A preemie can arrive earlier than expected, and suddenly parenting is full of monitors, medical terms, and waiting. Will breathing settle? Why does feeding take so long? When can you finally take your baby home? These worries are normal, especially when your newborn looks so small and yet is doing such a big job: growing outside the womb.
What “preemie” means
A preemie is a baby born before 37 completed weeks of pregnancy. Doctors calculate gestational age from the first day of the last menstrual period and confirm it with ultrasound.
Being born early can affect how ready a baby is to breathe, feed, keep warm, and fight infection. Even one extra week in the uterus may improve lung maturity and feeding stamina.
You may also hear:
- Preterm: the medical term for a baby born early
- Postmenstrual age (PMA): gestational age at birth + weeks since birth
- Term-equivalent age: around 40 weeks PMA
Preterm, low birth weight, SGA: different labels
- Preterm: <37 weeks
- Low birth weight (LBW): <2,500 g
- Very low birth weight (VLBW): <1,500 g
- Extremely low birth weight (ELBW): <1,000 g
- Small for gestational age (SGA): <10th percentile for that gestational age
A baby can be a preemie and not SGA (small mainly because of early birth). A baby can be term and still SGA (growth restriction in pregnancy).
Gestational age groups: what they can suggest
Clinicians group prematurity to plan monitoring and the right level of newborn care:
- Moderate preterm: 32–36 weeks
- Very preterm: 28–31 weeks
- Extremely preterm: <28 weeks
These categories help predict common needs, not your child’s future.
Extremely preterm
An extremely preterm preemie often needs CPAP or ventilation, an incubator for temperature control, and gradual nutrition starting with IV nutrition (TPN) and then tube feeds. Monitoring is close for lung disease, infection, gut problems, and brain/eye development.
Very preterm
A preemie born between 28 and 31 weeks may still have apnoea (breathing pauses) and bradycardia (slow heart rate), requiring monitors and sometimes caffeine citrate. Feeding often begins via tube and shifts to breast/bottle as coordination improves.
Moderate to late preterm
Babies after 32 weeks can still have jaundice, low blood sugar (hypoglycaemia), temperature instability, and feeding fatigue. Some need NICU observation mainly for monitoring and feeding support.
Viability thresholds
Around 22–24 weeks, survival can sometimes be possible, but uncertainty is higher. Decisions depend on the full clinical picture and discussion with parents.
Why a baby is born early
Spontaneous preterm labour and PPROM
Labour can start early on its own. PPROM (preterm premature rupture of membranes) means the waters break early. Triggers can include infection/inflammation, a cervix that shortens early, uterine stretching (twins/triplets), or previous preterm birth.
Medically indicated early delivery
Sometimes early delivery is safer than continuing pregnancy:
- Maternal: severe hypertension, preeclampsia, serious infection
- Placental: abruption, placenta previa with bleeding, placental insufficiency
- Fetal: growth restriction with concerning tests, fetal distress
Risk factors seen in practice
Multiples, IVF pregnancies, short cervix/cervical insufficiency, UTIs and genital infections, diabetes, thyroid disease, kidney disease, and placental problems can increase risk. In India, gaps in antenatal care, anaemia, nutrition challenges, and air pollution exposure may also contribute.
Signs of preterm labour: when to seek urgent review
Before 37 weeks, contact your maternity team or go to triage if you notice:
- regular contractions that continue
- pelvic pressure, cramps, or persistent back pain
- a gush or trickle of fluid
- vaginal bleeding or sudden discharge change
- clear decrease in fetal movements
What evaluation can include
Monitoring contractions and fetal heart rate, checking the cervix, transvaginal cervical length ultrasound, fetal fibronectin (fFN) in selected cases, and urine/blood tests.
Treatments that may be offered
Depending on gestational age and findings:
- Tocolytics (short-term slowing of contractions)
- Antenatal corticosteroids for lung maturation
- Magnesium sulphate for neuroprotection (often before 32 weeks)
- Antibiotics for PPROM or suspected infection
- GBS prophylaxis during labour when indicated
Transfer before birth to a higher-level NICU may be suggested if very preterm birth is likely.
Early health issues in a preemie after birth
Breathing and oxygen needs
Immature lungs can cause respiratory distress syndrome (RDS) due to low surfactant. Support may include oxygen, HFNC, CPAP, or ventilation, surfactant therapy may be used.
Apnoea and bradycardia
Monitors track episodes. Caffeine citrate is commonly used.
Temperature, jaundice, sugar, anaemia
A preemie loses heat quickly (thin skin, low fat), so incubators help. Jaundice may need phototherapy. Hypoglycaemia may need feeds or IV glucose. Anaemia of prematurity may require iron and sometimes transfusion.
Infection risk
Immature immunity plus IV lines increases sepsis risk. Hand hygiene in the hospital and at home remains one of the strongest protections.
Feeding challenges
A preemie may not yet coordinate suck–swallow–breathe. Tube feeds are common initially. Reflux-like symptoms often improve with pacing, positioning, and time.
What happens in the NICU
NICU teams can include neonatologists, nurses, respiratory therapists, pharmacists, dietitians, lactation consultants, and PT/OT/feeding therapists.
Monitoring may include heart rate, breathing, oxygen saturation, glucose, electrolytes, bilirubin, blood counts, cultures, X-rays, echocardiogram, and cranial ultrasound when indicated.
Many units use developmental care: dim light, less noise, contained positioning, clustered care to protect sleep.
Feeding a preemie: milk, fortifiers, formula
A preemie typically needs higher calories, protein, calcium, and phosphorus than a term baby.
Feeding may start with TPN, then tiny trophic feeds through an NG/OG tube, then gradual increases.
Breast milk supports gut health and is linked with lower NEC risk. Donor milk may be used when available. Fortifiers are often added to expressed milk to support growth and bone mineralisation.
When breast milk is not sufficient, preterm formula or higher-calorie feeds may be used. After discharge, iron and vitamin D are commonly prescribed—follow your hospital plan.
Bonding and development
Kangaroo care
Skin-to-skin care can support temperature stability, steadier breathing, calmer sleep, and breastfeeding.
Safety basics:
- start only when staff say it is safe that day
- keep the airway clear (upright position)
- ask for help with tubes/lines
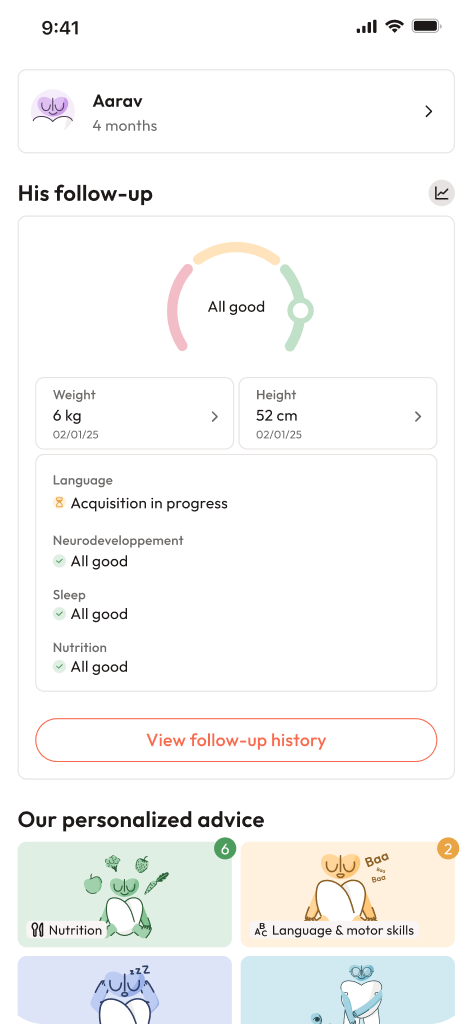
Corrected age and milestones
Corrected age = chronological age minus weeks born early. It helps track milestones fairly, often until about 2 years. Progress over time matters more than single dates.
Tummy time (when awake and supervised) supports neck strength and can reduce plagiocephaly. If the head always turns one way, ask about torticollis and early physiotherapy.
Going home and follow-up
NICU discharge usually needs stable temperature in an open crib, stable breathing (with home oxygen plan if needed), safe feeding with steady weight gain, and a clear medicines plan.
Many preterm babies undergo a car seat tolerance test before discharge.
At home, safe sleep remains: Alone, on the Back, in a Crib.
Follow-up clinics track growth, feeding, vision (ROP if needed), hearing, and development. Early intervention (PT/OT/feeding therapy) can make day-to-day care easier and support progress.
Family well-being
NICU stress can show up as insomnia, irritability, sadness, or replaying frightening moments. If these feelings persist, speak with your doctor or the hospital support team.
At a glance: essentials for parents
- A preemie is born before 37 weeks.
- Prematurity groups guide care needs, not future potential.
- Signs of preterm labour deserve prompt assessment.
- NICU care focuses on breathing, warmth, nutrition, infection prevention, comfort, and development.
- Feeding a preemie often needs tube support at first, fortification and supplements are common.
- Corrected age helps milestone tracking in early years.
- Support exists after discharge, you can also download the Heloa app for personalised advice and free child health questionnaires.

Further reading:
- Premature birth – Symptoms and causes: https://www.mayoclinic.org/diseases-conditions/premature-birth/symptoms-causes/syc-20376730
- Preemie: https://www.healthychildren.org/English/ages-stages/baby/preemie/Pages/default.aspx