Bringing a new life into the world—a profound journey, layered with wonder, curiosity, and at times, a swirl of worries only a parent can know. The marvel that is fetal development extends far beyond biology—it weaves together anticipation, maternal wellbeing, a dash of scientific precision, and more than a little hope. What exactly happens inside your womb as weeks turn to months? How do early choices shape the future of your baby’s health? Are growth patterns on track? From that fleeting first heartbeat to the complex choreography of tiny organs growing, each phase carries its own blend of possibilities and questions. And yes, knowing the medical milestones—along with practical steps—adds a welcome sense of reassurance. Let’s unravel these stages, highlight what’s happening each week, and decode all those clinical terms that sometimes feel like a foreign language.
The stages of fetal development: from a single cell to a thriving newborn
The journey of fetal development is almost poetic in its complexity. Everything begins at fertilization, when a single microscopic zygote forms, brimming with genetic instructions. This cell divides, multiplies, and differentiates at astonishing speed—quickly becoming much more than the sum of its parts. Should we break it down?
- Germinal stage (conception to implantation): Imagine a tiny bundle of promise—rapidly multiplying cells drifting down the fallopian tube, searching for their new home in the uterus. Here, the placenta quietly begins its foundational work, setting up critical support systems.
- Embryonic stage (about weeks 3–8): This is when the scene gets intense. Major organs—brain, heart, spinal cord, limbs—begin to take shape in a process called organogenesis. The neural tube, which becomes the brain and spinal cord, seals up. Limb buds, heartbeats, emerging facial features: all appear in quick succession. Vulnerability to harmful substances (teratogens) is highest during these weeks.
- Fetal period (week 9 onward): The transformation continues but shifts focus from basic assembly to fine-tuning. Brains wire up, organs mature, muscles flex, skin thickens. Your baby gains both length and weight—even practices swallowing and “breathing” movements as the lungs develop. All roads lead here: preparing for life beyond the womb.
Week-by-week timeline: what’s new each week?
Weeks 1–4: beginnings, cell division, and first connections
Bright beginnings—the union of egg and sperm sparks a journey. By week 4, a gestational sac may show up on an ultrasound—tiny, yet signaling unmistakable progress. At this point, the embryo is smaller than a poppy seed, establishing connections for nutrient and oxygen supply. Division and implantation take center stage, while maternal hormones like hCG nurture the environment for growth.
Weeks 5–8: the heart starts to beat, organogenesis in motion
Here’s where things accelerate. By week 6, you might catch a flicker—cardiac activity on the ultrasound—tiny heart chambers pulsing away. Neural tube closure (a critical step protected by folate), the earliest limb formations, and early facial features take shape. The phrase “embryonic period” truly shines now; this is a sensitive window, especially to toxins or medication. It’s worth highlighting: supplementing with folate and avoiding known teratogens now is especially protective.
Weeks 9–12: reflexes, growth spurts, and shifting toward the “fetal” stage
You’ll see a shift: the basic framework is set, and now organs begin to mature. Reflex movements (think of those tiny kicks you won’t feel just yet) start to emerge. Genital differentiation kicks in, and limb structures become increasingly refined. By week 12, your baby measures the size of a lime—amazing, right? First trimester screenings, including nuchal translucency and specialized blood tests, are often performed at this window.
Weeks 13–20: new facial features, rapid growth, sensory prep
Ready for detail? Eyebrows, lanugo (that charming downy hair), and bony frameworks become visible. Bones begin to harden; facial features become distinct—this is when curious parents might catch those tiny profile images on ultrasound. Many begin to feel gentle flutters (quickening) as baby’s early activity grows. A creamy substance called vernix caseosa starts to protect your baby’s skin.
Weeks 21–28: first sounds, surfactant, and sleep cycles
Now, the lungs undergo major architectural changes, laying down airways and starting to produce surfactant (the magic fluid that helps with breathing after birth). The senses awaken—your baby might respond to music or a familiar voice. Movements are more coordinated, and sleep–wake cycles appear. Brain growth is supercharged.
Weeks 29–36: growing strong—weight, brain folds, and coordination
Rounding the curve into late pregnancy, babies steadily gain weight. Subcutaneous fat accumulates, and the coordination of sucking and swallowing matures. Brain architecture—those lovely folds and grooves—becomes more intricate. Fetal movement tracking becomes a practical tool for parents.
Weeks 37–40+: preparing for the outside world
Final touches—lungs mature, organs ready for life outside the womb, and most babies settle head-down. This is the home stretch where everything gears up for birth—your baby “practices” breathing amniotic fluid, building muscle for those first breaths.
How is fetal development measured? Biometry and ultrasound explained
Ever wondered what clinicians mean with abbreviations like CRL, BPD, or EFW? Here’s the lowdown:
- Crown–rump length (CRL): Used in early pregnancy (first trimester) for the most accurate dating—measured from the top of the baby’s head to the bottom.
- Biparietal diameter (BPD), head circumference (HC), abdominal circumference (AC), femur length (FL): These four become the go-to metrics for tracking fetal growth mid-to-late pregnancy. Formulas combining them estimate baby’s weight (EFW).
- Fundal height: The doctor may still run a measuring tape over your abdomen, but ultrasound provides more detail, especially when growth seems off-track.
Clinical pearls: Growth restriction can be “symmetric” (all parts equally affected) or “asymmetric” (abdominal size lags), and management varies. Serial ultrasounds, Doppler studies for blood flow, and growth charts help tailor ongoing care.
Organ system development: how does each part grow?
Brain and nervous system
Neurogenesis (birth of nerve cells), synaptogenesis (connections), and ongoing brain folding: these processes all start early and keep evolving, well into infancy. The development is continuous—delicate but also astonishingly adaptive. If oxygen or nutrients become scarce, or if an infection occurs, there can be lasting effects, but many influences are modifiable, especially with good medical care.
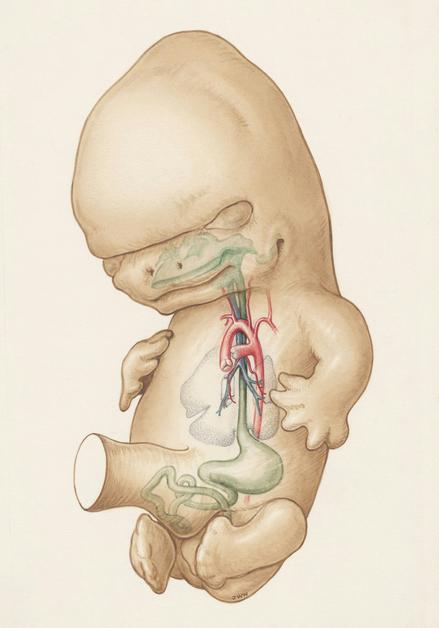
Heart and circulation
Four chambers organize, fetal shunts (ductus venosus, foramen ovale, ductus arteriosus) guide blood away from yet-to-function lungs, diverting oxygen-rich blood to the brain and heart. These shunts close dramatically at birth as the baby takes those first breaths.
Lungs and breathing
From tiny airways to mature alveoli, fetal lungs pass through several stages. Production of surfactant (to keep the lungs open) begins in earnest late in the second trimester—a key factor in survival for early preterm babies. When preterm birth seems likely, doctors often recommend corticosteroids to speed up this process.
Bones, muscles, reflexes
Early “limb buds” transform into coordinated, strong arms and legs. Bones ossify (harden), while suck and grasp reflexes develop. It’s common to spot a baby sucking a thumb on a scan—preparing for feeding after birth.
Digestion and kidneys
Structural changes abound: the intestines loop and rotate, and by the late second trimester, swallowing and digestive movements mature. Kidneys finish key steps in nephron development, and fetal urine turns into the main source of amniotic fluid.
Senses and perception
- Hearing: Responds to external sounds by about mid-pregnancy; heartbeat and digestion noises are familiar.
- Touch: Increases with time; gentle abdominal pressure or mom’s voice might trigger a response.
- Vision: Eyes develop early, but actual functional sight only matures after birth.
- Taste and smell: Flavors from mom’s diet seep into the amniotic fluid, laying the groundwork for future food preferences.
Placenta, cord, amniotic fluid
Placenta delivers oxygen, nutrients, and hormones like hCG or progesterone. The umbilical cord—two arteries, one vein, all cocooned in Wharton’s jelly—acts as the baby’s supply line. Amniotic fluid offers a protective cushion; both low and high levels guide further tests or attention.
Monitoring fetal development: from ultrasounds to movement counts
- Dating scan (usually 6–12 weeks): Confirms gestational age, checks for multiples.
- Nuchal translucency (11–14 weeks): Screens for chromosomal risks.
- Anatomy scan (18–22 weeks): Evaluates structure and growth.
- Growth scans and Dopplers (as indicated): Track size, blood flow, and amniotic fluid.
- Kick counts (from 28 weeks): Track 10 movements in 2 hours, especially if patterns change.
- Non-stress test (NST), biophysical profile (BPP): For pregnancies with added risks—assesses fetal well-being.
Advanced imaging, like fetal echocardiography or MRI, may be recommended for particular concerns, such as suspected heart or brain anomalies.
What influences fetal development? Genes, habits, and medical care
- Genetics: The blueprint that starts development, but also can introduce certain variations or risks. Routine prenatal screening helps parents understand possibilities—from Down syndrome to other chromosomal conditions.
- Nutrition: A balanced diet—rich in protein, vitamins, iron, iodine, and especially folate—is essential. Deficiencies, particularly in the first trimester, impact structure and later function.
- Environmental exposures: Alcohol, tobacco, prescription or herbal drugs (some of which might seem harmless) can all affect the developing baby. Open conversations with your care team are essential to making safe choices.
- Maternal health: Managing chronic illnesses—hypertension, diabetes, thyroid disorders—steers the odds towards better outcomes.
When things don’t follow the script: Variations, complications, and proactive care
- Early pregnancy loss: First-trimester miscarriages often trace back to chromosomal anomalies rather than anything a parent could avoid. Support, follow-up, and individualized counseling support recovery and planning.
- Growth concerns: Growth restriction (IUGR/FGR), possible macrosomia (large baby), or amniotic fluid concerns all call for tailored monitoring—serial scans, Doppler studies, sometimes expedited delivery.
- Preterm birth: Emerging before 37 weeks means more careful monitoring for lung, feeding, or neurologic immaturity. Antenatal corticosteroids, gentle feeding, and sometimes extra hospital care step in to boost the baby’s start.
- Structural anomalies: Detected mainly at anatomy scan, these findings prompt referral to genetics specialists. Further imaging, diagnostic options, and open discussion about management and outcomes support informed choices.
- Placenta and cord issues: From low-lying placenta to velamentous cord insertion, timely detection and follow-up matter. Management plans aim for safety of mother and child.
Maternal and fetal interventions: Optimising outcomes together
- Medical optimisation: Managing preexisting conditions, reviewing medications, and targeting therapy to minimize fetal exposure when options exist.
- In-utero therapies: Sometimes, direct treatment is possible—even before birth—such as blood transfusions, shunt placements, or laser procedures for particular twin complications. These advanced steps involve careful counseling and referral to specialist centers.
Fetal behaviour, senses, and the first steps in learning
- Movement: Early jerks slowly evolve into coordinated kicks, stretches, and hiccups. Changes in usual patterns often merit a discussion with your care provider.
- Sensory experience: Babies are surprisingly responsive—recognizing patterns, reacting to voices, and, unknowingly, starting the journey of learning and bonding even before birth.
- Bonding rituals: Speaking or singing to your bump isn’t just poetic; repeated exposure trains memory and preference, and supports emotional closeness.
Key takeaways
- Fetal development is a continuous process with recognizable milestones—each week brings unique changes that can be seen, measured, or sometimes felt by expectant parents.
- The sequence moves through the germinal, embryonic, and fetal periods—each with its own focus, from core structure building to advanced organ maturation.
- Major milestones include: early heartbeat (6–7 weeks via ultrasound), rapid brain growth, sensory system awakening, weight gain, and readiness for birth.
- Monitoring progression includes regular scans, blood tests, and kick-counts, tailored to both reassurance and detection of possible concerns.
- Choices matter—nutrition, medical conditions, supplements, and avoiding harmful exposures help tip the scales towards healthier outcomes.
- Support is all around: from medical teams to digital tools like the Heloa app, which provides personalised advice and child health questionnaires for free.
Questions Parents Ask
When can I hear the fetal heartbeat?
That soft, rhythmic thud on the ultrasound—often visible as early as 6–7 weeks—marks a major emotional milestone. Most clinics can find it with a handheld Doppler by 10 to 12 weeks, though sometimes it needs a little patience (especially with changing fetal positions). Stethoscopes or fetoscopes usually work after 17–20 weeks. Home Dopplers? They can be frustratingly inconsistent, so it’s always okay to ask your care provider instead.
Which prenatal vitamins and supplements matter the most, and when should I start?
Beginning before conception or as soon as pregnancy is confirmed works best for core nutrients. Think:
- Folate (folic acid): Shields against neural tube problems. 400–800 µg daily is standard, higher for specific risks (confirm with your clinician).
- Iron: Vital for blood volume and ensuring baby’s stores are built up.
- Iodine, vitamin D, calcium, omega‑3 (DHA): Each contributes, whether for brain power or bone strength.
Most prenatal multivitamins offer excellent coverage, but specific needs depend on health, diet, or lab test results.
What causes reduced fetal movement, and when should I check with my provider?
Fetal movement can fluctuate for many normal reasons: sleep cycles, baby’s position, even placental placement. Sometimes, activity seems quiet if you’re busy or less attentive. But a sustained dip or clear change deserves attention. Try sitting quietly when your baby is usually active; notice the time for 10 distinct movements (usually within 2 hours after 28 weeks). If you notice a persistent slowdown, don’t wait—clinicians usually respond with monitoring (NSTs, ultrasounds) for reassurance. Early checks, quick reassurance: often, that’s all you need.
Let fetal development be a source of fascination, knowledge, and calm as you journey through pregnancy—one week, one heartbeat at a time.
Further reading :
- Fetal development: MedlinePlus Medical Encyclopedia (https://medlineplus.gov/ency/article/002398.htm)
- Fetal development: The first trimester (https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/prenatal-care/art-20045302)
- Critical Periods of Development – MotherToBaby | Fact Sheets (https://www.ncbi.nlm.nih.gov/books/NBK582659/)









