Hormones and menopause—words that can make many parents pause, wondering what truly unfolds inside their bodies as this new chapter approaches. Perhaps you have noticed changes and pondered, “Is this normal? What can I do to support my health?” These are not just passing questions; they reflect genuine concerns about daily well-being, family dynamics, and long-term vitality. The horizon of menopause, shaped by the interplay of powerful chemicals like estrogen and progesterone, ushers in both uncertainty and opportunity. From unpredictable hot flashes to shifting moods, hormonal changes can ripple into many corners of life. Understanding these waves—what causes them and how to manage their effects—can ease the journey, dispel misconceptions, and help parents support both themselves and their loved ones.
Understanding Hormones and the Menopausal Transition
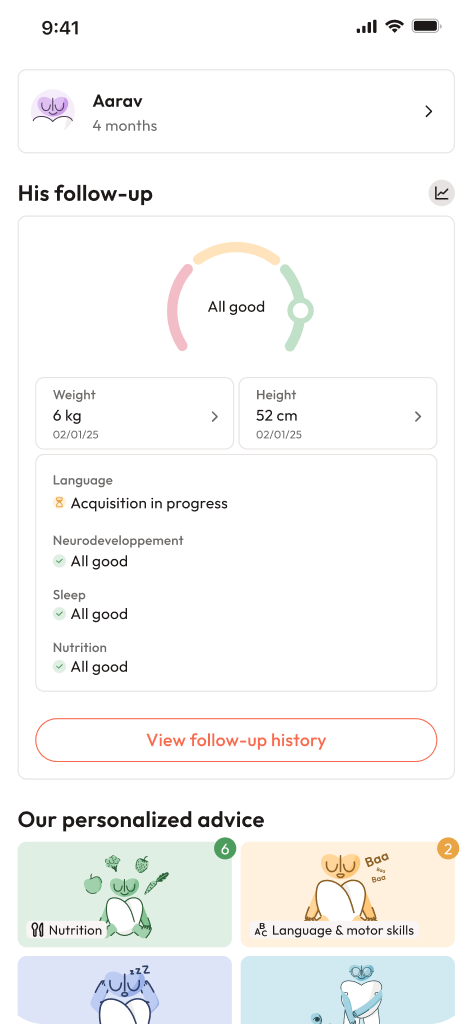
Menopause is not simply an abrupt ending but a complex biological evolution. As the ovarian reserve dwindles, the elegant choreography of hormones begins to shift. Estrogen and progesterone—the main players—see their levels dip sharply, leading to a cascade of physiological transformations. Menstrual cycles change character, sometimes erratic, at other times heavier or lighter until, one day, they stop altogether. This phase, often termed perimenopause, is peppered with irregular periods, mood changes, and sleep disruptions. But why does this happen? The answer lies in the fluctuating responses of the ovaries to follicle-stimulating hormone (FSH) and luteinizing hormone (LH), which spike as ovaries become less responsive.
Consider this: estrogen doesn’t just govern periods—it supports the skin’s plumpness, the heart’s rhythm, and even influences how we think and feel. When its influence wanes, the body adapts in unexpected ways, forcing parents to recalibrate their routines, their diets, and sometimes their outlooks. The median age for menopause is about fifty-one, but there’s no universal template—family history, ethnic background, and lifestyle all leave their marks. For some, symptoms are barely noticeable; for others, they feel all-encompassing.
Hormonal Changes and Their Effects
Hormones and menopause impact almost every cell. The famed hot flash—sudden, searing, and as unpredictable as the monsoon—traces its root to changes in how the brain manages heat. Lower estrogen disturbs the hypothalamus, triggering vasomotor symptoms: not just hot flashes, but also night sweats and palpitations. Up to 80% of women describe these feelings, often at the least convenient moment.
The decline in estrogen also transforms the urogenital tract. Lowered mucosal strength leads to vaginal dryness and can make intimacy uncomfortable. Sometimes urinary issues surface—an urgent need to visit the restroom or unexpected leakage when coughing or laughing. Infections may appear more frequently due to thinned mucosa.
Changes aren’t merely skin-deep. Reduced collagen production, a hallmark of lower estrogen, leaves skin feeling less supple, dry, perhaps a little more fragile than you remember. Unwanted facial hair? Thinning on the scalp? These are linked to the new hormonal balance, sometimes with emotional consequences as unsettling as the physical ones.
What about bones? Estrogen offers double protection: supporting bone density while slowing down bone loss. Its tapering heightens the risk of osteoporosis—a silent condition where bones become brittle. Spontaneous fractures can be one of the first signs, making daily calcium and vitamin D, plus load-bearing exercises, immediate allies.
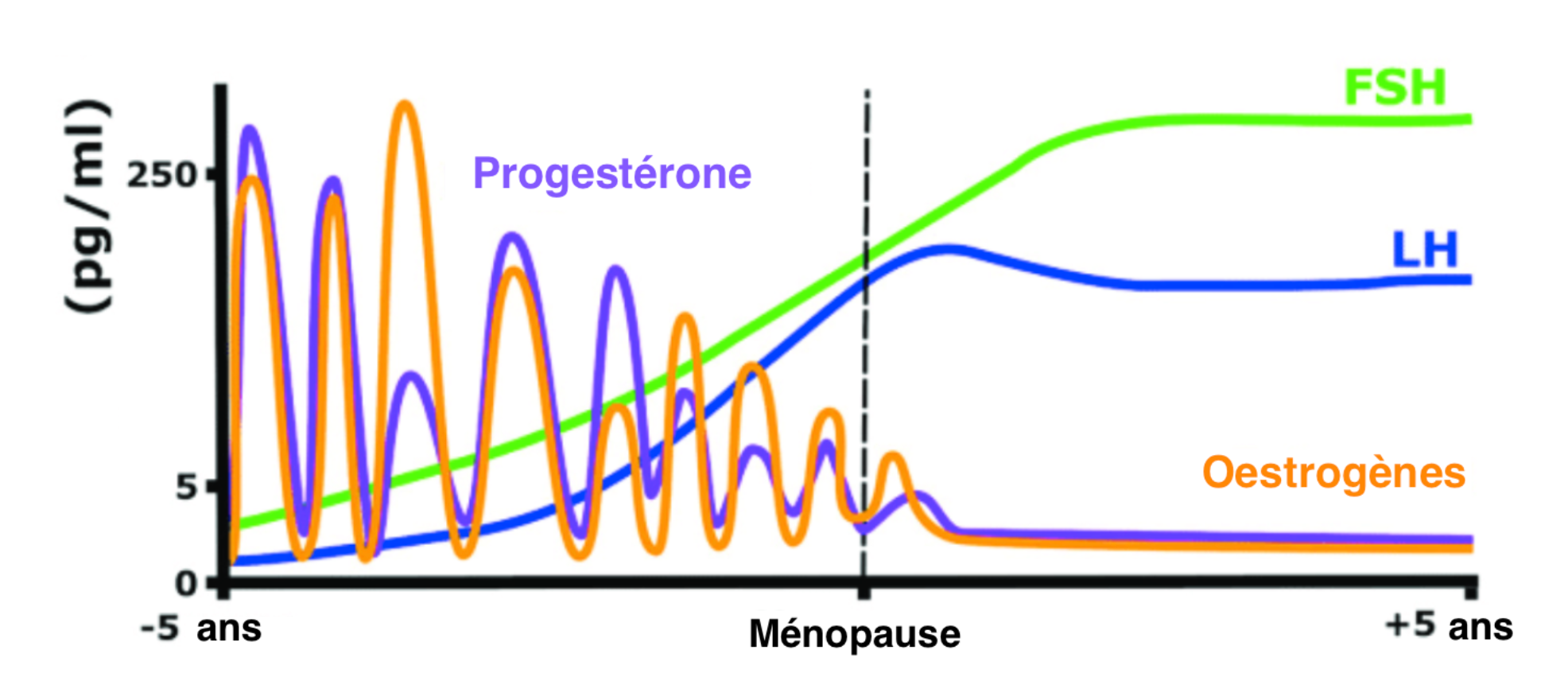
Mood, cognition, and energy also sway under the shadow of hormonal change. Anxiety, irritability, or even full-blown depressive episodes may arise—some fleeting, others more persistent. Sleep often suffers; tossing and turning, woken by night sweats, the consistent sleep of youth can feel like a distant memory. Weight changes, particularly an expansion around the waist, reflect deeper metabolic shifts. Some parents notice a loss of libido, for which biology shares space with psychological and relationship influences. Over time, waning estrogen gently raises the risk of heart disease, making healthy lifestyle choices ever more relevant.
Diagnosis and Monitoring Menopause
Hormones and menopause are typically recognized by the absence of periods for twelve months. No complicated tests are needed for most—your story is the strongest clue. In some situations, especially for younger women or where the picture isn’t clear, checking levels of FSH and estradiol can provide clarity. FSH typically climbs above 30–40 IU/L, while estradiol dips below 20 pg/mL during menopause, though there is a natural ebb and flow during perimenopause.
A host of other scenarios can mimic menopause—thyroid issues, pituitary disorders, surgical removal of the ovaries, or premature ovarian insufficiency. Ruling out pregnancy, polycystic ovarian syndrome (PCOS), or hypothalamic amenorrhea is important for accurate management and peace of mind.
Hormone Replacement Therapy (HRT) and Symptom Relief
The swirl of symptoms during menopause prompts many to ask: is there relief? Hormone Replacement Therapy (HRT) steps in here, replenishing some of what’s lost, especially for hot flashes, urogenital symptoms, and bone protection. Options include estrogen-only therapy (for women without a uterus), combined estrogen-progestin (if the uterus is intact), and bioidentical hormones—agents that mimic the body’s natural chemicals, though the compounded versions are not always regulated.
Like all significant choices, HRT demands balance. While benefits include reduced hot flashes and preservation of bone mass, there are trade-offs: a slightly higher risk of breast cancer (mainly with combined therapy), deep vein thrombosis, and stroke if begun after age sixty or continued long-term. Transdermal patches and gels tend to pose lower risk of clots and metabolic disruption than tablets. Timing matters: starting sooner after menopause, at the lowest workable dose, is advised for most. There are scenarios, like a history of breast cancer or certain kinds of bleeding or blood clots, where HRT is avoided.
For those who cannot or would prefer not to use hormones, non-hormonal medications like SSRIs, SNRIs, gabapentin, and SERMs (Selective Estrogen Receptor Modulators) can still ease symptoms. It’s reassuring to know that effective alternatives exist.
Nutrition and Lifestyle for Hormonal Balance
Daily choices can amplify or soothe the effects of hormones and menopause. Nutrition is foundational: phytoestrogens—naturally occurring plant chemicals found in flaxseed, soy, and legumes—may gently mimic estrogen. Load your plate with vegetables, whole grains, lean proteins, and sources of omega-3 fatty acids. Calcium and vitamin D become non-negotiables for bone protection.
Physical activity is the backbone of long-term wellness. Simple walks or resistance training, repeated regularly, stave off bone loss and ease stress. Sleep hygiene deserves special attention: establish a predictable bedtime, keep your space cool, and watch out for caffeine or alcohol late in the day—each can disrupt fragile sleep.
Stress management is not a luxury. Techniques like deep breathing, meditation, or even short breaks for yourself buffer the effects of heightened cortisol, which often runs high during busy parenting years. Family connections—shared meals, group walks, open conversations—strengthen not just parent-child bonds but also reinforce lasting healthy habits.
Personalized advice from a dietitian can help address specific needs, fine-tuning nutritional choices where medical issues or preferences come into play.
Advances and New Options in Menopause Care
Hormones and menopause remain vibrant areas of medical progress. Selective Estrogen Receptor Modulators (like ospemifene and bazedoxifene) target specific tissues, easing vaginal symptoms or supporting bones while bypassing organs like the uterus or breast. Fresh entrants—neurokinin 3 receptor antagonists (such as fezolinetant)—offer hot flash relief by recalibrating brain mechanisms, completely hormone-free.
Women who reach menopause earlier than average, especially after surgery, contend with a rapid hormone decline, increasing the risk for osteoporosis, heart disease, and depression. For these individuals, supportive therapy (including HRT until the usual menopausal age) is often a significant ally.
Male Hormones and Aging
Is there a male equivalent to menopause? Not in the same sense. “Andropause” occasionally surfaces in conversations but lacks the sharp hormonal drop seen with menopause. In men, the gradual decline of testosterone may influence libido, the frequency of morning erections, and the ease of achieving or sustaining erections. Hair loss is influenced more by genetics than hormone shifts, and testosterone’s main influence concerns body hair, not scalp coverage.
Long-term Health, Support, and Wellness
Maintaining wellness during and after menopause benefits from teamwork: regular bone checks (DEXA scans), cardiovascular risk assessments (like cholesterol and blood pressure tests), and consistent cancer screening, including mammograms. Open communication—whether about intimacy, dryness, or general well-being—strengthens relationships and helps address potential challenges early.
Professional assistance—whether from a gynecologist, endocrinologist, dietitian, or mental health provider—tailors care directly to your story and your family’s needs. Emotional health matters deeply; if low moods, anxiety, or memory changes linger, support is always justified.
Ultimately, hormones and menopause signify evolution rather than decline. With information, support, and steady care, parents can traverse this landscape with resilience, continuing to set powerful examples for family health.
Key Takeaways
- Hormones and menopause mark a natural stage in life, orchestrated by the interplay of estrogen, progesterone, and other key regulators.
- Symptoms can range from subtle to disruptive but are all part of the transition.
- Clinical diagnosis is most often based on menstrual history, with hormone testing for special cases.
- Relief for symptoms is available—hormonal, non-hormonal, and lifestyle-based approaches all have a place.
- Balanced nutrition, daily movement, and strong sleep habits underpin smoother physical and emotional transitions.
- Scientific advancements and individualized strategies support diverse needs, including early or surgical menopause.
- For men, aging-related hormonal changes exist, but without a menopause equivalent.
- Support—from professionals and loved ones—can make a world of difference. For extra guidance, parents can download the application Heloa for practical tips and free health questionnaires for children, adding another dimension to proactive family care.
Questions Parents Ask
Can menopause affect memory or concentration?
It is quite usual during hormones and menopause to notice changes in memory or trouble keeping focus. Many parents mention feeling forgetful or experiencing “brain fog.” Such symptoms are closely related to shifting estrogen levels, which play a part in how the brain works. For most, this is temporary and tends to settle as the body adapts. Simple organisation—using reminders, writing things down, incorporating daily routines—often helps. If these troubles persist or disrupt daily functioning, meeting a healthcare professional for a check-up is advised.
Can menopause impact heart health?
Definitely. The fall in estrogen decreases some of the heart’s natural protection, making high blood pressure and cholesterol changes more common. For parents, prioritising cardiovascular health is now especially important: regular exercise, balanced meals (with less fatty or salty food), staying away from tobacco, and scheduled health reviews do make a big difference. For those with a family background of heart disease, discussing more specific strategies with a doctor is very wise.
How can I talk to my children about menopause?
Starting such conversations can feel awkward. Still, using familiar, age-appropriate language helps children make sense of change. A simple explanation like, “My body is changing as I grow older, and it’s completely natural,” normalises your experiences for children. If you’re unsure where to begin, giving honest, reassuring answers and inviting children’s questions fosters understanding and trust. Some parents also find that storybooks or digital resources designed for families can open up this dialogue naturally.
Further reading: