Babies and parents embarking on that early journey together often encounter a few puzzles—baby reflux is one of the most frequent, and, sometimes, one of the most unsettling. Watching your tiny child spit up, grimace, or squirm after feeds can quickly stir up anxiety, questions, and a search for answers. Is this normal, or is it a sign of a deeper concern? If your days swing between burp cloths and gentle soothing, rest assured, you are among many. Unpacking what “baby reflux” really means, what science reveals about its origins, and the practical ways you can help your child, can bring both clarity and comfort. Let’s delve deep, connecting the dots between physiology, symptom recognition, feeding strategies, and the latest research—all with your daily reality in mind.
Baby reflux: what exactly is happening?
Ever wondered why your baby spits up so often? Baby reflux—technically called gastroesophageal reflux (GER)—shows up when an immature muscle, the lower esophageal sphincter (LES), lets the stomach’s contents flow back to the esophagus. Imagine this valve as a tiny door that isn’t quite strong enough yet to remain shut, especially after a feed. Nearly half of all infants below three months old experience regular spit-ups, most peaking at four to five months. This phenomenon isn’t a rare exception; it’s practically a rite of passage as your child’s digestive system matures during their first year.
But here’s an essential nuance: routine “spitting up” doesn’t always spell trouble. For most, it’s a harmless event—akin to a hiccup or a sneeze—rather than a disease. However, if the reflux escalates, triggering pain, feeding refusal, or slow weight gain, doctors refer to it as gastroesophageal reflux disease (GERD).
Spitting up versus reflux disease: why the distinction matters
Picture this: a baby calmly spitting up after a feed, then beaming a cheeky smile. Compared to another, who arches their back, cries, and resists the bottle or breast—two very different stories. The first fits physiological reflux—a function of that still-developing LES, which usually stays loose until about twelve months old. Nothing to worry about; it’s simply biology in action. But once distress enters the scene, or feeding becomes a struggle, GERD might be at play.
Regular reflux? Almost always harmless and temporary. GERD? Needs closer monitoring, sometimes intervention. Recognizing the difference saves families unnecessary distress and stops hasty, unsuitable remedies.
Causes, triggers, and the anatomy of baby reflux
Why does baby reflux happen so often? Start with the basics: an immature LES that relaxes unexpectedly, allowing milk to come back up. But here’s where feeding practices come into play. Overfeeding, or offering feeds too frequently, stretches a baby’s tiny stomach (imagine the size difference from a cherry at birth to an apple by the first birthday!). When the stomach gets too full—especially before previous milk has had time to empty—reflux becomes far more likely. The result: a stretched tummy, delayed gastric emptying, increased acidity, and irritation at the junction of the stomach and esophagus.
But the plot thickens. Other contributing factors include:
- Diet mostly liquid, which naturally moves more easily
- Lying flat soon after feeds (gravity isn’t there to help)
- Swallowing air—often with bottle-feeding, fast-flow nipples, or rushed schedules
- Allergies, such as cow’s milk protein intolerance
- Prematurity, or neurological conditions
Some scenarios—like eosinophilic esophagitis—are rare, but for most, proactive tweaks in routine offer significant relief.
Breastfeeding, formula, and baby reflux: what’s the difference?
Breast milk is a powerhouse—light, digestible, and custom-made to adapt as your baby grows. For exclusively breastfed babies, reflux usually occurs less frequently and resolves faster. The reason is simple: breast milk moves through the stomach swiftly, is less likely to flood the tummy, and adapts in both quality and quantity to the baby’s needs. Formula, on the other hand, is nutritious but takes longer to digest. Babies fed on formula sometimes face greater risk for baby reflux—not because formula is “bad”, but because it’s heavier, and bottle design or feeding technique might unintentionally invite swallowing more air or overfeeding.
Recognising the symptoms — what’s ordinary, and what’s a warning sign?
Some babies are straightforward: they spit up, squeal, and go right back to napping. Others present subtler signs—a hint of irritability, a persistent cough, or crying that seems hardest after feeds. Typical symptoms of baby reflux are:
- Frequent spit-ups or gentle vomiting
- Hiccups and temporary fussiness
- Occasional coughing, especially after lying down
Worrisome warning signs—those that call for a doctor’s advice—include:
- Poor or no weight gain
- Feeding refusal
- Constant cough, noisy breathing, or respiratory issues
- Projectile vomiting
- Blood in vomit or stool
- Signs of lethargy or dehydration
- Ongoing sleep disturbances or excessive crying outside feeds
A special mention: silent reflux. Here, there’s minimal visible spit-up, but discomfort persists. Persistent cough, gagging, or hoarseness mark this type. In such cases, attentive observation becomes your best tool.
Medical diagnosis, tests, and when to seek further care
When it comes to baby reflux, diagnosis rests mainly on the story you share with your pediatrician: what symptoms appear, when, and how your baby is growing. Most infants don’t require complex testing—just close tracking of weight, behavior, and feeding. If vomiting turns forceful, or symptoms drag on despite all home strategies, investigations may be needed—a contrast X-ray (upper gastrointestinal series), endoscopy, or even pH monitoring, though these remain the exception reserved for more severe, persistent cases.
Classifying baby reflux: three distinct types
- Physiological reflux: classic, almost ceremonial in infancy—baby spits up, shows no distress, and thrives.
- GERD: pain, poor feeding, poor weight gain, or respiratory symptoms enter the scene—attention needed.
- Silent reflux: discomfort masks itself, with irritability, choking, or chronic cough but little or no visible milk.
Tailoring management depends entirely on which scenario unfolds in your household.
Practical feeding strategies and support for baby reflux
Shifting small things in your daily routine can make a world of difference:
- Hold your baby upright as you feed, and for at least 20–30 minutes afterwards—let gravity do some work.
- Stick to smaller, more frequent feeds. Think of your baby’s stomach size; spacing feeds lets milk fully digest before the next round.
- Regular, gentle burping—after every breast or every 30–60 ml if using a bottle—can release swallowed air.
- Consider slow-flow or anti-colic bottles—these cut down swallowed air and tame the feeding pace.
- For suspected allergies, talk to your pediatrician about hydrolysed formula, but never switch formulas indiscriminately.
- Avoid thickening feeds or adding rice cereal unless specifically advised by your healthcare professional.
For breastfeeding mothers, dietary changes are rarely necessary unless under medical suggestion for allergy concerns. Responsive feeding—dosing meals according to hunger cues—remains a gold standard for reducing baby reflux.
Effective management and treating baby reflux at home
Good news: lifestyle changes are your first defense. Medicine is a backup, not a starting point.
- Feed upright, burp often, limit activity after feeding, and keep diapers comfortably loose.
- Let stomachs empty completely between feeds; avoid routine changes to maternal diet without reason.
- Keep your baby’s sleep surface flat, firm, and always on their back, with no wedges, pillows, or positioners (these increase risk).
- For persistent symptoms, especially with suspected food intolerance, your health provider might suggest an allergy elimination diet or hydrolysed/plant-based formula.
Medications—think gastric protectants, H2 blockers, or proton pump inhibitors—come into play only if symptoms impact growth or well-being, and always under vigilant follow-up due to possible side effects. Surgery? Extremely rare—reserved for severe, resistant cases.
Growth tracking is the norm. If vomiting persists, weight gain slows, or respiratory symptoms arise, rapid medical review is warranted.
Consequences and complications: when is baby reflux more than a nuisance?
Most infants with baby reflux mature out of it with zero long-term issues. On rare occasions—especially if GERD persists—complications such as poor weight gain, inflammation of the esophagus (reflux esophagitis), strictures, or recurrent respiratory issues might arise. Sometimes, milk protein allergy masquerades as reflux—symptoms resolve only after a switch to extensively hydrolysed or plant-based formula.
Preventing baby reflux: proactive tips
The best approach for families blends practical measures and gentle, consistent care:
- Upright feeding and post-feed positioning
- Smaller, more regular meals—never force feeds
- Adequate burping, loose diapers post-feed
- Allow the stomach to empty fully before next meal
- Sleep on the back, no wedges or positional gadgets
- Remove environmental triggers (e.g., smoke)
- Educate family and caregivers—consistency eases stress
Common myths—like drastic maternal diet changes or the use of positioners—tend to circulate. Focus on evidence, not anecdote. Above all, stay attuned to your child’s comfort, and trust your instincts; prompt concerns to the pediatrician rather than experimenting with unproven remedies.
Navigating daily life with a baby prone to reflux
Living with baby reflux is an exercise in patience, adaptability, and sometimes flexibility bordering on acrobatics. Routines shift, priorities change, and moments of frustration arise. Friendly support—sometimes from partners, sometimes from medical professionals, and sometimes from other parents in the same boat—makes a significant difference. Keep routines calm, carve out rest wherever possible, and remember: nearly all babies with reflux improve steadily, making the early chaos a distant memory.
Latest medical insights: what science says about baby reflux
Emerging research puts a spotlight on the benign course of most baby reflux cases, underscoring the success of conservative (non-medicinal) approaches. There’s growing caution about acid-suppressing drugs, both due to potential side effects and impact on a baby’s developing microbiome. Preliminary evidence about specific probiotics, such as Lactobacillus reuteri, is intriguing—fewer crying spells, less regurgitation—but large studies are still needed before universal recommendation.
Looking ahead, ongoing research and improved non-invasive diagnostic tools could soon provide more tailored support for infants—and their families—dealing with persistent reflux.
Key Takeaways
- Baby reflux—spitting up, frequent hiccups, and occasional distress—touches almost every family, usually fades away, and rarely leaves a lasting impact.
- Recognising the difference between ordinary reflux and potential warning signs (like poor weight gain, excessive crying, or breathing issues) empowers parents to act when needed.
- Simple, practical feeding and positioning changes are often enough. Medicines remain an option, but only when absolutely warranted.
- Trusted medical advice, calm routines, and a strong support network mean families rarely face this challenge alone.
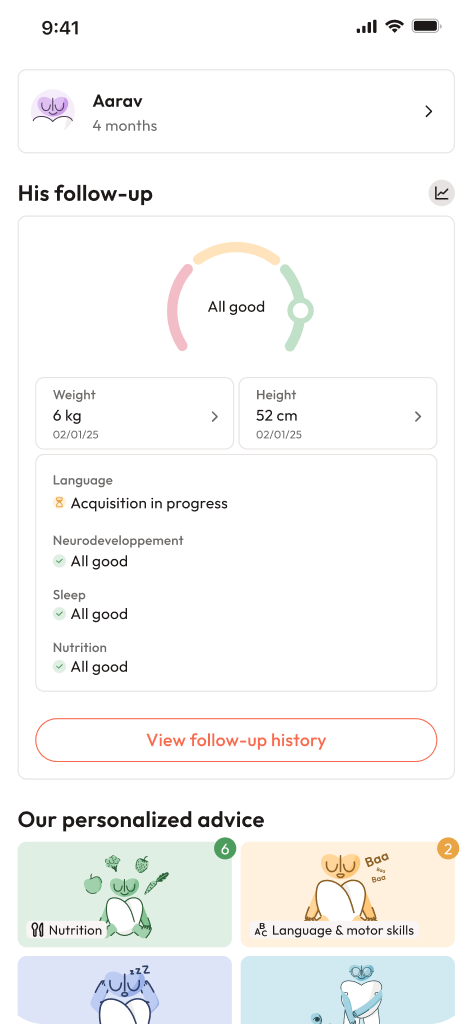
- For personalised guidance, instant health questionnaires, and expert tips tailored to your child’s needs, try the application Heloa.
Questions Parents Ask
Can reflux affect my baby’s sleep?
Many families find that baby reflux creeps into the night, making settling down a bit more difficult. Babies might squirm, fuss, or wake easily after feeds, especially if lying flat feels uncomfortable. To ease this, keeping your infant upright for 20–30 minutes right after a meal can help. Always place your baby on the back to sleep; even with reflux, this reduces the risk of sudden infant death syndrome (SIDS). Temporary sleep disruption caused by baby reflux often gets better as the digestive system matures. If sleep troubles continue or seriously disturb daily life, reaching out to your paediatrician is wise.
Are there home remedies that help with baby reflux?
Of course, gentle home remedies can lighten the load. Fewer, smaller feeds; patient, regular burping; and holding the baby upright after feeds are the go-to tips. Changing bottle design or nipple flow (for bottle-fed babies), or slightly adjusting feeding technique, can sometimes make a notable difference. It is not recommended to elevate the head of the crib or use wedges, due to safety risks. Any changes in feeding routine or diet should be done with medical guidance if symptoms persist.
How long does baby reflux last?
Many parents track the days, waiting for that phase to pass. Baby reflux peaks around four months and fades as babies begin sitting up, eating solids, and their digestive muscle matures—usually between six months and their first birthday. Some children take a bit longer, but the vast majority see full improvement by one year old. If symptoms linger longer, disturb growth, or leave your child unsettled, discussing with your child’s paediatrician is a practical next step.
Further reading: