Chickenpox pregnancy—it’s a phrase that can set off a whirlwind of questions in the mind of any expectant parent. Worries about vulnerability, potential dangers for the unborn child, and the unpredictable paths of infection often intermingle with feelings of uncertainty. What does it mean to face chickenpox pregnancy when immunity status is unclear? Is there a way to shield the baby or at least soften any blow? These are not just theoretical questions; they demand real answers, grounded in science but layered with empathy. In this in-depth overview, you’ll find perspectives on root causes, risks, care, testing, and prevention—crafted not for a medical textbook, but for parents who simply want to do the best for their growing family.
Let’s illuminate the path step by step—unpacking transmission, tracing the clinical journey, highlighting advanced medical advice, and offering practical, parent-facing strategies. Far from a simple infection, chickenpox pregnancy can unfold with a surprising range of consequences—sometimes mild, occasionally severe. Above all, knowledge remains your ally.
What Is Chickenpox Pregnancy and Why Does It Matter?
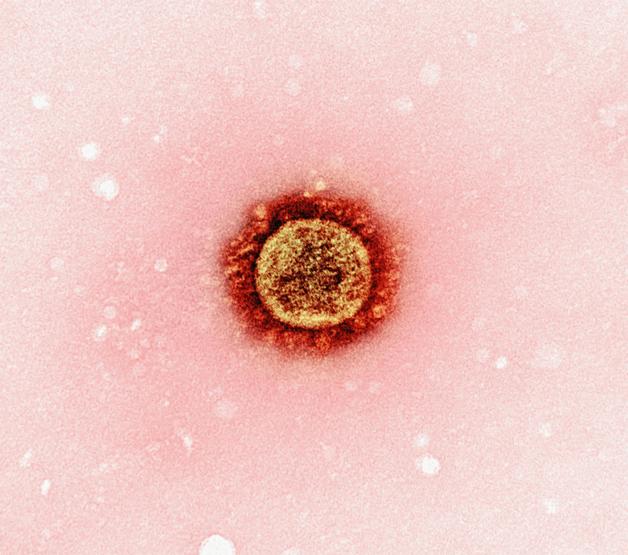
What exactly makes chickenpox during pregnancy such a point of concern? The answer lies partly in its stealthy nature and partly in the stakes involved. The varicella-zoster virus (VZV)—that’s the germ behind chickenpox—is notorious for high contagion. It finds its way through coughs, sneezes, or even direct contact with the ooze from those classic, fluid-filled blisters. What might seem a simple “childhood illness” can suddenly look quite different during pregnancy.
Pregnancy shifts the body’s immune landscape. Immunity that once shrugged off minor ailments now acts more cautiously, affecting both mother and fetus. Whether one is immune (thanks to earlier infection or vaccination) or completely inexperienced with this virus—the difference shapes every aspect of the story.
Wondering how long the risk lasts? For those experiencing chickenpox pregnancy, contagiousness starts 1–2 days before the rash is visible and only ends once all blisters have crusted. Each stage brings its own questions and points of vigilance.
Who Is at Risk? Causes and Pathways of Exposure
Let’s draw a quick timeline. Childhood—most people catch chickenpox, recover, and carry lifelong antibodies. But what if that infection never happened, or no vaccine was given? That’s where chickenpox pregnancy concerns become real.
The main suspects:
- Never having had chickenpox or the vaccine (often called being seronegative)
- Regular contact with school-aged children, especially in daycares or teaching environments
- Regional factors: Certain areas see much lower childhood infection rates or have patchy vaccine coverage, leading to more at-risk adults
A single encounter—a shared office, a crowded bus, a family visit—can be all it takes. And because memories of childhood illnesses grow fuzzy, a quick blood test for VZV antibodies provides real clarity on immune status.
But why such urgency? During chickenpox pregnancy, risks are magnified. Not just due to a mother’s health, but because timing shapes the impact on the growing fetus as well.
Chickenpox Pregnancy: How to Recognise and React
Aches, malaise, fever, a sense that “something is brewing”—these are the subtle hints. Suddenly, an itchy, red-spotted rash bursts forth—tiny red marks transform into classic blisters, ready to form a map across the body. This rash, with its burning itchiness and clustered appearance, is the telltale sign.
For some, symptoms remain moderate—just a few scattered spots, perhaps a gentle fever. For others—especially in chickenpox pregnancy—the reaction can be much more intense, with widespread lesions and a more unsettled general state. Timing, too, plays a powerful role: early-pregnancy infections differ sharply from those occurring closer to delivery.
Medical Risks: Effects on Mother and Baby
For the Expectant Mother
Chickenpox pregnancy introduces risks rarely seen in children. Adults—even more so, pregnant adults—face steeper odds of facing problems like varicella pneumonia. Picture a persistent cough, breath not coming so easily, and a need for hospital-level support—these are not rare stories. Certain triggers—especially the final months of pregnancy, pre-existing breathing issues, or smoking—can tip the scales even further.
Complications don’t stop there. Hepatitis (liver trouble) and encephalitis (brain inflammation), while rare, are documented risks. Each complication raises the level of concern but also opens the door to proactive management.
For the Unborn or Newborn Baby
Here, timing is everything:
- First 20 weeks: A delicate period. Chickenpox pregnancy at this point can, albeit very rarely (1–3%), lead to congenital varicella syndrome—which might involve skin scars, limb deformities, or nervous system troubles. This risk, though small, looms large due to the long-lasting nature of the possible effects.
- 20 weeks onwards: The odds of birth defects wane, but a hidden risk remains—the virus can “sleep” in the baby’s nerves, eventually causing shingles later in life.
- Near birth (from five days before to two days after delivery): The most dangerous window. Without enough passed-on antibodies, the newborn faces neonatal varicella—a potentially severe infection requiring urgent, advanced medical care.
Across all stages, severe chickenpox in the mother can trigger preterm labour or growth concerns for the baby.
Diagnosis and Clinical Pathways
Spotting chickenpox pregnancy usually comes down to the classic rash—clusters of irritated, liquid-filled blisters on reddened skin. Sometimes, though, stories from childhood get muddled or forgotten. That’s when VZV antibody blood tests (serology) shine—offering a concrete yes/no on real immunity.
Once infection is established, ultrasound tracking becomes vital. Early- or mid-pregnancy cases require close observation for signs like slowed growth or subtle limb and brain changes. In rare uncertainties—complex ultrasound findings, for example—special tests on amniotic fluid (amniocentesis with PCR) can look for viral DNA.
Doctors balance ongoing, sensitive care with close, technical surveillance—keeping one attentive eye on both physical changes and parental peace of mind.
Treatment Strategies: Mother, Fetus, and Newborn
For confirmed chickenpox pregnancy, immediate treatment is preferred. Acyclovir or valacyclovir are the standard antiviral solutions, taken as soon as possible to lower complication risks and speed healing. Most take valacyclovir three times daily for a week, but severe lung trouble (varicella pneumonia) warrants intravenous acyclovir and close hospital monitoring.
If a non-immune pregnant woman faces a high-risk exposure but has not yet shown signs, timely administration of specific immune globulins (VZIG) within 10 days offers strong extra defence. For late recognition or unavailability, preventive antivirals fill the gap.
When infection strikes near delivery, direct care for the baby becomes central: giving immune globulins or acyclovir rapidly—and placing the newborn under watchful isolation—offers the best protection.
A note that might surprise: breastfeeding is encouraged, even during chickenpox pregnancy. Maternal antibodies flow through the milk, helping the baby’s immune system. Hygiene is the keyword—careful handwashing, avoidance of feeding directly from blistered skin, and possibly masks safeguard everyone involved.
Vaccination, Prevention and Everyday Habits
Worried about chickenpox pregnancy in the first place? Quick solution: preconception vaccination tops every list of proactive steps. For those planning, checking VZV antibody status (simple bloodwork) beforehand removes doubt. If no immunity is found, two shots of the live attenuated chickenpox vaccine (like Varilrix® or Varivax®), at least a month apart, build protection. Remember—no vaccination during pregnancy; only afterwards or in advance.
During community outbreaks, or if you’re unsure about a recent exposure, extra vigilance matters. Limit contact with sick or unvaccinated individuals. For pregnant teachers or caregivers, early information-sharing at work makes a difference.
Don’t ignore a suspected exposure. Immediate medical advice, prompt antibody testing, and—where needed—quick VZIG or antiviral therapy build a powerful response.
Practical Guidance for Parents
- Act promptly if exposed—don’t hesitate; speed is protection.
- Isolate any infected family member, especially around babies and those with weak immunity.
- Stick to robust hygiene—wash hands, use masks if there are face or chest blisters, and keep a clean environment.
- If worried about immunity, get a blood test without delay.
- Vaccinate close contacts where possible.
- Follow up regularly with healthcare professionals, especially for ongoing pregnancy surveillance.
- Encourage gentle, factual discussion at home—reassurance helps families process worries and make positive plans.
No two paths are identical. Some parents find their worries quickly put to rest by negative blood tests; others navigate intense monitoring with courage. In either case, solidarity with experienced healthcare teams—plus steady, evidence-based information—maximises safety.
Clinical Care Steps and Breastfeeding Advice
Healthcare teams generally check chickenpox immunity during the first consultation. For unexpected exposures, VZIG is offered as soon as possible, reducing infection intensity. If chickenpox develops, starting antivirals rapidly is the key. For mothers hit by severe chickenpox pregnancy—especially lung or brain issues—hospital care combines specialist support and fetal monitoring.
If the infection comes right before or after birth, newborn care may mean neonatal intensive care, close isolation, and treatment with immune globulins or IV acyclovir.
Breastfeeding isn’t halted, unless blisters are present on the breast. In those cases, milk can be expressed and offered safely until healing completes—ideal for maintaining nutrition and immunity transmission.
A final note on prevention: mother’s milk isn’t enough alone to defend an exposed infant. Babies in direct risk situations always benefit from additional immune globulin and vigilant observation.
Key Takeaways
- Chickenpox pregnancy demands consistent attention. Diagnosis, proactive prevention, and vigilant monitoring dramatically influence outcomes for both mother and infant.
- Knowing immune status through serology testing, practicing preconception vaccination, and prompt post-exposure action offer the best lines of defence.
- Antivirals and immunoglobulins significantly improve the health trajectory in confirmed cases. Early action is always best.
- Psychological relief flows from clear, medical information—so regular communication with caring professionals is invaluable.
- Breastfeeding remains safe and recommended (with hygiene), supporting both rapid recovery and ongoing well-being.
- For extra guidance, practical advice, and health monitoring, explore the Heloa app for free child health questionnaires and personalised tips.
- Each chickenpox pregnancy journey is unique—dedicated resources and skilled professionals are available every step of the way.
Questions Parents Ask
Can chickenpox happen during pregnancy if I already had it as a child?
If you’ve previously had chickenpox, your immunity usually remains complete for life. Catching the virus again is quite rare. Unsure about your previous infection? One blood test can check your immunity, giving you clarity and peace of mind. Always consult your obstetrician for reassurance or step-by-step guidance if uncertain.
What should I do if I was exposed to chickenpox during pregnancy and I never had it before?
If you know (or strongly suspect) you’ve never had chickenpox or the vaccine, rapid action is important after exposure. Let your doctor know immediately—timely VZIG administration can lower the severity of infection dramatically. Even if no symptoms have appeared, do not delay seeking advice; medical options are most effective when applied early.
Is there any risk to my baby if I catch chickenpox early in pregnancy?
Unfortunately, chickenpox within the first half of pregnancy does hold a small risk for the fetus—mainly congenital varicella syndrome, with skin, limb, and sometimes neurodevelopmental concerns. These cases are very rare, but careful monitoring is well established. Your healthcare team will likely schedule regular ultrasounds and check-ins to monitor your baby’s development closely and discuss each step openly.
Further reading: