Sweltering afternoons, restless children chasing a cricket ball under a blazing sun, or a quick nap in the backseat while waiting for errands to finish—sometimes, small things become the backdrop to one of the greatest anxieties for parents: the risk of heatstroke in children. How to distinguish ordinary fatigue from a lurking danger? Why do children seem to crumple so quickly in the heat, sometimes before warning signs even become apparent? Parents often puzzle over such moments: Is my child too hot? Should I worry if she is drowsy after playing outdoors? Should I insist on more water, even when he refuses? The answers can swiftly swing between reassurance and emergency. This question of exposure, hydration, and vigilant observation is much more than just common sense—medical science brings strong, evidence-backed guidance on how to recognise, prevent, and deal with heatstroke in children.
Let’s unravel what every caregiver needs to know: from the subtle early cues to rapid interventions, and from daily safety tips to long-term aftercare, with the precision of paediatric science and a touch of practical wisdom.
What Makes Children So Vulnerable to Heatstroke?
Children—especially the youngest—inhabit a unique physiological universe. They absorb heat more rapidly than adults, and their bodies, with less mature cooling systems, struggle to keep up. What happens inside? When temperatures climb or a child exerts herself in games and sports, her core temperature can escalate before she has the vocabulary to vocalise discomfort. Unlike adults, a child’s capacity to sweat—one of the main natural cooling strategies—is not fully developed. Breathless after running, flushed and increasingly inattentive, a child may not even realise the danger mounting inside.
Compounding this, little ones often can’t grasp or express thirst with clarity, nor will they always move to a cooler place without prompting. The result? Heatstroke in children may manifest alarmingly quickly, and once it sets in, the margin for safe intervention shrinks. Prolonged exposure—inside stifling cars, poorly ventilated rooms, or under direct sun—can convert routine activities into risky episodes.
Factors Driving Heatstroke in Children
Let’s walk through the most common triggers. The interplay between high ambient temperatures, soaring humidity, and spaces where air cannot circulate—these make up the classic pathway to heat-related illness for children. Closed vehicles are a notorious risk: temperatures inside can soar by 20 degrees in just ten minutes, transforming a harmless wait into a life-threatening event. But it doesn’t end there.
Playing for hours under the midday sun, even with excited cheers for company, can push the body’s limits, particularly if water breaks are skipped. Heavy clothing, thick blankets during naps, or overdressing for fear of chills all contribute to excessive heat retention. Children on specific medications, such as anticholinergics, beta blockers, or diuretics, are at even higher risk because these can blunt the body’s cooling response. Gastrointestinal troubles, vomiting, or diarrhoea, quickly deplete fluid reserves, tipping the balance toward dehydration. In sum, heatstroke in children often develops where environmental stress, hydration gaps, and impaired heat dissipation overlap.
Unmasking the Symptoms: What Should Parents Watch For?
Is it just tiredness—or something more sinister? The first signs can be subtle: a mild fever, irritability, headache, and muscle cramps. Sometimes there’s queasiness, or a bout of vomiting. Lethargy, confusion, or a sudden drop in activity? Red flag. Skin may be hot and flushed, sometimes wet with sweat, but equally, it may feel dry—there’s no single pattern.
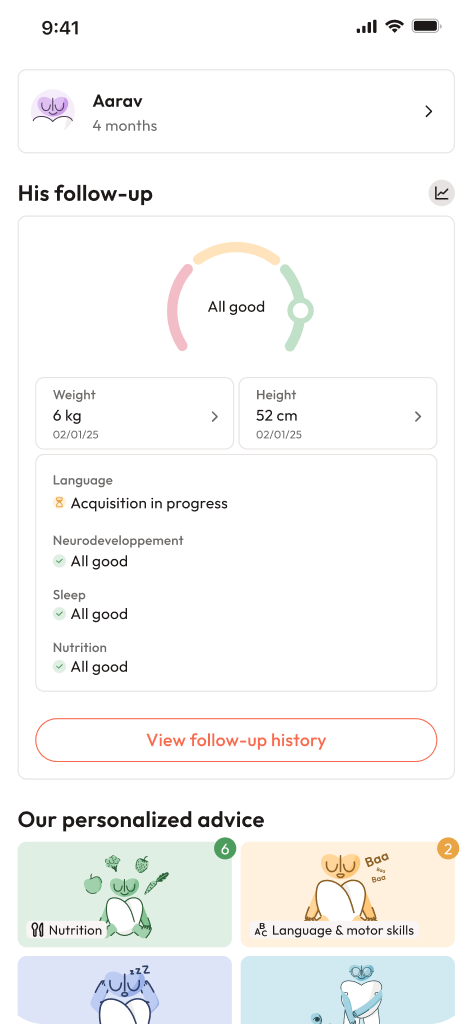
In more severe cases, things spiral alarmingly: temperature spikes beyond 104°F (40°C), children may appear glassy-eyed or delirious, collapse without warning, or have a seizure. For infants, drowsiness, limp limbs, or difficulty waking signals urgent dehydration or heatstroke in children. Shallow, irregular breathing or poor feeding in babies—all demand immediate medical attention.
When Should Parents Seek Help?
A rising temperature above 104°F (40°C). Clouded awareness, abnormal breathing, or a child who can’t be roused. Any such scenario—don’t wait and watch. For the littlest ones, the danger escalates rapidly: their reserve against dehydration is minimal, so even short lapses can have outsized effects.
The Medical Pathway: Diagnosis and Evaluation
If a child with suspected heatstroke lands in the doctor’s hands, several things happen in tandem. Core temperature is quickly measured—often via a rectal thermometer for accuracy. Detailed questions: Was he in a car? Did she vomit recently? Any history of heat exposure, or medications? Blood tests take centre stage, checking everything from electrolyte levels to kidney and liver function, highlighting possible muscle breakdown (rhabdomyolysis), or complications like low blood sugar or electrolyte imbalances. Doctors scrutinise for other possible causes—think infections or toxins—to ensure tailored, effective intervention.
Paediatricians are ever vigilant: differentiating plain exhaustion from true heatstroke in children is urgent, as the window for action can close rapidly.
Emergency First Aid for Heatstroke in Children
Delays can have lasting consequences. If you suspect heatstroke in children, first dial for emergency help—simultaneously, move the child to a shaded, airy location or into an air-conditioned room. Remove excess layers, and bring down the body’s temperature with lukewarm (never ice-cold!) water—splashing with a spray bottle or using wet towels, particularly focusing on the groin, armpits, and neck. A fan? Useful, but only if it doesn’t chill the skin.
If the child is conscious and can swallow, offer small sips of water. Not alert? Avoid forcing fluids. No paracetamol or ibuprofen—these don’t lower fever from heatstroke and could mask warning signs. Never use ice baths, which risk shivering and further complications. If the child becomes unresponsive, recovery position and close monitoring until professional help arrives.
Crucially, even a child who seems to recover should undergo a full hospital evaluation—hidden complications can surface later.
Medical Management in Hospital and Recovery Roadmap
In the hospital, doctors target two themes: steady, controlled cooling, and correcting dehydration with intravenous fluids. Continuous monitoring, frequent checks of vital signs, temperature, and urine output. Blood and urine tests guide ongoing modifications—searching for issues like organ dysfunction, muscle breakdown, or abnormal blood clotting. Doctors carefully avoid cooling the child too quickly lest the pendulum swings to low body temperature.
For some children, especially if complications arose or seizures occurred, longer-term rehabilitation, neurological checks, or physical therapy may be necessary. After discharge, families are counselled regarding signs to monitor, and some children have follow-up checks to catch delayed complications.
Everyday Prevention Strategies for Parents and Caregivers
Prevention need not be elaborate. Try these practices:
- Never, under any excuse, leave a child unattended in a parked vehicle—even for “just a minute.”
- Proactively offer water, since children may not ask—even when quite thirsty.
- Dress them in light, airy fabrics and add a sun hat when outdoors.
- Limit direct sun exposure; encourage play during mornings and evenings, avoiding the peak heat of day.
- Block out sunlight from rooms, use fans, and offer frequent cool baths.
- Use sunscreen generously, but remember—shade and hydration are fundamental.
- Avoid heavy blankets or dressing infants too warmly, particularly for sleep.
- Make double-checking car seats and keeping vehicle doors locked a habit, even at home.
- Teach older children to tune in to body signals—headache, dizziness, or sudden tiredness are warning bells, not just grumpiness from heat.
- Always brief all caregivers—whether grandparents, ayahs, teachers, or sports coaches—on early signs and what to do in an emergency.
Special Focus: Infants, Toddlers, and Medically Fragile Children
Some children require deeper vigilance: babies, toddlers, and kids with chronic illnesses or on heat-sensitive medications. For these little ones, extra caution with dress (no excessive layers!), frequent checks for rapid breath, unexplained crankiness, or reluctance to feed are vital. In hot spells, keep rooms ventilated and as cool as possible—fans or air conditioning when available, and never hesitate to ask a healthcare provider about extra precautions for specific medical conditions.
The Science of Complications: What Happens if Heatstroke Escalates?
Unchecked, heatstroke in children may injure essential organs—the brain (causing memory or learning difficulties, even seizures), kidneys, or liver, and can cause breakdown of muscle tissue (marked by dark urine or muscle pain). The quicker the intervention, the lower the risk of long-term damage. Sometimes, after severe cases, neurological or kidney problems appear later—an argument for scheduled follow-ups, even after apparent recovery.
Trends and Insights: When and Where Is Heatstroke in Children Most Frequent?
Typically, the risk jumps during heatwaves or humid spells. Infants and young children being left in vehicles are the most at-risk group statistically. Notably, children active in sports may see higher rates of exertional heatstroke, emphasising the need for coaches and parents to plan sessions and hydration breaks mindfully.
Debunking Myths about Heatstroke in Children
A prevailing misconception? That heatstroke in children only manifests inside parked cars. In reality, playgrounds, outdoor events, or a nap in a poorly ventilated room can be just as hazardous. Sweating—or the lack of it—cannot alone confirm or rule out heatstroke in children. Medications designed to reduce fever (paracetamol, ibuprofen) do not treat this type of hyperthermia. Also, heat exhaustion and heatstroke aren’t the same: the latter features confusion or unconsciousness and needs immediate action.
Empowering Families: Tools and Resources
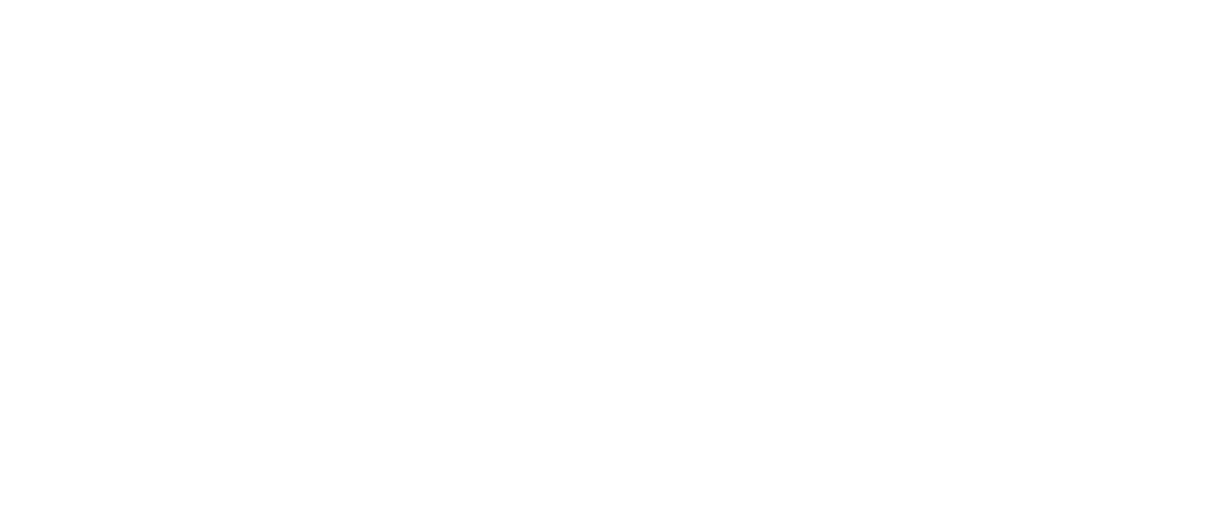
Building healthy hot-weather routines is the everyday foundation. Choose light clothing, plan hydration consciously, set reminders for water breaks, and keep sun exposure for the cooler hours. Encourage honest sharing among children about how their bodies feel. Double-check the backseat before locking your car—the simple steps matter. In moments of doubt, opt for caution and don’t hesitate to seek guidance from a doctor. Those looking for extra support can download the application Heloa for tailored advice and free health questionnaires for children.
Key Takeaways
- Heatstroke in children develops rapidly and can be life-threatening, but prevention is often straightforward with the right awareness and habits.
- Watch closely for early cues—never dismiss fatigue, confusion, or rapid temperature climb as harmless.
- Emergency action saves lives: cool the body, hydrate, and seek medical help swiftly.
- Infants, toddlers, and children with illnesses or on medication require exceptional vigilance.
- Misinformation is common: remember, sweating can deceive, and “just a few minutes” in a hot car is unsafe. Educating all caregivers multiplies protection.
- Professional help is always available—paediatricians and healthcare services provide the backup every parent deserves. For ongoing guidance and tips, turn to reliable resources or try the application Heloa.
Questions Parents Ask
Can heatstroke in children cause long-term complications?
Yes, sometimes, if a child’s core temperature stays very high for too long, it can lead to issues with memory, attention, or muscle strength after recovery. In rare situations, problems with the brain or kidneys can come up weeks later. The good news: children who get quick medical treatment almost always make a full recovery. If you notice lingering fatigue, mood shifts, or frequent headaches after a heatstroke episode, consulting your doctor is a sensible step.
How fast can heatstroke in children develop?
Surprisingly, very fast—sometimes within minutes, especially in hot vehicles or cramped spaces. Playing or participating in sports outdoors during peak heat can trigger symptoms within an hour if hydration is low or children are over-clothed. Young children, unable to verbalise distress, need even closer monitoring.
Which activities put children most at risk for heatstroke?
Strenuous outdoor sports, prolonged games in direct sunlight, even sleeping in a stroller or car seat under the sun—these increase risk, particularly without breaks or access to water and shade. It helps to encourage frequent pauses, offer water, and plan energetic activities for early mornings or late afternoons, when the heat is less intense. With mindful changes, children can continue to enjoy being active—safely.
Further reading: