processing sensations, planning actions, and executing them. In DCD, connections between and within these areas build inefficient pathways, making what should be automatic (like walking or catching a ball) into a process requiring relentless focus.
There’s a genetic strand: having a sibling with DCD raises risk. But no “DCD gene” has been found. Environmental threads weave in, too. Premature birth, low birthweight, or exposure to certain prenatal factors raise the chances, not through direct causation, but by subtly altering how the brain structures itself during early development.
Types, Subtypes, and the Unique Profile
A classroom of children with DCD looks nothing like a row of identical obstacles. Some will have overwhelmingly fine motor issues (think writing, drawing, dressing), while others will be hampered more in gross motor tasks (running, jumping, balancing). There can be a blend, shaped by the individual child’s strengths and needs. One child meticulously crafts Lego castles but winces when asked to run a race; another tackles football with enthusiasm but struggles mightily with puzzles or pen-and-paper tasks.
Beyond motor coordination, some children also face executive function issues—attention, working memory, organization—which can complicate both learning and daily routines. The profile is seldom pure or static. As life’s demands change, so do the manifestations of the disorder, demanding flexibility and adaptation from both the child and their family.
DCD, Comorbidities, and Making the Right Diagnosis
It’s not uncommon for Developmental Coordination Disorder to cross paths with other neurodevelopmental conditions. ADHD is a frequent companion—about half of children with ADHD meet diagnostic criteria for DCD as well. The overlap extends to Autism Spectrum Disorder (ASD) and learning disabilities (dyslexic or dysgraphic symptoms, language disorders). Untangling which symptoms belong where is not just academic—it has real-world effects on which therapies work best and how a support plan is constructed.
Ensuring the diagnosis is precise means excluding other causes—cerebral palsy, visual impairment, or global intellectual disability. DCD stands apart, defined by both what it is and what it isn’t. A multidisciplinary team, including paediatricians, occupational therapists, speech-language pathologists, and educators, delivers a nuanced diagnosis.
How is DCD Diagnosed? The Journey to Clarity
Wondering how diagnosis unfolds? Begin with a thorough history—developmental milestones, birth history, timeline of issues. Professionals then observe the child’s movement, sometimes using structured play or task-based activities. Standardised scales—such as the Movement Assessment Battery for Children (MABC-2), Bruininks-Oseretsky Test of Motor Proficiency (BOT-2), and parent questionnaires like the DCD-Q—measure movement combinations, dexterity, balance, and everyday task performance.
Referral and gender biases remain stubborn; boys outnumber girls in diagnosis, though not necessarily in occurrence. Importantly, assessment tools need to fit the cultural setting, and diagnosis before age five is rare, as motor milestone variability makes early categorization challenging.
In practice, this comprehensive assessment avoids unnecessary therapies, ensuring each intervention is chosen mindfully. Collaboration between family and professionals seeds the ground for meaningful progress—never exhausting a child with fruitless interventions, focusing instead on what proves effective.
Strategies for Support: Adapting Home, School, and Social Spaces
Supporting a child with Developmental Coordination Disorder calls for adaptation—not just from the child but from everyone around them. Occupational therapy is often the frontline, using cognitive strategies like CO-OP to break complex tasks into simple, achievable steps. Physical therapy bolsters balance, strength, and large-muscle coordination. Task-specific, repetitive practice, individualized for each child, has the best scientific backing for improvement—think of it as personalised rehearsal rather than general “exercise.”
Schools play an enormous role too. Accommodations—extra time for tests, permission to use a keyboard, visual organisers, structured routines—are not luxury, but necessity. Training for teachers transforms classroom culture, defusing frustration and celebrating small wins in motor learning.
At home, simple changes yield significant results. Dividing larger routines (bathing, getting dressed, packing a bag) into clear, manageable steps; using adaptive utensils; choosing clothes with easy fasteners—each adjustment affirms the child’s agency and reduces exhaustion. Acknowledging the real energy these children spend can transform not only practical outcomes, but the family dynamic as a whole.
Don’t overlook emotional support. Open conversations, celebrating small victories, redirecting focus from perfection to progress—these nurture confidence. Where self-esteem falters, access to psychotherapy or counseling makes a substantial difference.
Encouraging Active Lifestyles and Physical Health
Physical activity isn’t just a medical recommendation: it’s a pillar for coordination, fitness, and mind-body wellbeing. Structured, supportive environments—swimming, cycling, or nature walks—allow children to practice new skills at their own pace, minimising the pressure of comparison. Here, the rule is participation, not competition.
Collaboration with PE teachers ensures meaningful involvement. Activities at home can be playful yet targeted: homemade obstacle courses, simple ball games, or movement challenges. Regular movement also guards against health risks like obesity, delivering benefits well beyond motor skills.
Growing Up With DCD: What to Expect
Developmental Coordination Disorder stretches far beyond childhood. Into the teenage years, then adulthood, the footprint of DCD persists—sometimes visible, sometimes tucked away in more complex tasks. From driving to independent living, the adaptive strategies learnt in childhood remain vital. Transitions—school to college, college to work—often bring new challenges, making ongoing support and autonomy the twin priorities.
Families can facilitate robust coping by empowering young people: teaching planning skills, using assistive technology, and facilitating mental health support as needed. Owning the narrative—moving from secrecy or shame to advocacy and self-acceptance—can be the difference between struggle and flourishing.
The Role of Advocacy, Awareness, and Medical Support
Awareness of Developmental Coordination Disorder is building, but still lags behind better-known conditions. Advocacy groups, healthcare professionals, and educators increasingly band together to share resources, create campaigns, and reshape public perception. The role of open dialogue, sharing stories, and connecting with support communities cannot be overstated; visibility breeds understanding and empathy.
For professionals, ongoing education and willingness to adapt assessment to diverse cultural settings remain priorities. For families, knowing that partnership with practitioners opens doors to resources, support, and sometimes systemic change.
Medical Research and Future Prospects
Science continues to probe deeper—neuroimaging, genetics, and new assessment tools opening up insight into how Developmental Coordination Disorder develops, persists, and responds to therapy. While there’s no “cure,” longitudinal studies clarify how tailored interventions—blending physical, psychological, and adaptive strategies—tip the scales towards better long-term outcomes.
Emerging research is now focusing on adult presentations, mental health, and periods of life transition, as well as the development of culturally sensitive diagnosis tools. The ultimate goal: equipping families and professionals to empower children, whatever their path may be.
Key Takeaways
- Developmental Coordination Disorder is a lifelong neurodevelopmental condition primarily impacting motor coordination and movement learning.
- Early identification and tailored support can dramatically boost confidence and participation in daily life.
- Every child and family journey is distinct; personalized interventions—at home, at school, and socially—enable growth and independence.
- Coordination between parents, educators, and healthcare providers crafts a support system for sustained progress.
- Ongoing advocacy and medical research are enhancing understanding, diagnosis, and support avenues.
- For parents wishing for guidance tailored to their child, resources and free health questionnaires are a click away on the Heloa app.
Questions Parents Ask
Is Developmental Coordination Disorder considered a disability?
Developmental Coordination Disorder may be classified as a disability in medical and educational settings—especially where motor skill challenges strongly affect everyday living, participation, or learning. This categorisation is not meant to negatively label, but to help provide extra support, access accommodations, and secure understanding teachers. Each child presents a unique profile—what matters is getting the right support in the right context.
Does Developmental Coordination Disorder last into adulthood?
Yes, DCD does not simply disappear as the child gets older. For some, symptoms may ease, but challenges with movement often persist through adolescence and adulthood. The face of these difficulties changes—managing a wallet, driving, navigating a workplace might now be impacted. The good news: with early intervention, steady support, and practical strategies, a fulfilling, independent life remains well within reach.
Can you diagnose Developmental Coordination Disorder in teenagers or adults?
Absolutely possible. While most cases are identified in childhood, many individuals only realise the origin of ongoing challenges during teenage or adult years. Diagnosis here depends on careful piecing together of early developmental history, present skill levels, and patterns of daily challenge. Seeking professional advice at any age brings relief, helps explain life-long difficulties, and opens new doors to therapy, self-confidence, and adapted strategies.
Further reading: