Anticipating the arrival of a new baby—an experience as exhilarating as it is full of unanswered questions. You might be feeling everything all at once: joy, anxiety, curiosity, maybe even doubt. How can parents safeguard their well-being and that of their baby? Prenatal care, a concept that might sound technical at first glance, is in fact the living fabric of medical support and reassurance offered throughout pregnancy. It’s not just a series of checkups—it’s an ongoing conversation with healthcare professionals, blending evidence-based science and personalized guidance. If the mere mention of ultrasounds, screening tests, blood draws or nutrition advice leaves you with mixed emotions, you are in good company with countless parents who want clarity, tools, and above all, peace of mind. Together, let’s demystify the pillars of prenatal care—why it matters, what it really involves, the vital milestones and everyday actions that shape a healthy pregnancy, and how best to face challenges that might arise. With equal parts scientific rigor and genuine compassion, here is a complete overview designed to answer not just your questions, but the ones you didn’t know you had.
Understanding Prenatal Care: Foundations for Parent and Baby
The term prenatal care encompasses a broad array of medical check-ups, personalized medical support, and preventive healthcare. Rather than an endless succession of routine appointments, think of this as an active partnership between you and your care team—obstetricians, midwives, family doctors, and at times, specialists. What’s involved? Physical exams for mother and baby, prenatal screening for genetic or infectious diseases, and crucial ultrasound scans conducted at specific intervals. The importance of nutritional advice shouldn’t be underestimated; ensuring sufficient intake of folic acid, iron, calcium, and omega-3 fatty acids can quite literally shape your baby’s future health. There’s increasing attention paid to emotional resilience—screening for anxiety or prenatal depression has become as vital as checking blood pressure.
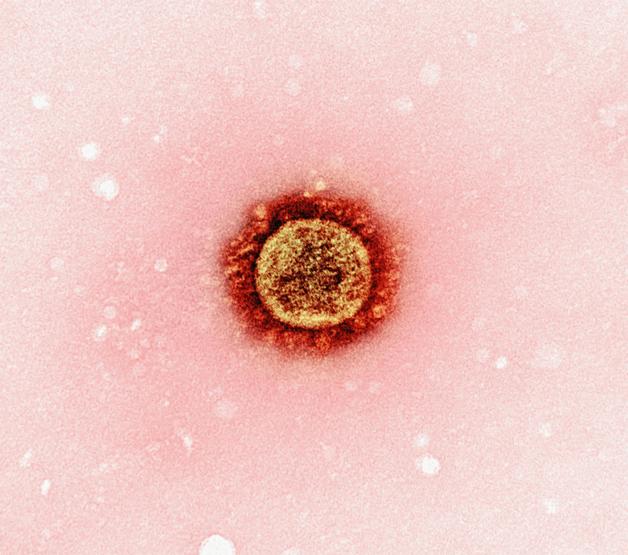
Modern advances—non-invasive prenatal testing, high-resolution fetal ultrasound imaging, and data-driven supplements—have dramatically improved what can be detected and managed. Each stage of prenatal care is an opportunity for early detection and timely intervention, optimizing outcomes for you and your future child.
The Purpose Behind Prenatal Care: More Than Routine Visits
Why commit to scheduled visits? The answer is surprisingly straightforward: prenatal care enables early identification of complications like preeclampsia, gestational diabetes, or fetal growth challenges, often before symptoms become apparent. Regular biochemical screenings, ultrasound checkpoints, and careful growth monitoring offer windows into how your pregnancy progresses. That folic acid supplement isn’t just another pill—taken early, it can dramatically reduce the risk of neural tube defects, among the most severe congenital anomalies. Meanwhile, ongoing assessments permit proactive management of chronic conditions, whether hypertension, diabetes, or less common metabolic disorders, paving the way for a full-term, healthier pregnancy.
It’s the steady rhythm of prenatal visits that acts as a protective net, giving you and your care team the information to adapt, respond, and intervene when it’s most effective.
Rhythm and Timing: When and How Often Are Prenatal Visits Needed?
The calendar for prenatal care is structured, but adaptable. Unlike a rigid schedule, the frequency of visits flexes based on trimester, personal risk factors, and emerging findings:
- First trimester (weeks 1–14): The journey begins with an early visit to confirm pregnancy. Here, comprehensive blood tests are typically conducted (screening for rubella, HIV, hepatitis, toxoplasmosis, and more). For most, checkups are every four weeks.
- Second trimester (weeks 15–28): Appointments shift to every three or four weeks, continuing with lab work and development monitoring.
- Third trimester (weeks 29–40): As delivery nears, visits speed up—first every 2–3 weeks, then every week after week 36. In the ninth month, biweekly visits often provide final reassurance and preparation.
Do high-risk pregnancies require different timelines? Absolutely. Pregnancies complicated by chronic illness, multiples, or previous complications may call for even more regular follow-up, often coordinated among various specialists. Expectations at every visit: measurement of vital signs, urine checks, fetal growth assessments, and symptom reviews—offering a holistic snapshot each time. Milestone tests—ultrasounds, glucose tolerance testing, Group B Streptococcus screening—are slotted in based on your risk profile and week of pregnancy.
Ultrasound Scans: Essential Snapshots of Development
If ever a medical tool embodied the magic of seeing the unseen, it’s the prenatal ultrasound. But what exactly are clinicians looking for, and when? Let’s break down the key milestones:
- First trimester (11–13 weeks): This is about confirming dates, counting heartbeats, and measuring nuchal translucency (a marker for chromosomal conditions like Down syndrome).
- Second trimester (20–25 weeks): The so-called anatomy scan; here’s where major organ systems and detailed fetal morphology become visible. Structural anomalies—heart, spine, kidneys—are best identified now.
- Third trimester (30–35 weeks): Focus shifts to fetal growth, amount of amniotic fluid, placental location, and fetal position (is baby head down, or breech?).
Additional scans may be recommended if there’s a personal or family history of anomalies, previous concerning findings, or new maternal health developments. Each scan is a data point in your baby’s evolving story.
What Happens at Each Prenatal Care Appointment?
A typical prenatal care visit? There’s a pattern, but also infinite variation. Expect a review of medical and family history, ongoing symptom checklists, and serial physical measures—blood pressure, urine, weight (these sound basic but help reveal issues such as gestational hypertension or early preeclampsia). Mental health matters, too; candid conversations about stress, sleep, and emotional swings are increasingly routine. Early visits focus on confirming pregnancy and adjusting timelines. Later, expect assessments of fundal height (the size of the uterus), fetal heartbeat, and guidance about physical discomforts—which may range from heartburn to sleep disturbances.
What about lab tests? After the baseline battery (complete blood count, blood typing, immunity screens, infectious disease status), additional tests (thyroid function, targeted genetic testing) are considered based on individual risk. In the third trimester, glucose tests screen for gestational diabetes, and Group B Streptococcus swabbing helps prepare for safe delivery. Every visit is a checkpoint—an opportunity for reassurance, education, and proactive guidance.
Nutrition and Lifestyle: Building Habits for a Healthy Pregnancy
If one aspect of prenatal care generates more questions than any other, it’s nutrition. What should you eat? Which foods are off limits? A balanced diet is your foundation, emphasizing folic acid, iron, calcium, and essential fatty acids (think omega-3s for brain development). Hydration matters—aim for around ten glasses of water daily, adjusting based on climate and activity level. Some dietary restrictions may surprise: unpasteurized cheeses, undercooked meats, and high-mercury fish (like swordfish, large tuna) pose infection or toxicity risks.
Caffeine and artificial sweetener intake—limit, but don’t panic if you indulge modestly. Every medication (even over-the-counters) should be cleared with your provider; certain substances, known as teratogens, can disrupt healthy fetal development.
Physical activity is typically encouraged—walking, swimming, or prenatal yoga can alleviate stress and promote cardiovascular health. However, activities with a high risk of falls or trauma are best avoided. Environmental hazards (paint fumes, pesticides, lead exposure) should be minimized wherever feasible. Above all: tobacco, alcohol, and recreational drugs are tightly linked to adverse pregnancy outcomes and are uniformly discouraged.
Facing the Ups and Downs: Common Concerns During Pregnancy
Morning sickness. Fluctuating emotions. Uneven weight gain. These are not just clichés—they are among the most common, and distressing, realities of pregnancy. For nausea, simple strategies (small, frequent meals, extra fluids, avoiding known triggers) often suffice, yet persistent vomiting deserves medical attention. Weight gain targets are usually personalized based on your starting BMI, but expectations and recommendations will be discussed with your care provider throughout prenatal care.
Emotional health counts just as much as physical health. Symptoms of stress, anxiety, or depression are never brushed aside; open conversation, mindfulness techniques, and professional support can make a world of difference. Many parents find value in prenatal classes, learning about labor, making informed decisions about pain management and birth planning, and involving partners—who, by attending, gain knowledge and become a more effective support system.
High-Risk or Special Circumstances: Personalized Monitoring and Support
For some, prenatal care means extra vigilance. Teen pregnancies, pregnancies in women over 35, those living with chronic medical issues, or those expecting multiples—each group faces unique risks. Extra ultrasound scans, non-stress tests (external fetal heart monitoring), and tailored blood work are standard. Consultations with maternal-fetal medicine specialists may offer nuanced management strategies, and genetic counseling can clarify options for those at risk of inherited disorders.
Coordination is everything: referrals to nutritionists, mental health providers, or community organizations help manage medical and psychosocial challenges. Multiples require more frequent scans and careful monitoring for preterm labor. Communication—between all professionals and with parents—is the linchpin that sustains trust, understanding, and positive outcomes.
Choosing Your Prenatal Care Provider: Points to Consider
Whom should you trust with prenatal care? There’s no single answer. Obstetricians, midwives, family doctors, or collaborative teams all offer distinct strengths. Obstetricians are equipped for complex presentations; midwives blend medical oversight with individualized, holistic care for low-risk pregnancies. Family doctors may offer continuity before, during, and after birth, familiar with your entire health history.
Practicalities count too—clinic hours, location, staff friendliness, and hospital affiliations. It’s prudent to ask about their management style, approach to mental health, and available support for partners. Feeling listened to, respected, and able to ask “awkward” questions—these factors are as important as technical prowess. Select the care pathway where you feel understood and supported.
Harnessing Community and Resources: Building Your Support Network
Good prenatal care is strengthened by community. Peer support groups, prenatal education classes, workshops, and curated online platforms all extend your network. Group care models, in which checkups are paired with guided discussion, foster both clinical monitoring and shared experience. Involvement of partners and extended family—attendance at classes, sharing daily responsibilities, or learning more about healthy pregnancy—amplifies emotional well-being.
Helpful support can be as simple as a meal cooked, a ride to an appointment, or encouragement during challenging moments. The overarching message: asking for—and accepting—help creates a more sustainable pregnancy journey.
Removing Barriers to Prenatal Care: Pathways to Equity
Unfortunately, not everyone has equal access to prenatal care. Transportation difficulties, lack of insurance coverage, language barriers or cultural differences—these can block timely medical supervision. Solutions are evolving: telemedicine (video appointments and remote monitoring), low-cost or walk-in clinics, broad-reaching public health initiatives, and translated educational materials all make a difference for communities underserved by traditional models.
Efforts to offer flexible scheduling, on-site childcare, and culturally sensitive practices recognize the diversity of parent experiences and improve health outcomes. Support exists—sometimes, it simply needs to be discovered or requested.
The Postnatal Chapter: Continuing Care After Birth
Postnatal checkups are not to be overlooked—monitoring recovery, emotional adjustment, breastfeeding support, and early detection of postpartum complications save lives and ease transitions. Newborns require vigilant checks for weight, feeding, and developmental progress, each woven with guidance for parents as they settle into their new roles.
Providers are trained to screen for postpartum depression and provide referral to mental health professionals when needed. Conversations about contraception and future pregnancies are also typically included, laying groundwork for holistic family well-being. Through consistent postnatal care, the circle of support begun in pregnancy continues seamlessly beyond birth.
Key Takeaways
- Prenatal care is the foundation for a healthy, managed pregnancy—melding prevention, screening, and education.
- Early and regular visits offer protection through the detection of pregnancy concerns and introduce expert intervention before issues escalate.
- Nutrition, lifestyle, and attention to mental health impact both immediate well-being and long-term outcomes for parent and baby.
- Families thrive with supportive, involved partners and informed loved ones, making use of resources and educational programs.
- Equal access, enhanced by telemedicine and flexible services, bridges gaps and supports health equity for every parent-to-be.
- Postnatal care is essential for ongoing maternal and neonatal health—recovery, mental health, feeding, and planning ahead.
- Resources are available, and dedicated professionals are ready to walk this road with you. For ongoing support, tailored health guidance, and free health questionnaires for your child, download the Heloa app.
The journey of pregnancy invites questions, challenges, and transformation—prenatal care is your partner every step of the way.
Questions Parents Ask
What can I do if I can’t make it to all my prenatal appointments?
Unexpected events, work schedules, or transportation difficulties can sometimes make it challenging to attend every appointment. If you miss a visit, don’t worry—reach out to your healthcare provider as soon as possible. They are generally understanding, especially if you communicate your situation. Some clinics can offer flexible hours, reschedule at your convenience, or set up telemedicine sessions. It’s always better to let your care team know about any issues early on so that they can support you and ensure you receive the follow-up and attention you and your baby deserve.
Are there different types of prenatal care?
Yes, prenatal care isn’t a one-size-fits-all experience. In addition to traditional individual check-ups, some parents may participate in group prenatal visits, where parents share experiences and receive education in a supportive setting. Others may benefit from specialized care, such as high-risk pregnancy management, additional screenings, or consultations with nutritionists or mental health professionals. Each approach is adapted to your medical history, preferences, and any unique needs that might arise during pregnancy.
How does prenatal care support emotional wellbeing during pregnancy?
Prenatal care values emotional wellness just as much as physical health. Many care providers now routinely discuss stress, emotional shifts, and mental health as part of each visit. Practical strategies—like guided relaxation, mindfulness tips, or referrals to counseling—can be suggested if needed. If you ever feel overwhelmed, anxious, or just need to talk, you can always bring up these feelings during your appointments. You are not alone in what you’re experiencing; every feeling is valid, and supportive resources exist to help you navigate this journey in the most reassuring way possible.
Further reading: