Juggling school schedules, family meals, extracurricular chaos – as a parent, you constantly decode aches and anxieties, some whispered between maths homework, others behind closed doors. But what happens when menstrual pain or persistent discomfort in your child doesn’t match the “normal” everyone talks about? Maybe you’ve heard the term endometriosis, perhaps in passing, or witnessed stories of invisible battles. The name itself is heavy, tangled with medical complexity and emotional weight. For any parent standing before the unknown, asking, “Is my child just unlucky with periods, or is something more at play?”, here begins a journey of medical clarity, practical tips, and reassurance — because complex conditions like endometriosis deserve attention, empathy, and informed action. Expect to find clear answers on what exactly endometriosis is, its symptoms and complications, why early recognition matters, and how you can seek the right care for your child.
What is endometriosis? Unravelling the basics
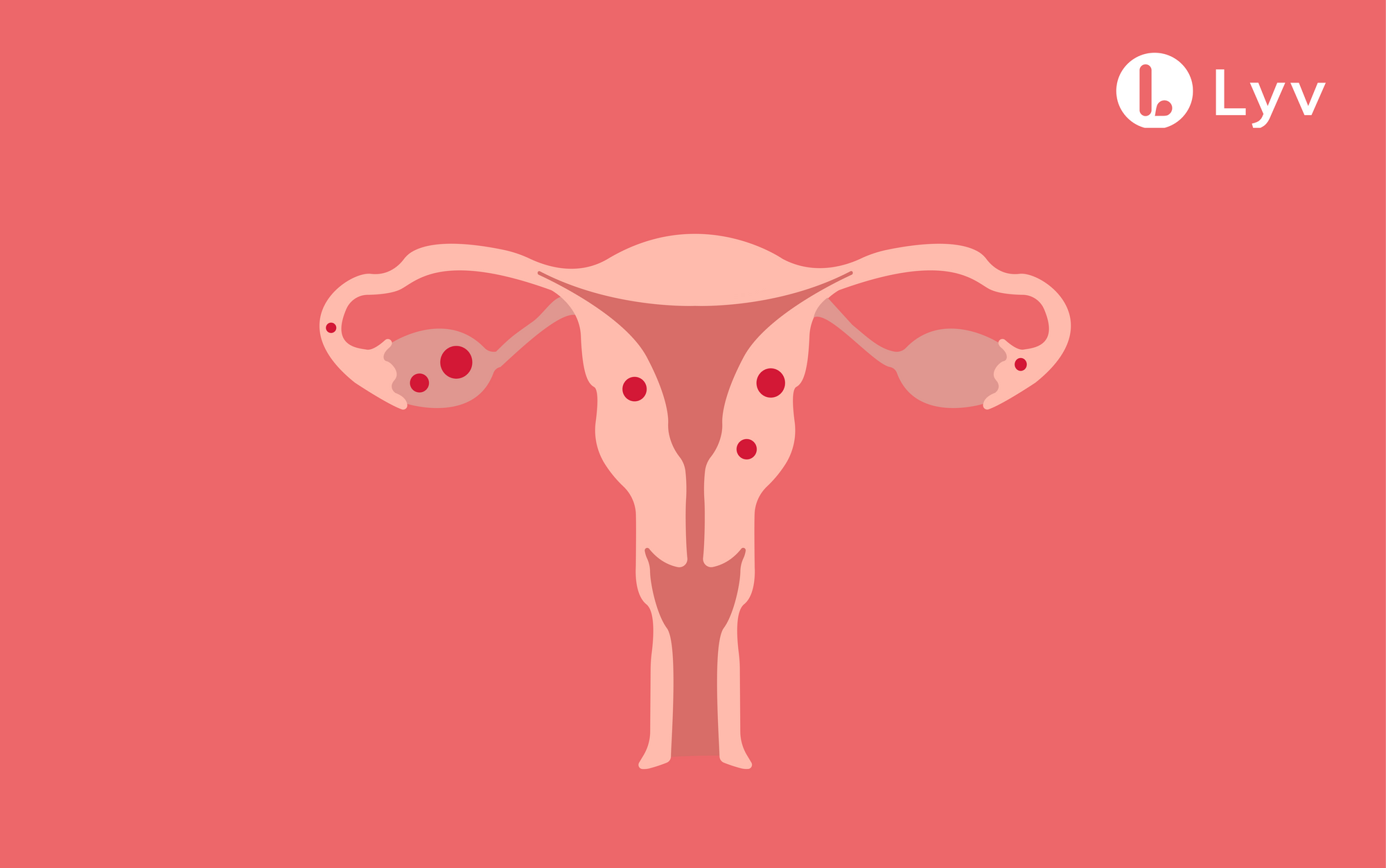
Ever wonder how a process as natural as menstruation could turn hostile against the body itself? In endometriosis, tissue remarkably similar to the endometrium (the uterine lining that thickens and sheds each cycle) ventures beyond its intended territory. Instead of neatly being expelled during periods, this tissue finds itself stranded in unexpected locations — ovaries, fallopian tubes, the outer walls of the uterus, sometimes even the bladder or intestines, and on rare occasions, much farther. Each month, influenced by hormonal changes, this rogue tissue reacts, swells, or bleeds, but unlike normal menstrual blood, it becomes trapped, sparking inflammation, irritation, and ultimately, pain.
Why does this happen? The root cause remains elusive. Suggestions include retrograde menstruation (where menstrual blood reverses course in the pelvic cavity), immune responses failing to clear misplaced cells, and even genetic predispositions. The only constant is unpredictability: endometriosis can be mild and silent, or it can disrupt daily routines, ambitions, and teenaged confidence with relentless persistence.
The many faces of endometriosis: understanding disease types
Not every case looks the same, and that’s exactly why diagnosis may slip under the radar for years. Recognising this mosaic helps in setting realistic expectations:
- Superficial peritoneal endometriosis: Think of small, flat spots scattered on the lining of the abdomen or pelvis, often difficult to spot on standard scans.
- Deep infiltrating endometriosis: Here, tissues burrow deep beneath the surface, sometimes affecting vital organs such as the bladder, bowel, or vaginal wall, causing pronounced and often cyclical pain.
- Ovarian endometriomas (“chocolate cysts”): These are cystic growths on the ovary, filled with old blood, notorious for causing pain and contributing to fertility problems.
Tissue can, albeit rarely, settle on surgical scars or extend into regions like the diaphragm or even lungs. Each type might bring its own set of challenges, which is why medical evaluation is always tailored and thorough.
Who is at risk? Decoding onset and vulnerability
Can a teenager face endometriosis? Absolutely, and often that’s where the whispers of pain first begin—at menarche or soon after. Early onset of menstruation (before 11), heavy or unusually long periods, or a family history (your mother or sister has been there) may tip the odds. Ethnicity and genetic factors may also influence risk, and, sadly, disparities in health care mean the problem is often underdiagnosed. Although most prevalent during the reproductive years, endometriosis respects no strict rules about age.
Signs and symptoms: listening, observing, and understanding
Not every pain signals the same story. Endometriosis, ever the master of disguise, can produce a varied picture from one person to another:
- Intense pelvic or abdominal pain during periods, ovulation, or sometimes even between cycles. The pain may feel stabbing, radiate to the back, or defy over-the-counter medication.
- Dysmenorrhea: Periods start with pain, sometimes even before bleeding, and the discomfort can halt school and activities.
- Dyspareunia: Pain during or after sexual activity (especially relevant as teens grow older).
- Digestive upsets: Bloating, nausea, diarrhoea, constipation—sometimes misread as food intolerance or just “bad luck.”
- Dysuria or pain during bowel movements: Especially near menstruation.
- Chronic fatigue: Not just being tired, but a kind of exhaustion that lingers despite rest.
- Difficulty conceiving: Up to 40% may find natural pregnancy challenging as adults, but this is just one variable among many.
- Psychological toll: Anxiety, low mood, strain on friendships and studies—a silent burden tucked beneath daily resilience.
Some children or teens might show just one or two symptoms, others may tick nearly every box. Importantly, symptom severity doesn’t always mirror the extent of disease seen during scans or surgery. This mismatch can be deeply confusing—both for parents and children.
Why early recognition and intervention matter
How does a delay of 7-10 years between symptom onset and diagnosis even happen, you wonder? It’s a mix of societal taboos, mislabelled pain (dismissed as “normal periods”), and limited access to gynaecological expertise in many areas. The result: children and adolescents enduring pain that erodes well-being, emotional confidence, and even future fertility. Attentive parenting—listening without judgement, validating instead of minimising complaints—lays the foundation for timely help. Early diagnosis and support have been shown to reduce complications, future emotional distress, and improve quality of everyday life for affected youth.
Diagnostic roadmap: from suspicion to certainty
No single blood test confirms endometriosis—unlike a throat infection or anaemia, there’s no shortcut. Instead, diagnosis combines several layers:
- Detailed medical history: A doctor probes for timing, character, and triggers of pain, checks family history, and asks about how symptoms impact school, play, and friendships.
- Physical examination: In adolescents, this is handled with particular sensitivity. Many times, examinations find nothing obvious.
- Imaging: Transvaginal or pelvic ultrasound may detect large cysts or deep infiltrating lesions, while MRI provides higher detail in complex cases.
- Laparoscopy: A low-risk surgical procedure where a camera inspects the pelvic cavity—a gold standard for official confirmation and staging. It can diagnose and sometimes treat visible lesions during one procedure.
Emerging science looks towards new frontiers like biomarkers from blood or urine, and advances in non-invasive imaging, but these are not yet routine. Meanwhile, collaborative care involving both parents and medical professionals is invaluable.
Causes: knowns, unknowns, and popular theories
Why my child? This question haunts many parents. Science points towards a complex web:
- Retrograde menstruation: Menstrual blood moves backwards and deposits cells in the pelvic cavity.
- Genetic tendency: If close relatives have endometriosis, the risks are higher.
- Immune dysfunction: The body might fail to clear the misplaced tissue, allowing it to persist and grow.
- Hormonal exposure: High levels of estrogen over a lifetime (through early, heavy, or long periods) provide fertile ground for lesion growth.
- Environmental exposures: Factors like certain toxins, and possibly factors related to modern lifestyles, may play a role, though evidence is not definitive.
Severity staging: understanding extent and implications
Doctors divide endometriosis into four stages—minimal, mild, moderate, and severe—based on location, depth, and the presence of adhesions or cysts. Stage I may mean a few scattered lesions, while Stage IV can involve large cysts, severe adhesions that “glue” organs together, and disrupted anatomy. Yet, a person with “mild” disease could have severe symptoms, and vice-versa, which often frustrates families seeking straight answers.
Complications: physical, emotional, and future health
Leaving endometriosis untreated can lead to:
- Chronic pain: Affecting school, hobbies, and sleep.
- Adhesions and scar tissue: These form a network of internal “bands” that can cause further pain and digestive or urinary problems.
- Ovarian cysts (endometriomas): Prone to rupture or grow larger, sometimes compromising ovarian function.
- GI and urinary tract troubles: If tissue involves the intestines or bladder, symptoms may flare during cycles.
- Rare complications: Endometrial tissue, though very rarely, can migrate upwards to the chest, causing chest pain during periods.
- Associated health risks: Scientific links to adenomyosis (where tissue invades the uterine muscle) and, to a lesser extent, some ovarian cancers.
- Psychological impact: Persistent pain—hardly visible to others—breeds anxiety, sadness, isolation, or even depression, especially if school performance or friendships are affected.
Endometriosis and fertility: what should parents know?
Infertility can loom as a daunting possibility—about 30–50% with endometriosis may face challenges. The reasons include anatomical changes, inflammation interfering with ovulation or fertilisation, and the effects of cysts or adhesions. Even when conception occurs, risks like miscarriage or preterm labour tick modestly upwards. Early intervention with compassionate, expert care can help safeguard future fertility and address concerns proactively.
Available treatments and practical daily management
While a permanent cure remains elusive, effective management is entirely possible:
- Hormonal therapies: Birth control pills, progestins, or even medicines to induce a temporary “menopause” aim to halt menstrual cycles and reduce pain.
- Pain relief: NSAIDs help many, but severe cases often need more tailored approaches.
- Surgery: Laparoscopy can remove visible lesions and break adhesions. In rare, severe circumstances, more extensive operations (like hysterectomy, removal of the uterus) may be discussed—generally reserved for those who have completed their family.
- Complementary measures: Gentle exercise, yoga, mindfulness, dietary adjustments (focusing on fibre, fruits, vegetables, and possibly reducing processed foods), and heat therapy bring comfort to some.
- Assisted reproductive technologies: IVF and intrauterine insemination provide hope in the face of fertility troubles.
- Psychological support: Talking therapy, peer groups, school counsellor involvement—never underestimate the strength a listening ear or community brings.
Approaches are always individualised, accounting for age, present and future needs, and the personal impact of symptoms. Regular follow-up and an open dialogue with healthcare professionals remain central.
Prevention and supporting early intervention
You may wonder if anything can truly prevent endometriosis. The medical consensus: while full prevention may not be attainable, there are trends worth noting. Extended breastfeeding, pregnancies, and long-term use of hormonal contraceptives can modestly lower the risk by reducing menstrual frequency. But these are personal and sometimes private decisions, each with its surrounding considerations. Ultimately, supportive listening, early recognition of symptoms, and rapid referral to a specialist create the strongest shield.
Awareness and reducing diagnostic delays
The average time to diagnosis—7 to 10 years. Can this truly be shortened? Increased education among parents, teachers, coaches, and healthcare professionals holds a powerful lever. Validating expressions of pain, encouraging open dialogues about menstrual health, and knowing when to seek a paediatric gynaecologist or adolescent health expert can turn whispered worries into real solutions. Peer support forums, reputable online platforms, and ongoing research are valuable allies in this journey.
Research, technology and hopes for tomorrow
Exciting chapters lie ahead. Scientists are chasing non-invasive diagnostic techniques like blood or urine biomarkers and highly sensitive imaging. New waves of medical treatment—targeted therapies that modulate hormones or the immune system, eventually with gentler side effect profiles—are on the horizon. And in the meantime, multidisciplinary care teams (combining gynaecologists, pain specialists, physiotherapists, and psychologists) are transforming management, demolishing the idea that endometriosis is a solitary medical battle.
Prevalence and invisible impact
It’s estimated that around 1 in 10 females of reproductive age worldwide experience endometriosis, but true numbers may be higher, especially in communities facing health access challenges. Beyond medical bills, the condition causes missed school days, lost opportunities, and ripple effects on family dynamics. Emotional support, school accommodations, and flexibility become meaningful pillars—far beyond any prescription pad.
Key Takeaways
- Endometriosis is a complex health condition rooted in misplaced tissue and driven by hormonal cues, with consequences stretching far beyond just pain.
- Symptoms like severe menstrual or pelvic pain, digestive troubles, fatigue, and even delayed fertility may hint at its presence—but each story is unique.
- Early recognition by attentive parents, validation of symptoms, and prompt specialist care create the strongest path to a healthy future.
- Multiple approaches, from medication to surgery and lifestyle tweaks, can successfully manage symptoms and safeguard both physical and emotional wellbeing.
- Emotional support and practical solutions exist – from evidence-based platforms to school counsellors and paediatric specialists.
- Educational outreach and ongoing research are driving a more hopeful, informed path forward for families.
- For tailored advice, free health questionnaires, and personalised parenting guidance, don’t hesitate to explore the Heloa app.
Questions Parents Ask
Can endometriosis occur in young girls and teenagers?
Yes, endometriosis doesn’t wait for adulthood. It can begin as early as the first menstrual cycles in adolescence. If your child often misses school or feels overwhelmed by painful, heavy periods, consider a medical discussion sooner rather than later. Early handling brings lightness back to everyday life.
Is endometriosis hereditary?
A family connection is well established. When a close relative such as a mother or sister has experienced endometriosis, the probability does climb. Still, genetics are just one piece. Hormonal, immune, and environmental factors together paint the bigger picture.
Can lifestyle or dietary changes help manage endometriosis symptoms?
While lifestyle changes won’t “solve” endometriosis, practical steps can offer comfort. A diet high in fruits, vegetables, and fibre, regular light exercise, stress relief, and consistent sleep may ease certain symptoms. Encourage your child to maintain a health diary and discuss any new approaches with the doctor, so the care remains safe and tailored.
How is endometriosis diagnosed?
Diagnosis involves a blend of medical history, physical exams, imaging (like ultrasound or MRI), and sometimes a laparoscopy—a small camera-guided operation providing clear answers. The process may feel lengthy but is designed for accuracy and long-term health.
Does endometriosis affect fertility?
It can, for some. Endometriosis might disrupt pelvic organs or ovulation, making conception more challenging. However, with early intervention and dedicated reproductive support, many do go on to conceive.
What are treatment options for endometriosis?
Treatments include hormonal medicines, pain relief, surgery, lifestyle adjustments, and psychological support. Strategies depend entirely on age, symptoms, and individual goals. Exploring all options with a trusted healthcare professional is the key.
Can endometriosis be prevented?
Complete prevention isn’t currently possible, though reducing menstrual cycles through breastfeeding or hormonal contraception might lower risk. Early attention to symptoms, ongoing support, and timely specialist access remain your best guardrails.
What resources are available for families?
Seek guidance from specialist healthcare providers, school counsellors, peer forums, and trusted online resources. Digital platforms and community groups open doors for reliable, practical help amidst the journey with endometriosis.
Further reading :