Oral thrush in infants—two simple words, yet for many new parents, they’re a source of worry, confusion, and countless questions. Why do these persistent white patches appear in your baby’s mouth? Is it contagious? Should you panic if your newborn refuses to feed or becomes cranky during a perfectly normal morning routine? From the science of Candida albicans to home care steps and the delicate dance of keeping baby and mother comfortable, understanding oral thrush in infants is half the battle—managing it with confidence is the other. Discover how to spot this common fungal infection, when to act, and which steps truly protect your family’s well-being.
What is oral thrush in infants? Definition and first signs
You notice soft, white spots on your baby’s tongue, maybe the inside of the cheeks or even spreading to the lips. They don’t wipe away easily, and behind them might linger a reddened, sometimes raw area. This is oral thrush in infants, a fungal infection owed to the overgrowth of Candida albicans. Though Candida sounds worrisome, it’s actually a regular inhabitant in the mouths and intestines of humans, both young and old. In infants, the immune system is still evolving—incomplete, almost like a fortress under construction—so an imbalance in mouth flora can quickly tip the scale, giving Candida a chance to multiply.
But why does it even happen? Several triggers: recent antibiotic therapy, exposure during vaginal delivery from a mother carrying Candida, premature birth lowering immune defenses, or even after inhaled steroids. Parents may wonder, “Is it my fault?” Far from it—oral thrush in infants is remarkably common, especially in the first six months.
Why are infants especially vulnerable?
Small babies are not miniature adults; their immune shields are unfinished. The delicate balance of microorganisms—beneficial bacteria versus opportunistic fungi—can be upset by antibiotics (prescribed for infections in baby or breastfeeding mother), or simple environmental exposures. If a breastfeeding mother develops cracked or sore nipples from a yeast infection, thrush may shuttle easily between mother and infant. This back-and-forth transmission can become a frustrating cycle without recognition and proper care.
Do pacifiers, bottle teats, or teething toys play a role? Absolutely. Items not properly sterilized can serve as silent vehicles for Candida. Even something as universally harmless as a favourite dummy, if not washed regularly, may increase risk.
Recognising oral thrush in infants: Key symptoms and what sets it apart
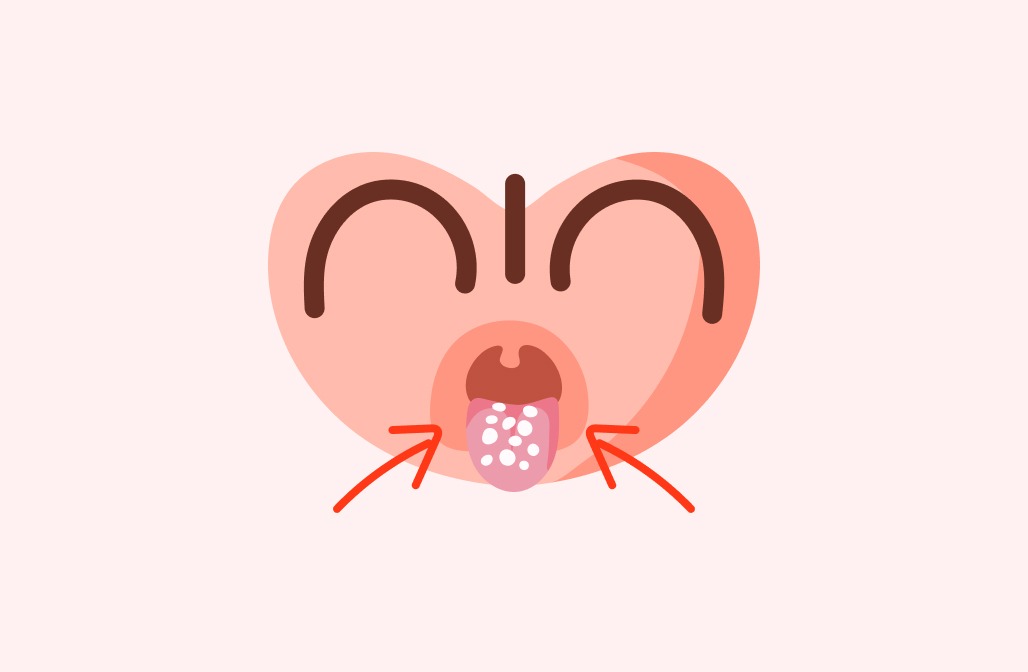
What should alert your eye? Think of white or creamy, cottage cheese-like plaques—persistent, slightly raised, and sometimes forming clusters. They stick to the tongue, gums, inside the cheeks, and the roof of the mouth. Try gently wiping with a clean, damp cloth. Milk residue should disappear, leaving the pink mucosa unscathed, while thrush patches remain and might even leave a red, sore area if rubbed.
Feeding difficulties are common—babies may become fussy, turn away from the breast or bottle, or cry unexpectedly during a feed. Drooling can increase, and you might find cracks developing at the corners of the lips. If the infection extends, a diaper rash may also appear, caused by the same yeast.
But how to tell if it’s more than just milk? The simple “wipe test”—persistent spots indicate thrush, while milk residue vanishes painlessly.
Causes and risk factors: Why does oral thrush in infants develop?
It’s rarely down to “hygiene” alone. Instead, oral thrush in infants happens when natural protective barriers falter. Key risk factors include:
- Immature immune system: especially in premature or very young babies.
- Recent antibiotic use: in the baby, or the mother if breastfeeding. Antibiotics can reduce helpful bacteria, enabling yeast to overgrow.
- Transmission at birth: vaginal delivery from a mother with undiagnosed Candida.
- Inhaled corticosteroids: can also upset the oral environment.
- Pacifiers and bottle teats: if not cleaned/sterilized, become reservoirs for yeast.
- Environmental conditions: persistent moisture, high humidity, crowded living spaces.
Family history—a tendency for fungal infections—may also increase susceptibility.
How oral thrush in infants spreads: Understanding contagion
The spread is almost always by contact—saliva, shared feeding utensils, pacifiers, or breastfeeding (especially if the mother has symptoms). Reinfection is common if only one partner (baby or mother) is treated. Practices that help: sterilising all equipment after every use and regular hand washing, especially after contact with your infant’s mouth.
Diagnosing oral thrush in infants: Medical insight and parent observations
Usually, no laboratory tests are required. A healthcare provider examines the mouth for typical lesions that do not easily wipe away. Sharing details—duration of white patches, feeding issues, recent antibiotic courses—helps refine decisions. If the baby is not improving, or if infection spreads beyond the mouth or recurs, deeper investigation may be needed.
Treatment: Steps to soothe and support your baby
Home-based hygiene and comfort
- Clean your baby’s mouth gently with a soft, damp gauze.
- Sterilise bottles, teats, pacifiers, and teething rings in boiling water.
- Wash hands thoroughly before and after feeds, or after handling feeding equipment.
- Offer feeds more frequently but in smaller amounts if discomfort increases.
Medical treatment
Doctors often prescribe antifungal medications, such as nystatin or miconazole oral gel. These are applied directly to mouth lesions, usually multiple times per day over a week or more. Importantly, continue the course as advised—even if the plaques reduce quickly—since stopping early may allow recurrence.
If the mother develops sore, sensitive, or flaky nipples (sometimes with unusual pain while breastfeeding), both mother and baby require simultaneous treatment. Antifungal creams for the mother, rinsing nipples with clean water, and frequently changing breast pads form an effective routine to break the infection cycle.
When to seek extra help
Prompt medical advice is required if:
- The baby is under four months old and has oral thrush in infants.
- Lesions persist beyond a week of treatment or worsen.
- Feeding becomes very difficult, or the infant displays signs of dehydration (reduced wet diapers, dry mouth, lethargy).
- Poor weight gain or repeated bouts of thrush are observed.
Home care routines: Supporting recovery and preventing recurrence
Continue medication for the full recommended duration. After each feed, clean your baby’s mouth using gentle techniques. Air-dry bottles and pacifiers whenever possible. If a diaper rash arises (sometimes also due to Candida), ensure frequent nappy changes, gentle cleansing, air exposure, and antifungal creams as directed.
Consider whether alternative feeding methods (small cup, spoon) are temporarily helpful if bottle-feeding or direct nursing becomes very uncomfortable.
How to prevent oral thrush in infants
- Sterilise all feeding equipment regularly to prevent Candida growth.
- Clean your baby’s mouth post-feeding, especially if formula or expressed milk is given.
- Let nipples and bottle teats fully air-dry between uses.
- Limit antibiotics and steroids to only what is truly necessary, under medical supervision.
- Encourage nutrition and hydration in both baby and mother, as a balanced immune system is naturally resilient.
- Monitor for recurrent thrush or associated diaper rashes. Any persistent or recurring symptoms merit a professional review.
Breastfeeding and oral thrush in infants: A two-way street
It’s natural to feel frustrated if thrush seems to keep returning. The yeast can shuttle from the baby’s mouth to the mother’s nipple and back. Red, sore, sensitive, or peeling are key signs on the mother. Dual treatment—often with topical antifungals—ensures a better, long-lasting result.
Stopping breastfeeding is not necessary: as long as medication is used as prescribed, most pairs can continue. If pain is too much, expressed breastmilk can be offered. With reassurance, consistency, and gentle care, comfort returns for both baby and mother.
Myths and scientific facts about oral thrush in infants
Perhaps you have heard that oral thrush signals a failure in hygiene, or that only home remedies—such as saltwater or bicarbonate rinses—will do the trick. The truth: oral thrush in infants, while common, is rarely dangerous and is best managed with proven medical antifungals and simple daily routines. Always check before trying homemade solutions, especially for infants.
Parental support: Managing the emotional load
Feeding issues, crying spells, and persistent white spots—these rattling experiences can test even the calmest parent. Know that such difficulties are shared by many and are not a reflection of parental error or lack of care. Try shorter, soothing feeds, gentle cuddles, and bolster your own peace of mind by seeking health advice when things don’t improve.
Professional support (paediatricians, child health nurses, lactation consultants) is accessible and ready to guide you—from prescribed care to emotional reassurance.
Key Takeaways
- Oral thrush in infants often appears as persistent, white patches that resist easy removal.
- Premature infants, antibiotic exposure, or transmission during birth represent common causes—none of which reflect poor parental care.
- Prompt, professional guidance and adherence to recommended hygiene practically guarantee recovery.
- Treat both mother and baby during breastfeeding to prevent reinfections and address all symptoms.
- Rapid, full recovery is the rule—not the exception—with good support and proactive hygiene. For personalised guidance, helpful questionnaires, and parent-focused resources, discover the application Heloa.
Questions Parents Ask
Can oral thrush in infants resolve without much intervention?
Some cases, especially mild ones, might clear as your baby’s immunity matures. However, persistent discomfort or continuous feeding difficulties indicate that it’s best to seek medical attention rather than wait for things to resolve by themselves.
Can oral thrush in infants affect siblings or family members?
Yes, direct contact, shared spoons or teething rings, or breastfeeding from a mother also carrying Candida can allow thrush to spread. Regular hand washing, sterilising bottles and teats, and avoiding shared utensils are simple steps that reduce spreading.
How to make my baby more comfortable at home when dealing with oral thrush in infants?
Gentle cleaning of the mouth, maintaining immaculate hygiene with all bottles, nipples or teething items, and feeding in small, frequent intervals offer comfort. If things don’t improve, or if feeding becomes too distressing, a check with the doctor brings both reassurance and a clear plan for relief.
Further reading: