Pregnancy—a time glowing with anticipation, peppered sometimes with just as much apprehension. Among the many questions that ripple through parents’ minds, gestational diabetes carves its own space: Will it disrupt the joyful experience? What does it mean for your child, for your own health now and later? Facing this diagnosis or even just a risk can stir up a unique blend of anxiety, confusion, and urgency. But take a breath. Let’s untangle the science, the risks, and the support available, so you can step forward with calm, confident steps. From what sets gestational diabetes apart from other forms, to the rhythms of daily care—even the intricate details of blood sugar monitoring and dietary choices—every aspect will be addressed with factual clarity and empathy.
Understanding Gestational Diabetes and Glycosuria in Pregnancy
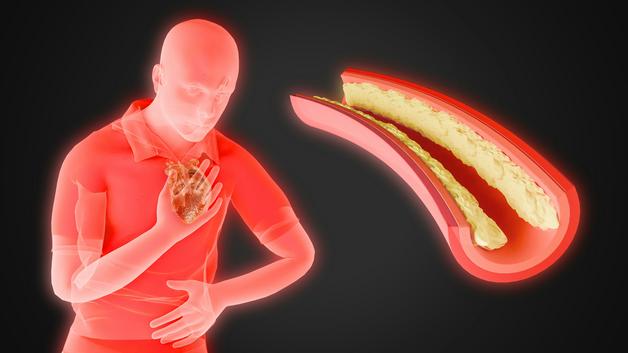
Imagine the body as a finely tuned symphony, each hormone contributing its note. Yet, pregnancy introduces entirely new instruments—placental lactogen, progesterone, oestrogen, and cortisol—each tweaking how you process sugar. With these changes, your body becomes more “insulin resistant.” The pancreas, ever the diligent conductor, tries to ramp up insulin production to maintain harmony, but sometimes, the effort falls a little short, and suddenly, glucose levels begin to rise. That’s the core of gestational diabetes.
Yet, a curious phenomenon: as the kidneys become a bit less effective at keeping glucose in the bloodstream, some sugar sneaks into the urine—this is what healthcare professionals call glycosuria. An occasional finding? Often simply physiological, no cause for alarm. But persistent sugar in the urine, especially if it appears alongside high blood glucose, sends a clear signal—further testing and careful follow-up are needed, as this could be an early sign of gestational diabetes.
Causes and Risk Factors for Gestational Diabetes
Why does gestational diabetes happen? The answer is multi-layered, like a well-spiced curry. Beyond the hormonal surges sits a landscape of personal and family traits:
- Maternal age over 25 years: Risk gradually increases with age.
- Overweight or obesity: More fat tissue equals more insulin resistance.
- Family history of diabetes: Genetics sometimes whispers loud.
- Ethnic background: South Asian descent, among others, faces a higher predisposition.
- Personal history: Previous pregnancies with gestational diabetes or multiple occasions of glycosuria make recurrence more likely.
- Polycystic ovary syndrome (PCOS): This metabolic condition raises baseline risk.
Tallying up risk factors isn’t meant to worry—it empowers you and your healthcare team to plan early screening and proactive support, rather than rushing at the last moment.
Recognising Symptoms and the Importance of Routine Checks
Perhaps the most confounding aspect: gestational diabetes often lurks quietly. No dramatic symptoms, no glaring warning signs. Occasionally, thirst, frequent urination, vague fatigue, or slightly blurred vision may emerge, but these shadow ordinary pregnancy effects. Relying only on symptoms? Not advisable.
Instead, routine—almost ritualistic—screenings become the parents’ best ally. Urine dipsticks during prenatal check-ups often detect sugar in urine; more of a red flag than a diagnosis. If persistent glycosuria or other risk features appear, blood glucose tests step into focus. It’s a stepwise approach, designed for catch and confirmation, not panic.
Screening and Diagnosis: Methods for Clarity
Timing matters. Typical screening for gestational diabetes occurs between the 24th and 28th week, but those with risk factors might begin even earlier. What does the pathway look like?
- Step 1: Urine glucose test: A quick test, generally over within seconds. If values soar beyond 15 mg/dL (0.15 g/L), especially more than once, it nudges the care team to probe deeper.
- Step 2: Blood glucose checks and Oral Glucose Tolerance Test (OGTT):
- Fasting blood sugar offers a baseline; a value of ≥92 mg/dL merits attention.
- For further clarity, the OGTT is administered—a measured challenge for the body’s sugar-regulating machinery. After a sugar solution, blood is tested at fasting, 1 hour, and 2 hours: if any results cross the diagnostic thresholds (92 mg/dL fasting, 180 mg/dL at 1 hour, 153 mg/dL at 2 hours), gestational diabetes is diagnosed.
- Some situations call for a 100g, two-step test, though protocols vary.
This blend of urine and blood assessments is what distinguishes passing, harmless glycosuria from genuine, attention-requiring gestational diabetes.
Impact on Mother and Baby: Short- and Long-Term Effects
The canvas of gestational diabetes stretches wide, touching both parents and babies—sometimes in subtle brushstrokes, sometimes in bolder hues.
Risks for Mothers:
- Short-term: Elevated chance of pregnancy-induced hypertension, preeclampsia, need for caesarean section, and infections.
- Long-term: The shadow of type 2 diabetes looms, along with the possibility of metabolic problems in later years.
Risks for the Baby:
- Macrosomia: Babies grow larger than usual, heightening the risk of tough deliveries or shoulder dystocia.
- Neonatal complications: Preterm birth, respiratory distress, and even neonatal hypoglycemia (dangerously low blood sugar soon after birth).
- Long-term: Exposure in the womb to high glucose can make children more likely to face weight issues, glucose intolerance, or metabolic challenges later in life.
But here’s the uplifting truth: With careful monitoring, regular checkups, and lifestyle tweaks, most of these potential troubles can be far lessened—sometimes avoided entirely.
Managing Gestational Diabetes: Strategies for Parents
Daily life need not be turned upside down. Here’s what science and experience recommend:
1. Diet and Nutrition
- Picture the plate: array of vegetables, pulses, whole grains (brown rice, chapati with whole wheat), fresh fruits in moderation, and proteins like fish or paneer.
- Smaller, regular meals help to flatten out blood sugar peaks and valleys.
- Curb the temptation of refined sugars, pastries, and highly processed foods.
- Hydration? Simple—water, sipped throughout the day.
2. Physical Activity
- Gentle movement is a reliable ally. Walking, swimming, or prenatal yoga—thrice a week, 30 minutes if possible—each session nudges glucose levels in the right direction.
3. Blood Glucose Monitoring
- A small, manageable ritual at home. The glucometer offers feedback, both building confidence and providing your care team with valuable insight.
4. Medication
- When food and movement aren’t enough, prescribed insulin (and rarely, oral medications) can be added—carefully tailored, and proven safe for mother and baby.
5. Personalised Teamwork
- Collaboration is everything. Obstetricians, midwives, dieticians, endocrinologists—they come together to build a support network, tuning care to unique situations.
6. Monitoring the Baby
- Regular scans, check-ups, sometimes extra fetal monitoring—each point of contact adds a level of reassurance.
Preventing Gestational Diabetes and Its Consequences
Preparation begins long before delivery day.
Before and during pregnancy:
- Manage weight with balanced eating and regular physical activity.
- Choose fibre-rich options (dal, legumes, millets); minimize processed sugar and saturated fats.
- Assess risk early with your medical team—especially previous gestational diabetes, family tendency, or PCOS.
During pregnancy:
- Consistent antenatal follow-up sharpens early detection. Multiple gestations or early signs prompt tailored surveillance.
Every prompt, positive adjustment—however small—builds a safer path for parent and child alike.
Life After Pregnancy: Staying Healthy for Years Ahead
Gestational diabetes rarely lingers after birth, but its imprint can keep you vigilant.
- Postpartum screening: Routine OGTT or fasting glucose sampling around 4–12 weeks after delivery, then at regular intervals.
- Breastfeeding: More than nourishment for baby. It nudges maternal blood sugar toward stability and helps shed pregnancy weight.
- Lifestyle choices: Healthy eating and moderate physical activity reduce the future risk of type 2 diabetes—for parent and child both.
Good habits started now can ripple forward, shaping a lifetime of better health outcomes.
Coping Emotionally: Finding Balance and Support
Gestational diabetes can spark a swirl of emotions—uncertainty, frustration, maybe even doubt. What helps?
- Take a brief pause to process feelings (there is no scorecard or timeline for adjustment).
- Reach towards support systems—family, friends, and even supportive online communities.
- Bring doubts, fears, or questions to your healthcare team, no matter how small or frequent.
- Simple, repeatable strategies help with stress: gentle breathing exercises, short walks, time with comforting music.
- Above all: small, steady changes matter vastly more than sweeping, overnight transformations.
If a cloud of worry lingers, sharing your concerns with your medical team could reveal gentle ways forward.
Recent Evidence and Innovations
Research into gestational diabetes moves quickly: emerging markers in blood, refined risk prediction based on genetics, increasing use of continuous glucose monitoring (CGM) for real-time management. Oral medications such as metformin aren’t just discussed, but increasingly scrutinised for both safety and efficacy.
Some of the standout trends?
- Universal OGTT screening at 24–28 weeks
- Bespoke care (personalising choices based on maternal and fetal need)
- A digital edge: telemedicine, remote consultations, and easy access to guidance
- Fresh focus on long-term outcomes, ensuring both parent and child stay healthy beyond pregnancy
Consensus is growing—earlier diagnosis and personal follow-up matter, and ongoing innovation is making tools and care more effective, accessible, and tailored.
Key Takeaways
- Not every instance of glycosuria during pregnancy signals diabetes, yet ongoing findings deserve attentive follow-up.
- Gestational diabetes often shows no early symptoms. Only screening helps in timely detection and safer outcomes.
- Healthy habits—eating, activity, and stress management—aren’t just recommended; they’re truly transformative.
- Expert guidance blends teams together, giving each parent the confidence and autonomy needed to thrive during pregnancy.
- Professional resources and multidisciplinary medical support are widespread. For added support, try the Heloa app—helpful for tailored advice, plus free health questionnaires for your child.
Questions Parents Ask
Can gestational diabetes go away after pregnancy?
For most parents, gestational diabetes does resolve after childbirth as pregnancy hormones that caused high blood sugar reduce naturally. Yet, a period of close blood sugar monitoring just after delivery is still recommended, since some might continue to face higher risk of diabetes later in life. Conversations with your medical team about regular checkups and preventive steps remain important for future wellbeing.
What foods should I avoid with gestational diabetes?
Limiting foods with high amounts of simple sugars is advised—think aerated drinks, sweets, bakery items, white rice, refined flour. Instead, picking whole grains, fresh seasonal fruits in moderation, pulses, and lean proteins can help in balancing blood sugar throughout the day. Tiny changes, like including more salad or swapping white bread for roti, can make a meaningful difference.
Is it possible to have a healthy baby with gestational diabetes?
Yes, with thorough monitoring, smart food choices, and medical support, most parents deliver healthy babies even when gestational diabetes becomes a part of the pregnancy journey. Early identification, ongoing care, and a care plan adjusted to your needs can pave the way for a safe, positive outcome. Each journey is unique, so keeping open communication with your care providers will help you make well-informed choices.
Further reading: