You want to know what is happening inside your body, what you can do right now, and when to ask for more support. You may be excited, a little anxious, or both, and that mix is completely understandable. Here is the reassuring part, the science of fetal development offers a clear map, practical next steps, and meaningful ways to support your baby, from the first cell divisions to the first cry.
Trimester map and why timing matters
Fetal development follows a steady rhythm, early structure building, then rapid growth, then fine tuning for life after birth. Timing shapes screening windows, ultrasound check points, and how clinicians interpret changes in growth or movement.
- First trimester, organ formation, highest sensitivity to harmful exposures, and early dating by ultrasound
- Second trimester, growth accelerates, sensory pathways come online, detailed anatomy evaluation
- Third trimester, brain and lung maturation, fat deposition, and birth readiness
You may wonder, how does gestational age differ from conception age. Clinicians count from the first day of the last menstrual period, so gestational age runs about two weeks ahead of conception age. This distinction keeps appointments and screening windows on track.
Week by week, what is happening now
Weeks 1 to 4, conception to implantation
- Fertilization creates a zygote that divides quickly, forming a blastocyst that travels to the uterus, then implants and sets up early placental structures and the yolk sac.
- A small gestational sac may appear on ultrasound around week 4 to 5, once visible, crown rump length is the best early dating measure.
- By the end of week 4, the embryo is only a few millimeters, smaller than a poppy seed.
- Practical tip, early dating by crown rump length improves due date accuracy.
Weeks 5 to 8, organogenesis begins
- The neural tube closes, the primitive heart begins to beat, limb buds form, facial primordia appear, organ systems start to take shape.
- Cardiac activity often appears by weeks 6 to 7 on ultrasound.
- By week 8, think kidney bean size.
- Supportive habit, begin or confirm folate if not already started, and avoid known teratogens, that is substances that can disrupt development.
Weeks 9 to 12, the fetal period and early reflexes
- Around week 9, the embryo is called a fetus, genital differentiation begins, early movements appear, organ systems shift from formation to maturation.
- First trimester screening, nuchal translucency paired with blood tests, is time sensitive in this window.
- By week 12, length is about 5 to 6 centimeters, lime like in size.
Weeks 13 to 20, rapid growth and protective skin coatings
- Length growth surges, neural networks expand, bone mineralization increases, facial features become distinct, lanugo and vernix appear to protect delicate skin.
- Many people first feel movement, quickening, in this window.
- The anatomy scan around 18 to 22 weeks evaluates the brain, heart, spine, kidneys, limbs, and placenta.
Weeks 21 to 28, lung branching, brain growth, and responses to the world
- Airways branch and early surfactant production begins, brain growth is brisk, the fetus responds to sounds, sleep and wake cycles become more defined.
- Survival outside the womb becomes possible near 23 to 24 weeks with advanced neonatal care, and corticosteroids are used if preterm birth is likely, to boost lung readiness.
Weeks 29 to 36, weight gain and coordinated function
- Rapid weight gain and fat deposition, thicker skin, maturing swallowing and sucking, continued brain folding, increasing sensitivity to light and sound.
- Growth scans may assess estimated fetal weight, amniotic fluid, and placental function when indicated.
Weeks 37 to 40 plus, term maturation and birth readiness
- Lungs and other organs complete maturation, many fetuses settle head down, practice breathing motions continue, preparing for life outside the womb.
- Final decisions depend on fetal growth, maternal health, and gestational age, small timing shifts around the due date are common.
Stages explained, germinal, embryonic, and fetal
- Germinal stage, fertilization through implantation, rapid cell divisions and early placental formation.
- Embryonic period, about weeks 3 to 8 after fertilization, major organs form, exposures here can cause structural anomalies.
- Fetal period, week 9 onward, growth and function take center stage, with a strong focus on brain complexity and organ maturation.
Clinicians may say embryo in the earliest weeks and fetus from about week 9. Gestational age anchors scheduling, counseling, and testing.
Critical windows and exposures, what timing means
Each organ has peak vulnerability windows. Very early folate insufficiency raises neural tube defect risk, early cardiac formation is sensitive in the mid first trimester, and limb development peaks in the same period. Later exposures tend to affect growth and function more than initial structure.
Common sources of risk, alcohol in the first trimester, certain medications and infections, and environmental toxins. If an exposure occurred, timing and dose guide next steps, often targeted screening or diagnostic testing with counseling.
Measuring growth, terms you see on ultrasound reports
Numbers on the screen can feel abstract at first. A quick glossary helps.
- The earliest and most accurate dating is crown rump length in the first trimester, often abbreviated CRL
- Growth metrics often include biparietal diameter BPD, head circumference HC, abdominal circumference AC, and femur length FL
- These feed formulas to estimate weight, referred to as estimated fetal weight EFW
- Fluid volume is checked using the amniotic fluid index AFI or a single deepest pocket
- Doppler flow studies, such as umbilical artery Doppler, evaluate placental resistance when growth concerns arise
Expect normal biological variation. Ultrasound weight estimates commonly have error in the range of plus or minus 10 to 15 percent, position and technique matter.
Organ systems, how they mature
Brain and nervous system
Neurogenesis, neuronal migration, synaptogenesis, and cortical folding overlap across pregnancy and after birth. Movements evolve from reflexive to organized, sleep and wake cycles emerge, and auditory pathways work by the second trimester, which supports response to familiar voices. Adverse influences like hypoxia, severe malnutrition, infection, or substance exposure can alter trajectories, timely care reduces risk.
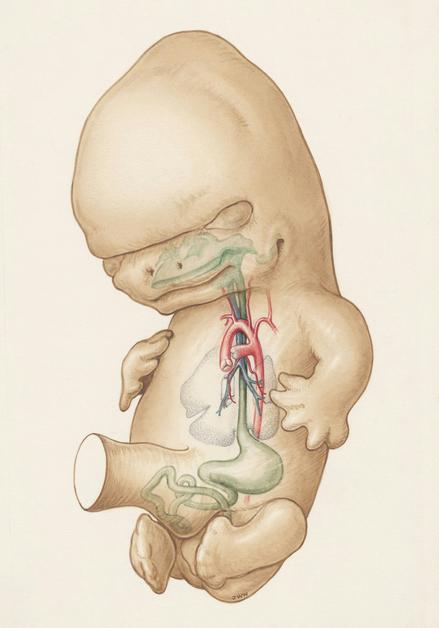
Heart and circulation
Cardiac morphogenesis builds four chambers and valves mainly in the embryonic period. Fetal circulation uses shunts, the ductus venosus, foramen ovale, and ductus arteriosus, to route oxygen rich blood to the brain and heart. At birth, lungs expand, shunts close, and circulation shifts.
Respiratory system and lung maturation
The lungs pass through embryonic, pseudoglandular, canalicular, saccular, and alveolar stages. Surfactant production rises through late preterm and term, making breathing possible after birth. Fetal breathing motions, and later practice breaths of amniotic fluid, support development.
Musculoskeletal growth and reflexes
Limb buds appear early, bones mineralize in the second trimester, muscle tone strengthens, and reflexes such as grasp and suck develop through the fetal period. Thumb sucking and fist clenching can be seen as neural circuits organize.
Gastrointestinal and renal systems
The gut rotates and differentiates, the fetus swallows amniotic fluid, which supports gut maturation and helps regulate fluid volume. Meconium forms in the bowel. Nephrogenesis occurs largely in the second trimester, and fetal urine becomes a major amniotic fluid source, so kidney health strongly influences volume.
Sensory systems and perception
Hearing responds by mid pregnancy, touch sensitivity increases with age, responses to gentle abdominal caresses may be noticed, light sensitivity rises later in pregnancy. Flavors in amniotic fluid may shape later preferences, an early preview of taste learning.
Placenta, cord, and fluid
The placenta is the interface for gas and nutrient exchange and an endocrine organ producing hCG, progesterone, and human placental lactogen. The umbilical cord contains two arteries and one vein cushioned by Wharton jelly. Amniotic fluid protects and supports growth, measured clinically by AFI or maximum vertical pocket.
Monitoring, screening, and tests you can expect
Routine ultrasound schedule
- First trimester, dating scan, and nuchal translucency screening when chosen
- Second trimester, the detailed anatomy scan around 18 to 22 weeks checks structures head to toe and placental location
- Third trimester, selective growth scans for indicated reasons like hypertension, diabetes, reduced movement, or growth concerns
Screening versus diagnostic testing
- Screening tests, such as noninvasive prenatal testing NIPT and the combined first trimester test that includes nuchal translucency NT, estimate risk for common chromosomal conditions, they do not give a definitive answer
- Diagnostic tests, chorionic villus sampling in the first trimester or amniocentesis after 15 weeks, provide chromosomal and genetic information with a small procedure related risk
Functional monitoring, movement, NST, and BPP
- Kick counts, many clinicians suggest counting movements from 28 weeks onward, for example 10 distinct movements within two hours, a sustained reduction deserves prompt contact with your care team
- Nonstress test, NST, evaluates fetal heart rate responses to movement
- Biophysical profile, BPP, combines NST with ultrasound checks for movement, tone, breathing motions, and amniotic fluid
Advanced imaging and specialist assessments
- Fetal echocardiography for suspected or high risk cardiac conditions
- Doppler ultrasound studies of the umbilical artery and middle cerebral artery for placental resistance and fetal anemia or blood flow redistribution
- Fetal MRI to clarify complex brain or thoracic findings when ultrasound views are limited
Growth assessment and interpreting deviations
Birth weight percentiles and serial ultrasound growth curves help distinguish symmetric from asymmetric patterns. Abnormal trends prompt closer follow up, Doppler assessment, and consultation with maternal fetal medicine.
Factors that shape fetal development
Genetics and prenatal screening
Genetics influences the pace and quality of fetal development, and chromosomal variations can occur in any pregnancy. Screening supports early identification and guides decision making about follow up tests and consultations.
Nutrition, supplements, and daily habits
Balanced nutrition with folate, iron, iodine, calcium, vitamin D, and omega 3 fatty acids supports organ formation and later maturation. Prenatal vitamins help cover gaps, discuss any additional supplements with your clinician. Avoid alcohol and tobacco, and review prescription, over the counter, and herbal medications for safety. Practical add ons, adequate sleep, gentle activity if approved, and vaccinations per national guidance.
The role of ongoing prenatal care
Regular prenatal visits and timely imaging are a window into fetal development, they catch variations early and reassure when progress is steady. Authoritative resources include ACOG, WHO, CDC, and major academic centers such as Mayo Clinic, Johns Hopkins, and Cleveland Clinic.
Common variations, complications, and when to seek care
Early pregnancy loss
Miscarriage is most common in the first trimester and is frequently due to chromosomal anomalies. Care may include emotional support, follow up, and evaluation for recurrent loss when indicated, along with counseling about future pregnancies.
Growth disorders and fetal compromise
Intrauterine growth restriction, also called fetal growth restriction, can arise from placental insufficiency, maternal disease, or fetal conditions. Surveillance uses serial growth scans, Doppler studies, and thoughtful timing of delivery that balances maturity with the risks of continuing the pregnancy.
Preterm birth and developmental consequences
Preterm birth risk increases with certain medical or obstetric factors. Outcomes vary with gestational age, earlier deliveries carry higher risk for respiratory and neurologic challenges. Preventive strategies and antenatal corticosteroids for threatened preterm birth improve respiratory outcomes.
Structural anomalies
Many structural conditions are first seen on the anatomy scan. When detected, referral to genetics and maternal fetal medicine supports specific imaging, diagnostic testing, and discussion of care options before and after birth.
Placental, cord, and fluid conditions
Placenta previa, placental abruption, velamentous cord insertion, and fluid abnormalities like oligohydramnios or polyhydramnios have distinct evaluation and management plans. Clear communication about monitoring and delivery timing helps align decisions with safety.
Interventions and referrals that support outcomes
Maternal medical optimization
Managing diabetes, hypertension, thyroid disease, asthma, and other conditions can reduce risk to the fetus. Medication plans aim to maintain maternal health while minimizing fetal exposure when alternatives exist.
In utero therapies and fetal procedures
Selected conditions have options such as intrauterine transfusion for fetal anemia, shunts for certain obstructive lesions, fetoscopic laser for twin to twin transfusion syndrome, and specific fetal surgeries. These are performed in specialized centers with careful counseling about potential benefits and risks.
When to involve specialists
Refer to maternal fetal medicine or neonatal specialists for growth restriction, complex structural anomalies, suspected fetal compromise, or when advanced testing and procedures are being considered.
Fetal behavior, senses, and early learning
Movement, hiccups, and sleep states
Movement begins as simple reflexes, then becomes organized with identifiable sleep and wake cycles. Hiccups are common and reflect diaphragm activity. Variation is expected, a sustained reduction calls for evaluation.
Hearing, vision, and touch
By mid pregnancy the fetus responds to sound, and later can recognize repeated elements of the maternal voice. Light sensitivity increases near term. Touch sensitivity rises across pregnancy with more coordinated responses to gentle pressure.
Early learning and bonding
Repeated sensory exposure, voices, rhythms, flavors in amniotic fluid, may shape preferences after birth. Speaking, singing, or reading aloud, low risk and potentially calming for both you and your baby.
Language choices that support both science and clarity
Parents often search for terms like fetal growth, prenatal development, ultrasound in pregnancy, pregnancy milestones, placenta, umbilical cord, amniotic fluid, neural tube, fetal heart rate, and lung development. Using these terms, paired with parent friendly explanations, improves readability and discoverability. Clear pairing also helps clinicians and families stay aligned at appointments.
Bringing it together, an empowering perspective
You might ask, what matters most for my family right now. The short list is clear, know your dates, show up for screening and anatomy evaluation windows, maintain healthy daily habits, watch movements in the third trimester, and speak up early if something feels off. Small steps compound.
Fetal development is a continuous, awe inspiring process. The more you understand, the more confident you become in your decisions, and the easier it is to ask for the right help at the right time.
Key takeaways
- Fetal development progresses through germinal, embryonic, and fetal stages, timing shapes screening, imaging, and sensitivity to exposures
- The first trimester emphasizes organ formation and early screening, the second trimester focuses on growth and sensory development, the third trimester brings brain and lung maturation and birth readiness
- Core measurements include CRL, BPD, HC, AC, FL, and EFW, fluid is assessed with AFI, and Doppler studies help evaluate placental resistance
- Screening tests such as NIPT and NT estimate risk, diagnostic tests like CVS and amniocentesis provide definitive genetic information
- Kick counts from 28 weeks support awareness of well being, a persistent reduction deserves prompt contact with your care team
- Balanced nutrition, smart medication review, smoke and alcohol avoidance, vaccinations, and regular prenatal care all support healthy fetal development
- There are caring professionals and reliable resources to guide you, including ACOG, WHO, CDC, and major academic centers, and you can download the application Heloa for personalized tips and free health questionnaires for children
Fetal development, repeated often and understood well, turns uncertainty into informed action, steady, compassionate, and science aligned.
Questions Parents Ask
When can I hear the fetal heartbeat?
You may see cardiac activity on an ultrasound as early as 6–7 weeks. Hearing it depends on the method: a handheld Doppler at the clinic often detects a heartbeat around 10–12 weeks (sometimes earlier or later depending on fetal position and body habitus), while a stethoscope or fetoscope usually works after about 17–20 weeks. Home Dopplers vary widely in reliability and can increase anxiety if you can’t find a sound—don’t hesitate to ask your care team to check during a visit instead. If you’re worried about the heartbeat at any point, contact your clinician for a timely check.
Which prenatal vitamins and supplements matter, and when should I start them?
Starting key nutrients before conception or as soon as you know you’re pregnant helps support early development. Commonly recommended components include:
- Folate (folic acid) — to reduce neural tube risk; usual preventive doses start around 400–800 µg daily, with higher doses sometimes advised for specific risk situations (discuss with your clinician).
- Iron — supports maternal blood volume and fetal iron stores; needs vary, and a blood test can guide the right amount.
- Iodine, vitamin D, calcium, and omega‑3 (DHA) — each supports specific aspects of growth and brain development.
A standard prenatal multivitamin covers many of these needs, but individual recommendations depend on diet, health conditions, and blood tests. Try to review supplements and medications with your care provider to personalise what’s best for you and the baby.
What causes reduced fetal movement, and when should I seek care?
Reduced movement can have simple explanations: normal fetal sleep cycles, the baby’s position, a posterior placenta, or the effects of maternal activity or medication. Still, a sustained decrease in your baby’s usual activity deserves prompt attention. A practical check is to sit quietly at a time when the baby is normally active and note distinct movements—many clinicians use a target of about 10 movements within two hours, though patterns vary. If you notice a clear and lasting reduction, contact your care team right away. They will usually assess with fetal heart monitoring (NST) and may add an ultrasound or biophysical profile to make sure everything is reassuring. It’s always better to ask early—most evaluations are reassuring, and quick checks provide real peace of mind.
Further reading :
- Fetal development: MedlinePlus Medical Encyclopedia (https://medlineplus.gov/ency/article/002398.htm)
- Fetal development: The first trimester (https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-care/art-20045302)
- Critical Periods of Development – MotherToBaby | Fact Sheets (https://www.ncbi.nlm.nih.gov/books/NBK582659/)









