Pregnancy—a word carrying with it an entire world of anticipation, transformation, and sometimes confusion. As soon as the line appears on a test or a faint hope takes hold, a million thoughts can swirl: Is this normal? What happens next? How can the mother and growing child be given the best possible start? These questions linger, whether it is your very first time embarking on this journey or you’re already familiar with baby kicks and trimester milestones. Physical symptoms, emotional swings, dietary restrictions, family support—all these themes can leave parents searching for reliable answers, genuine guidance, and sources of reassurance. Here, we break down the physiological wonders, the challenges, and the everyday actions that shape the pregnancy experience, blending solid scientific information with practical, empathetic advice. Because pregnancy isn’t just a sequence of medical events, but a profound reordering of life, outlook, and even identity.
Understanding Pregnancy: Nature’s Powerful Process
Pregnancy begins with a chain of microscopic events—fertilization of an egg by a sperm—triggering a vast array of changes inside the body. At its heart, pregnancy is the condition where a developing fetus grows inside the uterus, usually for about forty weeks, divided into three trimesters. But behind this familiar definition? There’s ongoing adaptation, not just to support fetal growth, but to prepare both body and mind for the changes to come.
Physical signals often announce pregnancy’s arrival abruptly—perhaps a missed period, breast tenderness, or morning queasiness. Internally, a hormone called human chorionic gonadotropin (hCG) rises, sustaining the new life. The uterus, just the size of your fist at the start, begins to expand, setting off a cascade of changes that touch nearly every organ system. Wondering why energy can suddenly feel absent, or food preferences flip overnight? These shifts are the result of hormonal, metabolic, and circulatory adjustments, all orchestrated for a single purpose: nurturing new life.
Emotionally, pregnancy can be equally unpredictable. The term “psychic transparency” sometimes describes this state—a phase where feelings and memories surface powerfully, questions about the future press close, and the strengths or vulnerabilities inside each person stand magnified. Rather than dismissing emotional ups and downs as just “hormones,” psychologists now recommend viewing them as invitations to self-reflection and support.
How Pregnancy Begins: Biological Insights
The moment of conception can seem almost magical, but it’s defined by biological precision. Ovulation releases an egg, usually midway through the cycle. Fertilization by sperm most commonly occurs in the fallopian tube, forming a zygote. In a process as delicate as it is remarkable, the zygote moves to the uterus and implants, supported by hormonal signals—especially hCG, progesterone, and estrogen. Sometimes this journey unfolds naturally. In other cases, assisted reproductive technologies play a role, particularly if natural conception is difficult. At every step, timing, hormone levels, and overall parental health create the foundation for a healthy start.
The Physical Metamorphosis: Visible and Invisible Shifts
Everyone talks about the “glow” of pregnancy, but the visible transformations run much deeper than occasional radiant skin. Weight gain? Yes, but it’s not just “baby weight”—blood volume increases, body fat redistributes, organs gently shift to make space. The pelvis tilts, ligaments loosen, and a subtle postural dance unfolds daily. Sometimes unexpected changes like thicker hair or sudden pigmentation on the skin appear—small but telling reminders of how deeply pregnancy influences every system.
The physical discomforts? Real, and varied. Morning sickness—a misnomer, as nausea can ambush at any time—might strike fiercely before breakfast or linger all day. Fatigue can flatten even the most energetic. Tips for relief exist: nibbling bland foods, sipping ginger tea, resting often, and breaking large tasks into gentle routines. And if back pain or breathlessness arrive? Consider posture supports, soft shoes, and stretching; the body is recalibrating with every passing week.
Emotional Highs, Lows, and the Search for Balance
The emotional journey through pregnancy rarely follows a straight path. A day can start with euphoria—ecstatic at the first flutter of movement—only to dip later, weighed by doubts or worries. These shifts are not weaknesses; they reflect the powerful hormonal and psychological tides that accompany pregnancy. Group discussions, counseling, or even informal conversations with friends can provide invaluable support. Taking time to reflect, name concerns, or even laugh at small absurdities eases this transition—human connection is a trusted antidote to isolation.
Confirming Pregnancy: Science Meets Intuition
Most people reach for a pregnancy test at the first hint (perhaps a skipped period or unusual fatigue). These tests detect hCG in urine—simple, quick, and increasingly accurate. For even earlier certainty, a blood test delivers answers with more sensitivity, able to spot pregnancy sometimes days before a missed period. Ultrasound, usually performed after a few weeks, offers visible confirmation: the tiny gestational sac, sometimes a softly flickering heartbeat. Whether at home or in the clinic, early confirmation provides clarity, but always follow up with a medical provider to establish tailored, ongoing care.
Early Prenatal Care: The Groundwork for Health
Scheduling an initial visit with a prenatal provider—whether a general practitioner, a gynecologist, or a midwife—lays the cornerstone for a healthy pregnancy. These appointments might seem routine, yet each test (blood, urine, blood pressure) and each discussion about medical history, supplements (like folic acid and iron), and lifestyle sets up targeted care. Regular check-ups aren’t just formalities; they help detect potential issues early—high blood pressure, gestational diabetes, anemia—allowing for timely intervention and reassurance.
Journey Through the Trimesters: Week by Week Evolution
First Trimester
In these first 12 weeks, the transformation is largely behind the scenes. The embryo implants, organs begin forming, and a flicker of heartbeat may be seen as early as the sixth week. Parents may experience nausea, unpredictable moods, and frequent toilet visits. This is the window when pregnancy losses are statistically more common—often due to genetic reasons, not parental actions. Listening to the body, staying hydrated, choosing small meals, and understanding that emotional swings are part of the landscape can turn intimidating moments into manageable ones.
Second Trimester
Relief often arrives: morning sickness fades, energy surges, and the unmistakable “quickening”—baby’s first movements—brings newfound wonder. Anatomy scan around 20 weeks provides a detailed check, sometimes revealing the baby’s gender. Physical changes accelerate: skin darkens in spots, belly grows more pronounced, and minor aches might appear. Blood sugar screening, uterine size assessments, and routine checks mark this period—a stage where many parents begin to truly “show” and connect with the pregnancy.
Third Trimester
As the finish line approaches, anticipation and discomfort often go hand-in-hand. The baby gains weight rapidly, settles head-down, and organs prepare for birth. Sleep gets disrupted, swelling appears, and the urge to finalise the birth plan intensifies. Look for persistent or regular contractions, water breaking, or a sudden decrease in fetal movement—signals not to ignore. Preparation isn’t just about packing a hospital bag; it’s a mental and logistical process, setting up home and heart for what comes next.
Nutrition: Fuelling Mother and Child
A balanced diet packed with vitamins, minerals, and essential nutrients anchors a healthy pregnancy. Iron builds extra blood; calcium and Omega-3 fatty acids support bone and brain growth; folic acid shields against neural tube defects. Forget “eating for two.” The body needs extra calories, yes, but quality matters far more than quantity. Raw meats, high-mercury fish, and unpasteurized products pose infection risks—best avoided entirely. Washing produce thoroughly and trusting in simple, home-cooked meals provides safety and nourishment. For most, supplements fill specific gaps; always consult the prenatal care provider before starting anything new.
The Role of Movement and Gentle Activity
Contrary to old advice, pregnancy thrives with the right kind of movement. Prenatal yoga, swimming, or gentle walks not only ease physical discomforts—think sore back, tight hips—but also restore emotional balance. The physiological benefits extend beyond birth, supporting smoother postpartum recovery. Days of fatigue or pain? Even mindful breathing or a few stretches can offer a reset. The balance lies in listening to your body’s signals and adjusting activity accordingly—progress over perfection.
Soothing the Discomforts
Aches, pains, and digestive twists often accompany pregnancy. Heartburn? Eat small, frequent meals and skip acidic or spicy foods. Sore muscles or ligament pains? Gentle stretching or a prenatal massage can grant relief. Preventative strategies work too: avoid sitting or standing too long; try supportive pillows for sleep. Sometimes, minor adjustments—changing sleep positions, wearing flexible clothing—bring about surprising comfort.
Finding Comfort and Confidence in Changing Bodies
As the body adapts, wardrobe and self-presentation naturally adjust too. Lightweight fabrics such as cotton, soft waistlines, and supportive footwear contribute to ease without compromising style. Skincare might need a gentler approach to prevent irritation. Comfort can be empowering, not a trade-off—embracing new shapes with practical choices and personal touches.
Mental Well-being: Managing Mood and Stress
Mood swings, heightened stress, intense emotions—these are par for the course in pregnancy, fuelled by shifting hormones and real-life anxieties. Sharing feelings with trusted friends or partners can lighten the load. Where stress lingers, mental health resources (like counseling or meditation apps) play a powerful role. Joining community groups creates a sense of belonging—protective against isolation and overwhelm. Remember, strong feelings are normal; seeking support is a sign of strength, not inadequacy.
Essential Screenings and Ongoing Monitoring
Throughout pregnancy, regular check-ups include tracking blood pressure, fetal growth, and screening for issues like gestational diabetes or anemia. Blood and urine analyses monitor for infections and nutritional status, while genetic testing may be suggested for some. Parents with pre-existing conditions (like diabetes or thyroid disorders) benefit from specialist care and closer surveillance—every step calibrated for safety.
Adapting Daily Life: Practical Adjustments
- Medications and Supplements: Discuss all treatments with your healthcare provider. Supplements must match individual needs—not every parent needs the same regimen.
- Safer Lifestyle Choices: Alcohol, tobacco, and recreational drugs have proven risks for the developing baby. Complete avoidance is best.
- Managing Daily Energy: Rest when needed. Reschedule and prioritise. Even for long travel, move regularly—reducing the risk of blood clots.
- Work and Activity: Adjust workload, delegate tasks, and trust your body’s feedback; it knows best when rest or help is required.
Partner and Family Support: Building the Network
Pregnancy feels easier with support. Partners can join consultations, learn about birth options, and share daily responsibilities—nurturing both mother and baby. If siblings are involved, communicate honestly and create small rituals to connect. A network—be it family, friends, or professionals—offers not just practical assistance, but emotional resilience.
Preparing for Labour and Delivery
Prenatal classes demystify the birth experience. Relaxation techniques—like meditation, targeted breathing, or even music—help lower anxiety. Crafting a birth plan clarifies preferences, but flexibility is key, given birth’s unpredictable nature.
The Delivery Moment
Vaginal births are most common, but C-sections sometimes become necessary. Providers will discuss pain relief: medical options (epidurals) and natural techniques (massage, water immersion). Packing essentials for the hospital—comfortable clothes, ID cards, and items for baby—removes last-minute stress and brings peace of mind.
Postpartum Recovery and Newborn Care
Birth is the beginning of another transformation. The uterus continues contracting; lochia (normal bleeding) persists for some time; soreness, whether perineal or abdominal, is common. Good nutrition, as well as gentle movement, aids recovery. If sadness or worry lingers, or if “baby blues” extend, reach out to a specialist promptly.
Feeding a newborn involves choices—breastfeeding supplies natural antibodies and nutrition; formula feeding is a valid, safe option under medical guidance. Lactation consultants or healthcare professionals can troubleshoot concerns. Practical tips around safe sleep, umbilical cord care, and regular check-ups protect the baby’s health at each step.
Fact-Checking the Myths
- Adapted exercise brings benefits, not risks.
- No need to double food portions—moderate, balanced nutrition matters most.
- Morning sickness isn’t tied to the clock—it may appear anytime.
- Certain medications or supplements are both necessary and safe—when professionally supervised.
- Heartburn and baby hair growth? No connection exists.
- Sexual activity is generally safe unless your provider says otherwise.
Key Takeaways
- Pregnancy is a layered, dynamic journey, reshaping both body and mind.
- Personalized, consistent prenatal care optimizes the outcome for mother and child—every history, every body is different.
- Varied nutrition, appropriate physical activity, and open communication about mental health enhance well-being and foster smoother recovery.
- Empathy, self-awareness, and reliable medical advice are essential tools for parents at every stage—resilience grows from support.
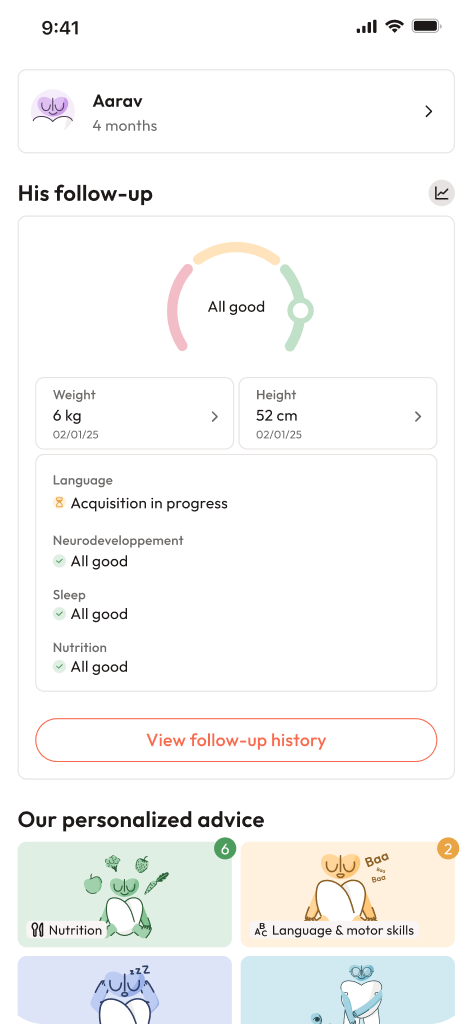
- Multiple resources, both professional and community-based, exist to accompany and guide you. For personalised guidance and free child health questionnaires, download the Heloa application.
Questions Parents Ask
What is a pregnancy calculator and how does it work?
A pregnancy calculator is a user-friendly tool designed to estimate important milestones—like your due date or the beginning of different trimesters. Simply enter the first day of your last period (or sometimes, your conception date), and the calculator gives you a tailored timeline. While these results are based on averages and serve as helpful guidelines, medical check-ups and ultrasounds provide more accurate dates.
How can I confirm pregnancy as early as possible?
If pregnancy is suspected—even before a missed period—the most accessible solution is a home urine test. These measure hCG hormone in urine, which rises early after conception. For quicker or more definitive confirmation, a blood test at the doctor’s clinic offers greater sensitivity, sometimes catching pregnancy even before obvious symptoms. Whether the result is clear or confusing, reaching out to a healthcare professional ensures the best next steps.
What are some common early symptoms of pregnancy?
Most people first notice mild fatigue, breast swelling, nausea (not just in the morning), and more regular urination. Such signs may surface before any period is missed, as hormonal changes take effect swiftly. Some parents feel these immediately, while others hardly notice. If any symptom feels unusual or too intense, a medical opinion can bring reassurance and clarity. In most situations, these reactions indicate natural adaptation to pregnancy—and each experience is unique.
Further reading: