The birth of a baby ignites countless questions, but nothing grabs attention quite like a bright red or purplish mark blossoming on fragile skin. That first glimpse—a splash of colour, a bump rising where yesterday there was none—can be startling. Is it painful? Will it grow larger? Could it harm my child? Such worries are common when infant hemangioma makes its entrance, often called a “strawberry mark” for its vivid hue and texture. Many parents find themselves scanning their child for changes, juggling between reassurance and concern. What is certain: knowing what to expect, understanding treatments, and recognising risks helps families move from uncertainty to confident care.
Explore how infant hemangioma emerges, why it chooses some babies, how it evolves, and most importantly, how parents can protect, soothe, and support a child as these vascular tumours chart their unpredictable journey—whether fading quietly with time or demanding medical attention.
What Is Infant Hemangioma? Recognising the Mark and Its Nature
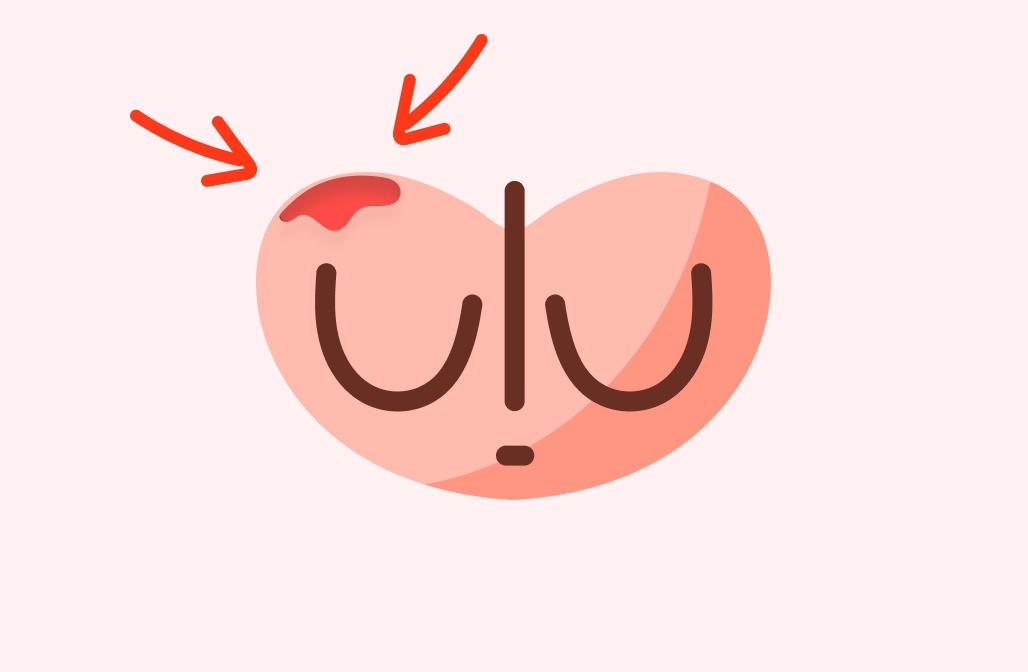
A small, soft growth, strikingly red or at times bluish, suddenly appears—barely noticeable at first, but then it starts to expand. Infant hemangioma stands as the most prevalent benign vascular tumour in infancy, appearing in about 4–5% of babies. Far from being a rarity, it’s seen more frequently in girls, premature infants, and babies of lower birth weight, sometimes clustering along the face or scalp, or surprising parents on the trunk or limbs.
Structurally, an infant hemangioma is made up of an overgrowth of delicate blood vessels (capillaries), forming just under or on the skin. Think of it as a tangle of vessels working overtime—unusually active, but not cancerous. Its drama lies in three main acts: first, rapid growth (the proliferative phase, most intense within 3 to 6 months); second, a stable plateau where size steadies; and third, the gradual fading (the involution phase) which may take several years, often leaving behind a faint shadow, a slight change in texture, perhaps a silvery patch.
How is this different from other marks? Unlike port wine stains or vascular malformations, which stay the same over time, an infant hemangioma has a unique life cycle—intense change, then retreat. One clue for doctors: the GLUT-1 protein marker, present only in these particular tumours.
Why Do Infant Hemangiomas Develop? Unravelling the Risk Factors
Curiosity runs high: Why my child? The answer isn’t straightforward. The precise triggers behind infant hemangioma remain partly mysterious, but science points to a web of influences:
- Prematurity and low birth weight: The smallest and most fragile babies are at higher risk.
- Female gender: Girls, by a margin of up to five to one, outnumber boys.
- Maternal and pregnancy factors: Ageing mothers, twins or triplets, and certain pregnancy procedures (like chorionic villus sampling).
- Hypoxic stress: Episodes of lower oxygen during fetal life may send a signal—blood vessels, grow! This fires up angiogenic factors (proteins like VEGF and GLUT-1).
- Genetic and syndromic cues: Sometimes, hemangiomas cluster in families, or announce themselves as part of syndromes like PHACE—where other organs such as the heart or brain may also show abnormalities.
For most, however, there is no clear family link—just a sporadic quirk of development.
The Making of an Infant Hemangioma: Science Under the Skin
Cells with big ambition—endothelial progenitor cells—are at the core. These are the architects of new blood vessels, usually keeping growth in check. In infant hemangioma, this control slips. Some experts talk of the “placental provenance theory”—a fascinating idea that cells with traits like those from the placenta hitch a ride to the skin, starting a chain reaction. Their signal? Growth factors such as VEGF, triggering new vessels relentlessly.
Visualise the progression:
- Early days: A pale patch, almost invisible, or a faint hint of pink.
- Rapid ascent: Within weeks, a mushrooming of colour—red, raised, sometimes lobulated—heralds the proliferative burst.
- Deep components: If the activity is beneath the surface, bluish swelling emerges—softer, almost sponge-like.
- Retreat: By toddlerhood, slow shrinking sets in, sometimes leaving fibrofatty tissue or delicate telangiectasia (tiny red threads).
Markers such as VEGF, CD31, and especially GLUT-1 help unravel the tumour’s true nature for pathologists, making distinction from other vascular lesions possible.
How Infant Hemangiomas Look, Grow, and Change
Each hemangioma writes its own story, but some themes repeat:
- Superficial hemangioma: Like a strawberry perched on the skin—bright red, defined, and often alarming in its speed.
- Deep hemangioma: Hiding below, it may look bluish or purplish, emerging as a soft, compressible mass.
- Mixed hemangioma: A blend of both, adding complexity to colour and shape.
Where do they appear? While face and neck lead (especially eyelids, lips, or scalp), they can also sprout on limbs, torso, or in rare instances, within internal organs such as the liver. A focal lesion remains small and defined, a segmental one stretches along a larger developmental pathway, while multifocal types sprinkle several sites.
What should parents watch for? Early expansion is common—expect a growth spurt in the first few months, then a calming phase, and ultimately a slow, patient regression.
Typical Locations and Why They Matter
Location matters. A vivid infant hemangioma on the cheek or eyelid commands more worry than a barely visible patch on the leg. Most often, these vascular marks nestle on visible territory: head, neck, eyelids, hands. Function can be touched—if it grows near the eye, vision can blur; if sneaking near the airway or mouth, breathing and feeding could be at risk.
Occasionally, when several skin hemangiomas bloom together, doctors will check for internal involvements—especially the liver—using imaging.
Diagnosing Infant Hemangioma: Clinical Eyes and Modern Tools
Diagnosis is primarily a matter of expertise and pattern recognition. A trained paediatrician or dermatologist can spot an infant hemangioma by watching its behaviour and evolution. Uncertainty (for instance, a rapidly growing or deep-set lesion) prompts imaging:
- Ultrasound with Doppler: Maps out blood flow, helping to distinguish from cysts or other tumours.
- MRI: Provides clarity for large, segmental, or complex lesions.
- CT scan: Reserved for very peculiar cases.
On rare occasions, a biopsy is performed, with the presence of GLUT-1 confirming the diagnosis.
If multiple skin hemangiomas are seen, a liver ultrasound may be in order—multiple superficial marks can sometimes hint at deeper, unseen growths.
Complications: When an Innocent Mark Acts Up
While most infant hemangioma are spectators, never jeopardising health, a minority can cause turbulence:
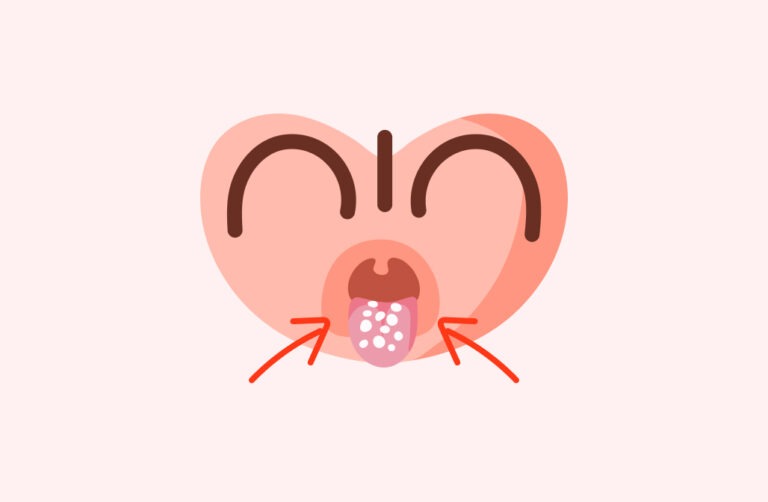
- Ulceration: The skin breaks down—painful, often bleeding, and at risk of infection, notably in areas like the lip or diaper region.
- Bleeding: Usually modest, but sometimes more, if the lesion is bumped or in a vulnerable spot.
- Infection: Secondary to breakdown, requiring careful local care and sometimes antibiotics.
- Threats to function: Hemangiomas near the eye—risking vision; those near the mouth—feeding issues. A strike across the airway? Breathlessness or noisy breathing.
- Liver involvement: Extensive skin hemangiomas can sometimes signal the presence of hemangiomas in the liver, raising the rare risk of hormonal disturbances or heart strain.
- Cosmetics and psychology: Scarring, discolouration, or persistent marks—especially on the face—can touch self-image, later requiring support and sometimes minor cosmetic corrections.
Prognosis and Outlook: The Future for Children with Infant Hemangioma
Good news: time is a friend more often than a foe. In the great majority, infant hemangioma shrinks away—sometimes within a few years, often by age ten. Residual changes? Rarely concerning—slight pallor, a gentle dip, a map of fine vessels. What is important: careful observation and not missing the few cases where rapid change, ulceration, or functional trouble emerge. If the appearance troubles you or your child, small interventions—sometimes dermatological, sometimes emotional support—are available.
Treatments and Management: From Watchful Waiting to Active Therapy
Most infant hemangioma needs no interference—just reassurance and regular check-ups:
- Observation: Gentle watchfulness, especially with small, uncomplicated spots.
- Pharmacological options:
- Oral beta-blockers (propranolol): The mainstay for problematic, rapidly growing, or function-threatening marks. Early initiation is key, with medical monitoring.
- Topical beta-blockers (timolol): For petite, superficial hemangiomas, these eye drop-like gels offer a gentle, targeted approach.
- Corticosteroids: Used infrequently now, yet they have a place if beta-blockers are not suitable.
- Other therapies: For stubborn cases, medicines like vincristine or sirolimus might be tried under specialist guidance.
- Topical creams: Occasionally effective for minor lesions.
- Laser therapy: Pulsed dye lasers target superficial or post-healing redness, especially on the face.
- Surgery: Rare, but reserved for persistent, function-impairing, or ulcerated growths that defy medicine.
- Supportive care: Skincare, wound healing, pain management, plus emotional reassurance for families faced with persistent or visible lesions.
Special Considerations: Unique Cases in Infant Hemangioma
Special care for special situations. Premature babies and those with low birth weight sit at higher risk, deserving closer checks. Marks suggestive of PHACE syndrome or those near vital organs demand a broader clinical team—paediatrician, dermatologist, sometimes neurologist or cardiologist.
Lesions with a “beard” pattern (chin, neck, lower face) ring warning bells for airway involvement—ENT consultation is wise. Near the eyes? An ophthalmologist’s evaluation is essential, as visual development is sensitive even to minor encroachments.
Multiple marks signal internal checks: liver scans, heart monitoring, and holistic consideration of the child’s growth, feeding, and development.
Current Recommendations and Evolving Science
Contemporary management champions an individualised, risk-based approach:
- Low-risk: Routine review every 4–6 weeks in infancy.
- Complicated or risky locations: Early treatment, especially with beta-blockers, after cardiovascular assessment.
- Adjunctive therapies: Laser or surgery, only as needed, tailored to the lesion’s impact on appearance or function.
- Scoring and monitoring: Use of clinical scoring systems and photo documentation to track progress.
- Family education: Helping parents recognise warning signs and understand medicines’ effects.
- Interdisciplinary collaboration: From paediatrician to dermatologist, and when warranted, other specialists join for best outcomes.
Research is advancing: New therapies, alternative beta-blockers, targeted interventions, and the search for reliable biomarkers like VEGF are reshaping future care. Psychological research also reminds us—timely intervention can secure not just skin health, but self-confidence and emotional well-being.
Daily Management and Prevention Tips
No manual exists for preventing infant hemangioma—they are not the result of anything done during pregnancy or after birth. Preventing trauma is practical: keep the area clean, use gentle moisturisers, regularly trim fingernails to prevent scratching, and avoid irritation. Should signs of infection (redness, oozing, pain) or sudden changes develop, medical advice is recommended immediately.
Gentle daily routines—cleansing, moisturising, and attentive monitoring—are the most effective “treatment” for uncomplicated marks.
Supporting Your Child and Family Well-Being
Beyond the medical, living with infant hemangioma weaves a tapestry of emotions. Support is multifaceted:
- Keep the affected area clean and soft.
- Monitor for change: rapid growth, breakdown, or discharge.
- Adhere to any prescribed treatments, and never skip appointments.
- Arm yourself with simple, reassuring responses for curious questions from friends or relatives.
- Engage with parent networks and support groups online or locally—shared experience provides comfort.
- Honest, age-appropriate explanations at home foster acceptance as your child grows.
- Work with teachers so schooldays are as supportive as home.
- Professional counselling is available for children or families who find the psychological impact lingers.
Trust in collaboration—medical, familial, and social—lays the foundation for a thriving, confident future.
Key Takeaways
- Infant hemangiomas are widely seen, generally benign, and most fade away naturally, though a small percentage need treatment if they affect health or essential functions.
- Prompt recognition, ongoing observation, and when needed, early therapy help avoid complications and support healthy development.
- Multiple treatment pathways exist; from “wait and watch” to medications, laser, or surgery, choices adapt to each unique case.
- Comprehensive family understanding and leveraging expert resources enhances both medical and emotional wellbeing.
- Consult your healthcare provider promptly for any skin changes in your child that worry you; and for guidance, download the Heloa app for free questionnaires and tailored health guidance.
Questions Parents Ask
Can infant hemangiomas appear after birth or do they always show at birth?
Many parents feel baffled—a mark that wasn’t there at birth, but suddenly pops up in those first weeks? Entirely normal. Infant hemangioma typically develops postnatally, growing rapidly soon after birth rather than being present from day one. No cause for alarm—delayed appearance is common and not a signal of something being wrong.
Are infant hemangiomas contagious or caused by infections?
Unease about spreading to siblings or being linked to infection is understandable. Rest easy—infant hemangioma is not contagious. Neither viruses nor bacteria play any role, nor does hygiene or anything parents did during pregnancy or after. It is a matter of unusual blood vessel growth, not infection.
Will my child have long-term problems if they had a hemangioma as an infant?
For most children, the chapter closes peacefully. Once an infant hemangioma has faded, the skin may retain a tiny difference in colour or texture—a pale area, a gentle dip, sometimes a few fine vessels. These marks are almost always minor, rarely causing trouble later. Rarely, large or deeply located hemangiomas might leave more obvious changes, but health and growth remain unaffected. For any worry about lasting impact, discussing options with your paediatrician brings reassurance and, if needed, tailored suggestions.
Further reading: