Addressing the discomfort of sore nipples can feel overwhelming, especially when fatigue and daily responsibilities already press down hard. Maybe you’re noticing stinging, cracking, or an unrelenting tenderness in this sensitive area—sometimes sharp, sometimes more like a deep ache. Sore nipples can turn up whether you are breastfeeding, pregnant, or even simply adapting to hormonal shifts. Do questions swirl in your mind—Why me? How long will this last? Can I do something, today, for relief? Rest assured, a wide palette of medical insight and practical know-how exists to help you. Let’s unravel the causes, dive into the science behind nipple pain, scan for those tell-tale symptoms, and uncover both gentle remedies and evidence-based prevention. You’ll also find clear guidelines on when to seek medical support—a vital tool in any parent’s kit.
Why Do Sore Nipples Happen? Exploring the Causes
Hormonal Fluctuations and Their Ripple Effect
Imagine the tide of hormones that accompanies pregnancy, breastfeeding, menstruation, or menopause. The nipple, teeming with sensitive nerve endings and thin skin, responds dramatically. Estrogen and progesterone—two hormones fluctuating through menstrual cycles and pregnancy—alter skin thickness, moisture, and blood supply. This sometimes leads to exaggerated sensitivity or outright pain. Have you ever noticed that cycle-related tenderness appears—and then disappears just as mysteriously? Such ebb and flow is a story written by your hormones.
Some women report that mid-cycle ovulation brings on surprising nipple sensitivity; for others, the days before periods are a patchwork of discomfort. All of this falls within a broad spectrum of normal—until pain lingers or worsens, hinting that something more may be at play.
Irritation, Friction, and Everyday Trauma
Let’s talk about the unexpected culprits in your wardrobe and daily routine. Tight bras, especially those with seams or underwires pressing against the breast, can invite soreness. Synthetic fabrics—think polyester sports bras—or even simple repetitive motion during exercise (jogger’s nipple) can chafe vulnerable skin, leading to cracks and stinging. Excessive cleaning, particularly with scented soap, or even just frequent contact with rough towels can tip fragile skin into irritation territory.
Sometimes, tenderness comes after nipple piercings or increased sexual activity. The link? Repeated friction and minor trauma, quite different from the hormonal origins of pain but no less real.
Infections and Skin Conditions
It’s not uncommon for sore nipples to become the frontline for fungal or bacterial invaders. Breastfeeding parents might battle thrush—a yeast infection signaled by sharp pain during feeding, sometimes with white patches inside the baby’s mouth—or mastitis, where bacteria drive redness, swelling, fever, and throbbing agony. A single cracked nipple may become the entry point for such infections, so watch for skin changes such as scaling, rashes, or oozing.
Non-infectious skin conditions—eczema, psoriasis, or the less-common contact dermatitis caused by allergies to laundry detergent or body lotion—can also set the nipple area ablaze with itching and soreness. Less frequently, conditions like benign cysts or, very rarely, Paget’s disease and breast cancer, may present with persistent abnormal pain and changes in shape or colour.
Mechanical Stress and Breastfeeding Technique
Especially for breastfeeding mothers, the mechanical side of sore nipples comes sharply into focus. When a baby’s latch is too shallow, or if the nipple is crushed between the baby’s tongue and hard palate, micro-tears and swelling develop fast. Problems sometimes worsen with improper use of breast pumps—flanges that pinch or too-strong suction causing tissue trauma. Even extended feeds, with little recovery time between sessions, stack up the risk.
Symptoms: How to Recognise Sore Nipples
Curious if your discomfort qualifies as “sore nipples”—or if something more complicated is unfolding? Symptoms can swing widely:
- Redness, rawness, or visible cracks
- Swelling or mild bleeding, sometimes with a shiny or glossy appearance
- Blisters, scabbing, or peeling skin (especially around the areola)
- Persistent itch or a rash—sometimes an early sign of eczema or allergic reaction
- Colour changes, from paleness (vasospasm) to dark blue, signalling blood flow disturbances
- Distortion in shape, like inversion or flattening—these warrant closer observation
- Warmth or the presence of pus, coupled with general unwellness, might flag infection
Timing matters too. If pain spikes during breastfeeding, and your baby’s mouth shows white patches, think about possible thrush. If the pain stays long after feeding, or worsens with activity or friction, scan your daily habits or hygiene products for clues.
Diagnosing Sore Nipples: What Should You Watch—and Ask?
A careful eye and honest, detailed reporting forms the launchpad for any diagnosis. Think back: Has your feeding technique changed? Have you switched soaps, detergents, or bras? Are there any new skin problems elsewhere on your body? Using a room with good lighting, gently inspect for cracks, blisters, or swelling; look closely after feeds to spot latching trouble.
If pain is relentless, or skin breaks fail to heal, a doctor may take a skin swab for infection or suggest imaging—ultrasound or mammography—if lumps are present. A detailed review by a lactation consultant can spotlight latch or technique errors invisible to the naked eye. Do not overlook persistent scaling, itch, or odd discharge—such warning signs deserve medical review for rare but concerning causes.
Relief and Treatment: Combining Comfort and Medical Know-How
Practical Home Measures
Comfort sometimes lies in the simplest changes. Cool or warm compresses offer fleeting but significant ease. Soft bras in breathable cotton, and switching to seamless sportswear, can cushion inflamed areas. Keep the skin dry—swap damp pads frequently and let air circulate after feeds. Dabbing a thin layer of expressed breast milk or purified lanolin acts as a gentle shield, supporting skin repair biologically.
For pain relief, non-prescription ibuprofen reduces inflammation and takes the edge off acute discomfort. Remember, a short pause from direct breastfeeding, with careful hand expression to maintain supply, can allow battered skin to recover when sores are severe.
Medical Treatments
When infection steps in (marked by fever, pus, or escalating pain), targeted therapy is key: antifungal creams for thrush, antibiotics for bacterial invaders. Eczema or allergic irritation may settle with a mild, doctor-supervised topical steroid, alongside reverting to fragrance-free cleaning routines. Vasospastic attacks—where the nipple blanches and throbs in the cold—respond to warmth and sometimes, specialist medication.
If breast pumps are part of your routine, it’s wise to double-check the fit and reduce suction; clean every part meticulously to rein in both injury and infectious trouble.
Adjusting Clothing and Routines
Practical adjustments matter more than you’d imagine. Choose bras that provide gentle lift without pressure points. Specially designed nipple shields or barrier creams can come in handy during athletic activities. Limit washing to once or twice a day, favouring mild, hypoallergenic products. Don’t hesitate to drop any practice or product that seems to trigger flare-ups.
Prevention: Supporting Nipple Health Every Day
- Perfect the breastfeeding latch; a deep and comfortable technique prevents most injuries
- Stick to natural-fabric bras and tops—avoid synthetic and tight options
- Use only gentle, fragrance-free cleansers on the breast and nipples; rinse thoroughly
- After every feed, apply a barrier cream or a drop of breast milk—let it dry naturally
- Moisture-wicking breast pads help keep the area dry
- Cover the chest in cold or windy weather to protect from climate-induced vasospasm
- Manage persistent skin issues—eczema or allergies—by following your doctor’s tailored plan
- Choose the right breast pump flange size and maintain good hygiene to limit trauma and infection
- Regularly self-check for any new lumps, scaling, or colour changes, addressing them without delay
When Should You Seek Medical Help?
Delaying support sometimes complicates what could heal faster with the right help. Reach out to a doctor, nurse or lactation consultant when:
- Sore nipples do not ease after a couple of weeks, despite home care
- There’s ongoing, severe pain—whether during feeding or daily routine
- You notice cracks, bleeding, pus, or unusual discharge
- A lump, swelling or fever develops (even mild flu-like symptoms)
- Persistent nipple changes appear: scales, crusts, inversion, abnormal colour—especially if slow to heal
Early advice not only preserves comfort but also protects ongoing breastfeeding and screens for rare but important underlying causes.
Key Takeaways
- Sore nipples can catch anyone by surprise, yet, most recover with gentle changes and attentive skin care
- Hormonal changes, friction, poor latch in breastfeeding, infections, and skin issues dominate the causes
- A smart mix of soft clothing, fragrance-free hygiene, proper technique, and proactive observation avoids most complications
- Seek medical insight for anything lasting, severe, or paired with new lumps, odd discharge, or fever
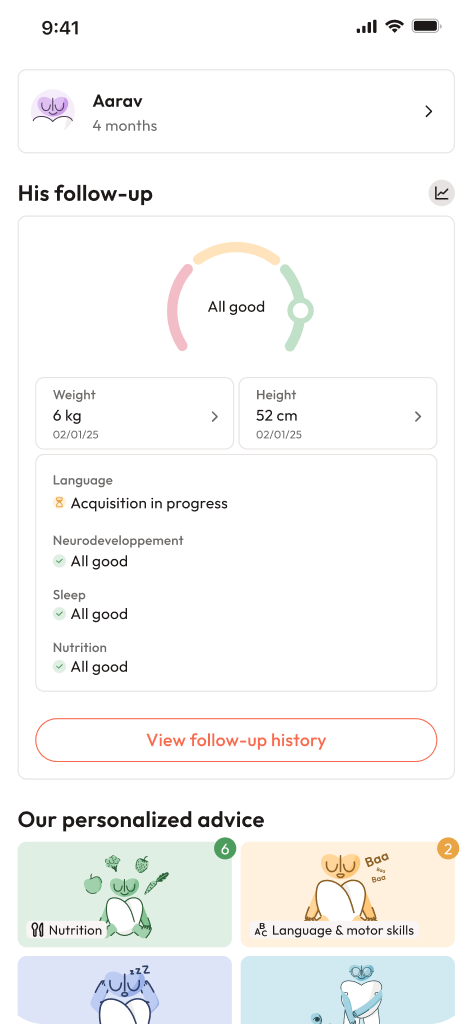
- Reliable help is available—use all resources, from health professionals to digital tools. For more tips and tailored questionnaires on children’s health, download the application Heloa for free advice and parental support.
Questions Parents Ask
Can sore nipples occur even if I’m not breastfeeding?
Absolutely; sore nipples often puzzle parents who are not breastfeeding. Hormonal ripples from menstruation, pregnancy, or menopause frequently make the area extra sensitive. Friction—think rough fabrics or energetic exercise—or even an unpredictable reaction to everyday products like soap or laundry detergent may be culprits too. If discomfort hangs on, a quick consultation with your doctor can point toward an effective solution customised to your situation.
Are sore nipples during ovulation normal?
Yes, this is quite expected. The hormonal dance during ovulation commonly heightens nipple sensitivity—mild discomfort may appear and then fade after a few days. When pain grows more intense or overstays its welcome, mention it at your next check-up for peace of mind.
When should I worry about sore nipples?
Most of the time, sore nipples are no reason for major concern. Yet, it’s important to remain mindful. Watch for sustained pain, persistent changes in colour or shape, unexplained discharge, swelling, or the presence of lumps. Any of these signs mean it’s time to reach out for a medical opinion, ensuring peace and safety for yourself and your family.
Further reading: