A child sleeps peacefully… then suddenly wakes up with a loud, seal-like cough, a hoarse cry, and noisy breathing that feels far too dramatic for “just a cold”. That scenario is classic croup. It can be frightening, yes, but most croup episodes are viral, short-lived, and respond very well to a single dose of steroid medicine when needed—plus calm, sensible home care.
So what matters most tonight: is this mild croup you can watch, or the kind that needs urgent help? Why does it spike after midnight? What treatments are commonly used by clinicians in India? Let’s put clarity back into the room.
Understanding croup and why it sounds scary
Croup is inflammation of the upper airway—mainly the larynx (voice box) and trachea (windpipe). Inflammation is the immune system at work: cells arrive, fluid leaks into tissues, and swelling (oedema) narrows the airway.
In small children, the tightest part is just below the vocal cords, the subglottic region. Swelling there can reduce airflow quickly. That is why croup sounds dramatic even when oxygen levels may still be normal.
Barking cough and stridor: what those sounds mean
- The bark happens when air is forced through swollen tissues around the vocal cords.
- Inspiratory stridor is the high-pitched sound on breathing in. It reflects narrowing in the upper airway.
Stridor often gets louder when a child is crying, because breathing becomes faster and more forceful. Calm is not only comfort, it is part of symptom control.
Why nights are often worse
Several factors can make croup look louder at night:
- Lying down can increase secretion pooling.
- AC/fans can dry the throat.
- Tired children cope less well.
Who gets croup most often
Croup is common under 5 years, especially between 6 months and 3–5 years.
Mild, moderate, severe: a quick snapshot
- Mild: barking cough, no stridor at rest, minimal effort, drinking okay.
- Moderate: stridor at rest, visible retractions, increased effort.
- Severe: marked distress, poor air movement, tiring breathing, trouble drinking, or signs of low oxygen.
Types of croup
Viral croup often follows a cold: runny nose, congestion, mild fever, then a barky cough and hoarseness. Stridor may appear at night.
Spasmodic croup
Spasmodic croup can start suddenly at night, often with little fever and minimal cold symptoms. It may recur. Some families notice triggers such as smoke, perfumes, dust, or reflux symptoms.
Laryngotracheobronchitis in simple words
This medical term means inflammation of the larynx and trachea (sometimes extending to larger bronchi). It is commonly used for typical viral croup.
Causes and risk factors
Most croup is viral. Parainfluenza virus is the most common cause, but RSV, influenza, and SARS-CoV-2 can also trigger it.
Risk factors that increase chances or severity:
- age under 5 years,
- cooler-season viral circulation,
- daycare/school exposure and siblings,
- smoke exposure (including passive smoking),
- pollution, strong fragrances, harsh cleaning sprays, dry indoor air.
When bacteria are a concern
Bacterial causes are uncommon but can be more severe (for example bacterial tracheitis). Clinicians worry more if a child looks very ill, has high fever, worsens rapidly, or does not respond as expected to usual croup treatment.
How croup spreads
Viruses causing croup spread via droplets and contaminated hands/surfaces.
Practical steps:
- Wash hands after wiping noses.
- Avoid sharing bottles, cups, spoons, towels.
- Clean high-touch surfaces and toys.
- Keep your child home until fever-free for 24 hours (without fever medicine) and breathing is comfortable.
Symptoms to recognise early
The classic pattern of croup includes:
- barking cough,
- hoarse voice or hoarse cry,
- stridor (especially at night).
Breathing effort: what to look for
Seek medical help if you see:
- retractions (pulling in at the ribs or base of the neck),
- nasal flaring,
- very fast breathing or pauses,
- a child who struggles to breathe in.
Hydration clues
If breathing effort is high, drinking drops. Watch urine output/wet nappies, tears, saliva, and alertness.
How long croup lasts
Most children improve in 3–5 days. After a steroid dose, noisy breathing often improves within hours and is clearly better in 24–48 hours, though a mild cough can linger.
When to get urgent help or emergency care
Seek urgent assessment if:
- stridor happens while your child is calm,
- breathing looks laboured or fast and does not settle,
- retractions or nasal flaring appear,
- drinking becomes difficult.
Go to emergency care immediately if:
- lips/face look blue or grey,
- your child is very sleepy, floppy, difficult to wake, or exhausted,
- there is drooling with distress or trouble swallowing,
- symptoms started after a choking event.
A note on epiglottitis
Epiglottitis is uncommon where Hib vaccination is routine, but it is an emergency: high fever, severe throat pain, drooling, difficulty swallowing, and a very ill child leaning forward to breathe (often without the barking cough).
How doctors diagnose croup
Croup is usually diagnosed clinically: history plus exam. Pulse oximetry may be used to check oxygen saturation.
X-rays are not routine. They may be considered if symptoms are atypical or response is poor. The “steeple sign” can appear, but its absence does not rule croup out.
Conditions that can mimic croup
Clinicians may consider:
- foreign body aspiration (sudden onset after choking),
- bacterial tracheitis (high fever, very ill appearance),
- anaphylaxis/angioedema (hives, facial swelling, sudden breathing difficulty),
- deep neck infections (neck pain/swelling, drooling),
- bronchiolitis/asthma (wheeze dominates),
- pertussis (prolonged coughing fits),
- structural airway issues if episodes are frequent or outside the usual age range.
Home care for mild croup
Hold your child upright, keep the environment quiet, and reduce crying. Less distress often means less stridor.
Fluids and fever comfort
Offer small, frequent sips (water, ORS, milk, warm soups). For fever or throat pain, use paracetamol/acetaminophen or ibuprofen at the correct dose for age and weight. Avoid aspirin.
Nasal care
Saline drops/spray can help if the nose is blocked, especially for babies who struggle to feed when congested.
Cool air or humidified air
Some families find comfort with cool air or a humidifier, though evidence is mixed.
- Avoid hot steam (burn risk).
- Keep humidifiers clean to prevent mould.
Honey (only over 1 year)
For children older than 12 months, honey may soothe coughing. Do not give honey under 1 year.
What to avoid
Avoid smoke, strong fragrances, and OTC cough syrups for young children.
A simple night plan
- Pick your child up and keep them upright.
- Check whether stridor is only when crying or also at rest.
- Look for retractions and nasal flaring.
- Offer small sips if swallowing is easy.
If stridor persists at rest or breathing effort increases, seek urgent care.
Medical treatment for croup
A single dose of dexamethasone reduces airway swelling in croup. Improvement often begins within 2–6 hours and lasts 24–72 hours.
Nebulised budesonide
Nebulised budesonide may be used when oral medicine is difficult.
Nebulised epinephrine
Nebulised epinephrine is used for moderate to severe croup with stridor at rest. It works quickly, but the effect can wear off within a few hours, so observation is needed.
When hospital admission is needed
Admission may be advised for persistent stridor at rest, repeated epinephrine needs, low oxygen levels, dehydration, very young infants, or significant underlying medical conditions.
Antibiotics do not treat viral croup. They are reserved for suspected bacterial infection.
Prevention and recurrent croup
Hand hygiene, vaccination (influenza, COVID-19, Hib), and avoiding smoke/irritants can reduce risk.
If croup is recurrent (often three or more episodes in a year), unusually severe, starts under 6 months, or continues beyond 5–6 years, clinicians may evaluate for airway anatomy, reflux (GERD), or atopy.
Key takeaways
- croup is upper-airway inflammation, subglottic swelling is why the sound is dramatic.
- Mild croup can often be supported at home with calm, upright positioning and fluids.
- Stridor at rest, retractions, nasal flaring, colour change, exhaustion, or poor drinking need urgent assessment.
- Dexamethasone often improves croup within hours, nebulised epinephrine is for more severe episodes with observation.
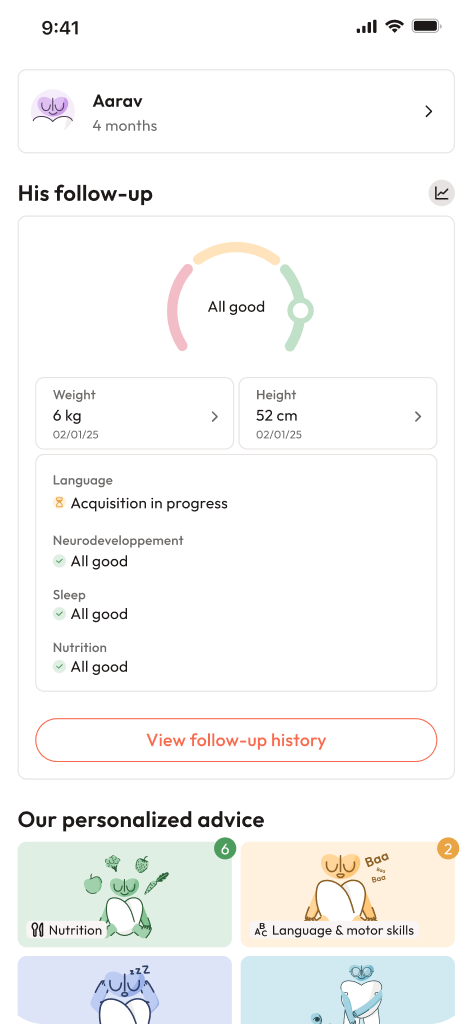
- Support is available: if you would like personalised guidance and free child health questionnaires, you can download the Heloa app.

Further reading:
- Croup – Symptoms & causes: https://www.mayoclinic.org/diseases-conditions/croup/symptoms-causes/syc-20350348
- Croup – Diagnosis & treatment: https://www.mayoclinic.org/diseases-conditions/croup/diagnosis-treatment/drc-20350354
- Croup – StatPearls – NCBI Bookshelf: https://www.ncbi.nlm.nih.gov/books/NBK431070/