Facing a suspected or confirmed chickenpox pregnancy can instantly send a parent’s mind whirring—what does this mean for you or your future child? The intersection of maternal health and viral infection creates a situation packed with uncertainty, prompting a cascade of urgent questions. Could mere contact with a contagious child change the course of an entire pregnancy? How can you shield your baby if you missed chickenpox as a child or vaccination as an adult? Why does pregnancy transform a usually mild childhood disease into a source of real anxiety? Let’s unravel the facts, examine the science, and bring practical reassurance into a landscape that can, at first glance, seem overwhelming. Expect a deep dive into risks, preventative strategies, medical solutions, and emotional support, all delivered with empathy and scientific clarity.
Understanding Chickenpox Pregnancy: Transmission, Symptoms, and Immune Shifts
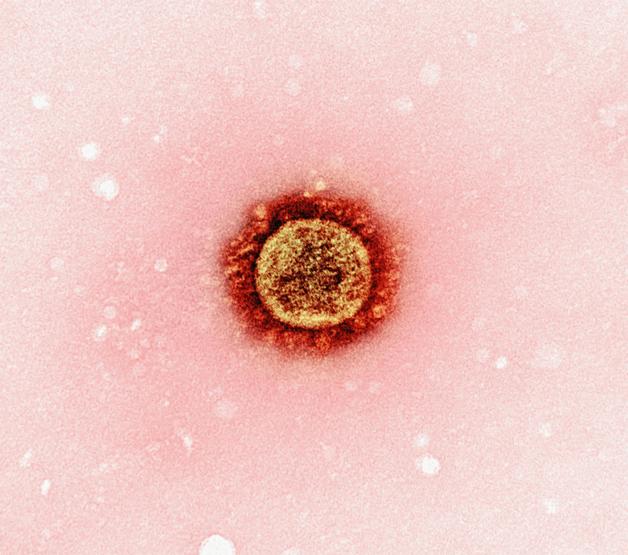
Chickenpox, also recognized as varicella, roots itself as a highly contagious viral infection boldly lurking in places both familiar and unexpected. The varicella-zoster virus travels through airborne droplets—think sneezes, coughs, tight playroom circles—and by direct blister contact, making transmission remarkably efficient. Ever wondered how long a person remains contagious? The infectious period spans from just before the iconic rash blooms until scabs seal each blister, typically covering a week.
The body’s initial response isn’t the rash—subtle signs come first: fever, exhaustion, headache, loss of appetite. Then, the unmistakable red, itchy speckles escalate, forming blisters over the skin’s landscape. For most healthy children, recovery is almost routine—a handful of days, some irritation, and the promise of lifelong immunity. But chickenpox pregnancy raises the stakes dramatically.
During pregnancy, immune defenses are naturally dialed down. This adaptive shift, protecting the growing fetus, ironically renders the mother more susceptible to complications from common infections like chickenpox—even a brief moment near someone infected could be all it takes. In regions with low childhood exposure or suboptimal vaccination rates, the proportion of susceptible women rises, creating unexpected vulnerability at a time when protection feels most vital.
Who’s at Risk? Causes, Exposure, and Immunity
Primary Infection and Major Risk Factors
For those who have neither experienced varicella nor received vaccination, the threat of primary infection during pregnancy is genuine. Everyday settings—nurseries, schools, crowded households—become potential zones of exposure. If immunity remains unconfirmed, a quick blood test for VZV antibodies offers clarity. Non-immune pregnant women must avoid known sources and minimize exposure, as the chickenpox vaccine is strictly contraindicated during pregnancy but can be envisaged postpartum.
Assessing Immunity and Early Response
Not all hope lies in avoidance. Knowing your immune status before conception can be game-changing. If a woman has protective antibodies (positive VZV IgG serology), she stands shielded. If not, the focus pivots to prevention—immunization remains the gold standard for future pregnancies, while post-exposure prophylaxis (like varicella-zoster immune globulin) reduces the ripple of risk if a mishap occurs.
The Symptom Timeline: Recognizing Chickenpox Pregnancy
Clinical Patterns and Disease Onset
Imagine a sudden fever and weariness, joined swiftly by an explosive, itchy rash. That’s classic chickenpox pregnancy. The blisters come in waves, evolve rapidly, burst, crust, and finally heal. This routine takes about 7–10 days, but the path can be treacherous in a pregnant body. The rash usually marks the transition from contagious invisibility to obvious symptoms—too late, often, to prevent household exposure.
Severity Spectrum and Pregnancy-Related Impact
The experience of chickenpox pregnancy covers a notable spectrum: some women witness a handful of lesions and mild discomfort; others suffer high fevers, extensive rashes, and profound fatigue. Severity spikes in adulthood, especially under the altered immune settings of pregnancy or with complicating factors such as smoking or respiratory issues.
Maternal and Fetal Risks: Why Timing Changes Everything
Risks for the Mother: Beyond the Skin
Chickenpox in pregnancy isn’t simply an irritating rash. The risks surge in the third trimester or for those with compromised lung function—varicella pneumonia can emerge, defined by persistent cough and breathlessness. Rapid progression to shortness of breath sometimes leads to hospital stays, specialized respiratory support, or even more advanced interventions. Rarer developments, like hepatitis or encephalitis, remain possible, demanding vigilant medical attention.
Fetal and Neonatal Consequences: The Critical Window
Timing is everything.
- First to Early Second Trimester (Weeks 7–20): Here, congenital varicella syndrome (CVS) looms, although rarely (just 1–3% of cases). CVS translates to a heartbreaking constellation: skin scarring, limb defects, neurological delays, even ocular or developmental complications.
- Later Pregnancy (After 20 weeks): The direct risk for CVS tapers, but other concerns persist. The virus can lie dormant and resurface as shingles in early childhood, an unpredictable twist.
- Around Birth: Infection between five days before and two days after delivery exposes the newborn to neonatal varicella. Without maternal antibodies, the disease can become severe, sometimes life-threatening, and demands swift neonatal intervention.
Maternal illness is not merely a side note—it can trigger preterm delivery, fetal growth restriction, and necessitate intensified prenatal surveillance.
Diagnosis and Monitoring: Science in Action
Confirming Chickenpox Pregnancy
A brisk clinical inspection often identifies the classic vesicular rash. But confirmation depends on thorough history (prior infection or vaccine?), and for certainty, a serological VZV antibody test. The period of infectivity lies hidden—spanning 24–48 hours before the skin erupts, lasting until 72 hours after crusting. This invisible window underlines the importance of timely response.
Watching Over the Baby: Fetal Surveillance
If infection strikes, especially before mid-pregnancy, gentle precision guides management. Serial ultrasounds meticulously screen for fetal anomalies—growth restriction, limb abnormalities, even neurological changes. When ultrasounds spark concern, amniocentesis and PCR for viral DNA can provide further answers. The risk for CVS decreases as pregnancy advances, but monitoring remains unwavering.
Practical Management: Maternal, Fetal, and Neonatal Care
Antivirals: A Race Against Time
At the first hint of chickenpox pregnancy, early antiviral therapy is pivotal. Acyclovir or valacyclovir soothes the course, easing symptoms and curbing complications, especially if begun within the narrow 24-hour window after rash onset. Severe cases, particularly those with lung involvement, may involve hospital admission for intravenous treatment and close monitoring.
What If Exposure Happens? Prevention After the Fact
Contact with chickenpox during pregnancy—what now? Rapid assessment is vital. Varicella-zoster immune globulin (VZIG), administered within 10 days post-exposure, steers the immune system toward protection, mitigating severe outcomes. Should immunoglobulin be unavailable or given too late, preemptive antivirals may still truncate the infection’s trajectory.
Safeguarding the At-Risk Newborn
For infants entering the world within the high-risk window (mother rash onset five days before to two days after birth), immediate administration of immune globulin or acyclovir is advised, regardless of symptoms. Isolation and dedicated monitoring in neonatal care ensure any complication is anticipated and addressed promptly.
And what about breastfeeding? Not only is it generally safe—it is encouraged. Breast milk delivers an extra dose of maternal antibodies, even if not entirely sufficient for full protection. If blistering occurs on the breast, feeding from the affected side should be paused until healing starts, but pumped milk remains a valuable resource.
Preventive Strategies: Looking Forward with Confidence
Preconception Vaccination—the Highest Standard
For those preparing for pregnancy, knowing your chickenpox status matters. Absence of immunity should prompt two doses of varicella vaccine, with a safety interval of at least a month before conception. While the vaccine is not permitted during pregnancy, it is safe immediately after childbirth—even for breastfeeding mothers.
Simple but Effective: Hygiene and Isolation
Amid outbreaks, strict home hygiene, immediate isolation of contagious members, and minimizing contact with unvaccinated or at-risk individuals stand as primary shields. Vaccination of non-immune family members further fortifies the household barrier.
Rapid professional assessment after suspected exposure, rather than waiting for symptoms, makes all the difference: time-sensitive interventions calibrate risk and proactive care ensures safety.
Parental Empowerment: Practical Advice and Daily Solutions
Responding to High-Risk Contact
If contact with chickenpox is suspected, quick action outpaces uncertainty. Immediate medical advice, antibody testing, and—if needed—antiviral or immunoglobulin administration can be started before symptoms even appear, stacking the odds in favor of a mild course.
Any sign of unexplained fever or rash? Speed is an ally—prompt medical care and early antivirals can dramatically transform the outcome.
Family and Emotional Well-being
Protecting the more vulnerable (such as newborns, immunocompromised, or preterm babies) calls for clear boundaries, diligent hygiene, and up-to-date vaccinations in the home. Staying informed, sustaining communication with healthcare providers, and seeking emotional reassurance keep anxiety at bay and resilience strong—there is support, both practical and psychological, for every step of the journey.
Tailored Guidance Through Pregnancy Stages
- Before 20 weeks: Intensified ultrasound monitoring is used to pinpoint possible fetal complications.
- After 36 weeks: Newborns are observed meticulously, and preventive treatment is provided as appropriate—even before symptoms emerge.
Personalized care in concert with medical teams—rapid diagnosis, precise follow-up, and ongoing support—shapes the path toward a favorable outcome for mother and baby.
Medical Pathways and Breastfeeding: A Balanced Approach
Routine prenatal screening checks for chickenpox immunity at the first appointment. When non-immune women are exposed, VZIG reduces risk; confirmed cases get antiviral therapy immediately. Severe forms (pneumonia, nervous system involvement) mean hospital care, sometimes intensive.
If maternal chickenpox erupts close to delivery, the newborn’s safety is prioritized: specialized nursery, potential IV acyclovir, and VZIG are frontline tools. Breastfeeding remains a positive force, even during active infection—mothers should simply adjust the method if breast lesions appear, leveraging pumped milk or alternate side until healed.
Key Takeaways
- Chickenpox pregnancy demands agility in prevention, diagnosis, and responsive care. The interplay of timing, immune status, and rapid intervention dramatically influences maternal and fetal well-being.
- Early identification—through serology, history, or swift post-exposure actions (including VZIG and antiviral medications)—sets the tone for both prevention and management.
- Vigilance is not an option but a positive act of care: close monitoring (ultrasound, neonatal assessment), combined with practical daily precautions, strengthens family safety even in periods of heightened risk.
- Practical support abounds—emotional reassurance, detailed medical information, and ongoing communication with professionals light the way through any chickenpox pregnancy scenario.
- Personalized advice is always within reach: for interactive tips and tailored questionnaires, parents can download the Heloa application, which brings reliable answers and peace of mind into daily family life.
Questions Parents Ask
Can I get chickenpox during pregnancy if I had it as a child?
If you had chickenpox as a child, your body has developed natural immunity, making it very unlikely to catch the infection again. That immunity is usually lifelong. However, if you are unsure about your history or exposure, a simple blood test can check your immunity status. Your healthcare provider can help provide reassurance or guide you on the next steps if needed.
What happens if I am exposed to chickenpox while pregnant and I’m not immune?
If you haven’t had chickenpox before or you’re unsure of your immunity, it’s understandable to feel concerned after exposure. In this case, it is important to reach out to your healthcare provider quickly. Medical options, such as receiving varicella-zoster immunoglobulin (VZIG), can be offered soon after exposure to help lower the risk of developing severe infection. Early treatment and support can make a big difference, so don’t hesitate to ask for advice as soon as you are aware of any contact.
Are there risks if I catch chickenpox in early pregnancy?
Catching chickenpox in the first half of pregnancy can, in rare cases, affect the baby and increase the risk of congenital varicella syndrome (CVS), which may lead to certain developmental concerns. Although these situations are quite uncommon, it is natural to worry. Medical monitoring, including regular ultrasounds, will help assess your baby’s well-being throughout pregnancy. Your medical team is there to guide and support you every step of the way.

Further reading: