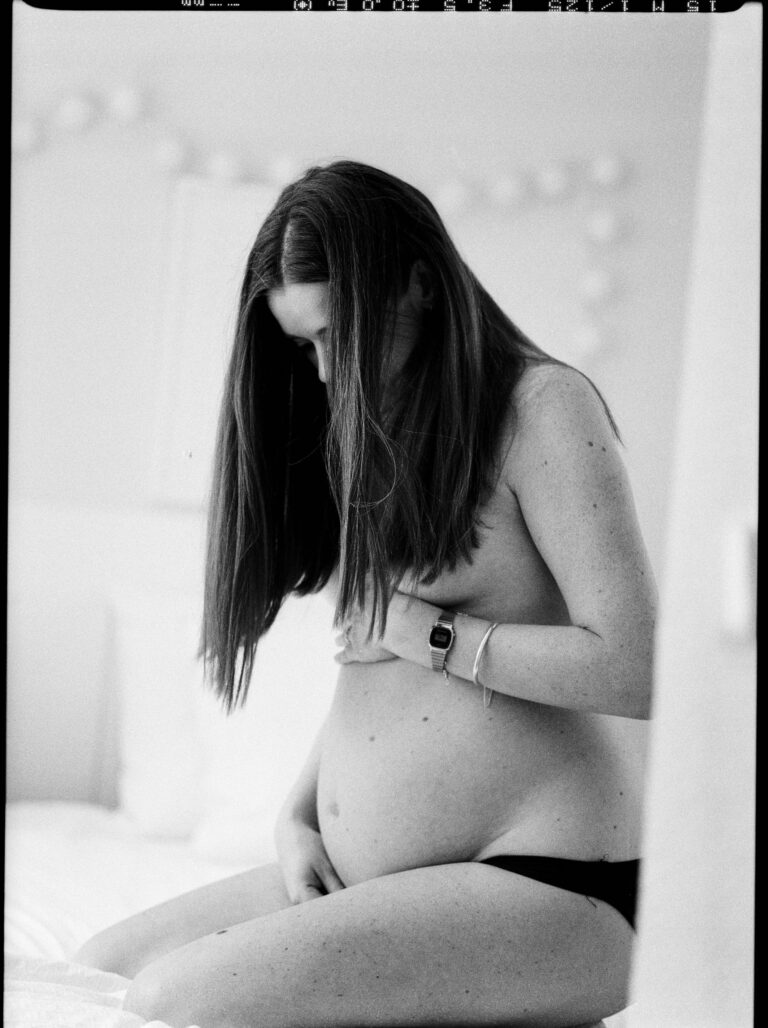
The moment that faint second line appears on a pregnancy test, a breathtaking torrent of questions begins. Should movement slow down, or perhaps become gentler as pregnancy progresses? Is being pregnant and physically active truly safe, or does that expose mother and baby to unwarranted risk? These are not trivial anxieties—between bustling clinic visits and advice from elders, parents often find themselves lost in a maze of contradictory beliefs. The reality is more nuanced than old wives’ tales may suggest. Medical science brings a reassuring voice: physical activity, adapted with care, is more friend than foe during pregnancy. Explore the proven benefits, review the genuine risks, and unravel a tapestry of guidance—spanning safe movements, warning signs, trimester-by-trimester adaptations, and practical tips to blend activity into daily life without guilt or guesswork. Here’s what every parent deserves to know to remain positively pregnant and physically active, making sound choices for health, comfort, and family joy.
Pregnant and Physically Active: Myths, Facts, and Reassurance
Whispers abound—relatives may advise rest, friends might caution against walking, some even link movement to miscarriage. Yet, scientific consensus turns the page on such myths. Unless restricted by a medical condition, being pregnant and physically active elevates well-being: it supports healthy weight, reduces common discomforts like backache, and improves sleep quality. Wondering about adverse effects? Global authorities, including the American College of Obstetricians and Gynecologists, state quite unequivocally that regular, moderate exercise—think brisk walking, swimming, or supervised prenatal yoga—offers more help than harm. The real risk lurks not in movement, but in inertia.
Certainly, pregnancy is not a one-size-fits-all journey. Each experience is unique, and some conditions (for example, placenta previa later in pregnancy, or risk of preterm labour) do call for rest. This is why a preliminary conversation with an obstetrician or trained prenatal expert forms the backbone of safe activity. Once that green light flashes, embracing appropriate exercise can confidently become part of daily routine.
Medical Insights: The Science of Exercise in Pregnancy
Tired of vague assurances? Let’s pivot to real-world evidence. Medical studies show that being pregnant and physically active—that is, engaging in activities such as walking, light strength training, or low-impact aerobics, for about 150 minutes weekly—can cut the odds of gestational diabetes, high blood pressure, and even caesarean delivery. Why? Physical movement fine-tunes the cardiovascular system, enhances metabolic function, and promotes better oxygen exchange. For the baby, improved maternal circulation means more balanced nutrient and oxygen supply.
On the mental health front, the story is just as compelling. Regular exercise reduces risk of prenatal and postnatal depression by at least one-fourth. Sleep interruptions, anxiety, and feelings of overwhelm—these common visitors during pregnancy—are all soothed, at least partially, by a gentle, sustained movement routine. Imagine a day where a short stroll under the morning sun becomes a mood lifter, not a guilty indulgence.
What Activities Are Safe, and What to Sidestep?
One size never fits all. Still, certain activities bring consistent positive results for pregnant bodies.
Safe Choices For Most Pregnant and Physically Active Parents
- Walking: The humble walk, whether slow or brisk, suits nearly every trimester.
- Swimming / Aquatic Aerobics: Buoyancy offers joint relief and reduces swelling.
- Stationary cycling: Keeps the heart rate up but risk of falling down minimal.
- Prenatal yoga or gentle pilates: Flexibility, balance, and mind-body relaxation rolled together.
- Strength training with light resistance bands: Maintains muscle tone without unnecessary strain.
- Pelvic floor exercises: Often overlooked, these help incontinence prevention and speed up postnatal recovery.
Activities to Avoid
- Contact sports such as football, or high-fall risk hobbies like horse riding and rock climbing
- Hot yoga or any strenuous workouts in excessive heat—risk of overheating is real
- Exercises performed flat on the back after 16–20 weeks, as they can reduce blood flow to the baby
- Jumping, sudden direction shifts, and any movement provoking pain, dizziness, or discomfort
Red flags—think vaginal bleeding, severe headaches, or new visual disturbances—demand immediate rest and medical attention.
Tailoring Activity By Trimester
First trimester might surprise parents with a sudden loss of energy, or waves of morning nausea. This doesn’t spell an absolute ban on being pregnant and physically active. If energy permits, keep moving; if fatigue dominates, gentle stretching and short walks become perfectly meaningful achievements.
Winter of tiredness can give way to the spring of the second trimester. As the belly blooms and centre of gravity shifts, modifying activities for stability and comfort is key. Running enthusiasts might switch to cycling. Stretches can continue, though with moderation—hormonal changes make joints more supple, and overdoing it could lead to sprains.
Approaching the third trimester, comfort is paramount. Appetite for strenuous activity often fades, but movement still matters—pelvic floor routines, swimming, and mindful relaxation (meditation or breathing exercises) keep muscles engaged and minds calm. The focus gently shifts from exertion to preparation for labour and smooth recovery.
The Role of Nutrition and Hydration for the Pregnant and Physically Active
Fueling the body correctly transforms exercise from a chore to a source of energy. Pregnancy and activity both raise the body’s nutritional demands. Bump up daily calories (by 300–500 in later months if maintaining an active lifestyle), prioritise fresh fruits, colourful vegetables, lentils and lean protein. Before exercising, a small snack—perhaps a banana and a handful of peanuts—keeps blood sugar steady. After activity, mix protein and carbs to aid muscle repair.
Hydration is non-negotiable. Drink at least 8–10 cups water daily—another 1–2 cups extra if exercising or sweating heavily. Cloudy urine, headaches, or dry mouth? These could point to dehydration. Always keep a bottle handy, sip often, and never wait for thirst to build.
Never skip prescribed prenatal vitamins—iron, folic acid, calcium—these building blocks fortify both mother and growing baby, especially for those pregnant and physically active.
Risks, Red Flags, and When to Put Movement on Pause
Medical professionals reassure: for most, exercise poses little threat when approached thoughtfully. Still, overexertion, unintentional overheating, and neglecting rest can tip balance towards harm. Warning signals—blood loss, painful contractions, sudden swelling or breathlessness—cannot be brushed aside. These moments warrant an immediate break and, most importantly, a visit to the healthcare provider.
A handful of conditions—such as severe anaemia, unexplained vaginal bleeding, preterm rupture of membranes, or twins after 28 weeks—make even moderate activity less safe. Here, prescribed rest is a sign of wisdom, not defeat.
Practical Strategies to Stay Motivated and Consistent
Fatigue, unpredictable schedules, and endless to-do lists may sap motivation. Break movement into short, daily rituals—a ten-minute walk in the morning, another in evening. Choose activities that spark joy, rather than feel like obligation. Enlist a companion or join gentle group classes for accountability.
Progress happens in increments, not leaps. Celebrate every bit of activity—and remember that adapting is a sign of care, not weakness. Feeling low on willpower? Even a few stretches count. The idea isn’t competition, but care.
How Physical Activity Fuels Maternal and Baby Health
Physical movement during pregnancy is no small investment. It’s linked to:
- Improved fetal circulation and heart function (yes, baby’s heart rate variability can be a silent marker of positive outcome!)
- Lowered risks of needing a C-section or facing persistent pregnancy hypertension
- Enhanced postnatal recovery
- Reduced odds of gestational diabetes or mood disorders for parents
- Smoother, often quicker labour
- Improved sleep and digestion
Science shouts out—being pregnant and physically active is, when medically allowed, a foundational building block for the health of both generations.
Restarting Activity Safely After Delivery
Following childbirth, the urge to “bounce back” can be powerful. Yet, the body benefits most from gentle, gradual resumption of movement. For some parents, short walks and focused pelvic floor exercises make sense within days of a natural birth. After surgery or complications, listen to medical advice before lacing up those sneakers.
Why bother? Postpartum exercise supports mood, strengthens abdominal and pelvic muscles, maintains healthy weight, and ushers more energy into busy days. Expect setbacks. Expect different pacing. Respect the body’s cues. Progress, not performance, holds the real value.
Expert Support – The Value of Professional and Community Guidance
The maze of pregnancy advice can bewilder. Leaning on expertise—obstetricians, midwives, physiotherapists—transforms uncertainty into clarity. Individualised exercise plans respect personal health, fitness background, and evolving needs. Local prenatal programs, trusted resources like WHO or the CDC, and, above all, open dialogue with a caregiver, establish a foundation for safe, confident activity.
Key Takeaways
- Being pregnant and physically active is usually safe and highly beneficial—boosting heart, mind, and body when guided by sound medical principles.
- Listen to your body: adapt activity as trimesters unfold, and trust sensations that signal the need for pause or rest.
- Combine nutrition, hydration, and movement for the best outcomes.
- Warning signs—however minor they might seem—require prompt attention.
- Expert guidance, along with social or digital support like the application Heloa, smooths the journey with evidence-based advice and personalised questionnaires.
- There’s no contest: every step, no matter how small, counts.
Questions Parents Ask
Can you start exercising during pregnancy if you were not active before?
Certainly! Even if exercise wasn’t part of routine before, gently starting movement during pregnancy—perhaps a slow walk in the neighbourhood or simple prenatal yoga—delivers meaningful value. There’s no reason to force intensity; the most important thing is listening to body signals, progressing slowly, and confirming any plan with your doctor. Each bit of regular movement can help, especially when tailored to comfort and safety.
How can you tell if you’re doing too much physical activity while pregnant?
Wondering if you’ve crossed the line? Pay attention to warning signs such as unusual tiredness, dizziness, feeling breathless without relief, or physical discomfort. Fresh episodes of vaginal bleeding, swelling, or generally feeling unwell mean it’s time to stop and consult your health provider. Taking frequent breaks and pacing yourself—plus adding rest days—is not only permissible, but wise during this journey.
What are some tips for staying motivated to exercise during pregnancy?
Motivation sometimes disappears—blame hormones, fatigue, or simply a busy day. Setting realistic, small targets, choosing activities you genuinely enjoy, and joining a friendly prenatal class or involving a partner can add an extra lift. On days when energy feels low, even a short stretch session or an easy walk helps, and every little effort should be acknowledged. The journey is personal—steady progress and kindness to oneself matter most.
Further reading: