Endometriosis. The word alone can trigger an avalanche of questions—especially if you’re a parent concerned for your daughter or simply eager to untangle the mysteries of reproductive health. You notice her doubling over from intense cramps, or perhaps struggling with relentless fatigue. Is it normal, or could something deeper be at play? If your instinct is to seek answers, you’re not alone. Endometriosis impacts an estimated one in ten women of reproductive age and can cast its shadow over adolescence, work, family planning, and emotional well-being. How does this invisible condition take shape? Why does it hurt in so many unpredictable ways? Most of all: what can you do right now, as a parent, to offer reassurance and guidance? A deep dive awaits—exploring medical foundations, warning signs, modes of diagnosis, strategies for support, and the advances in science that offer hope for tomorrow.
What Actually Is Endometriosis?
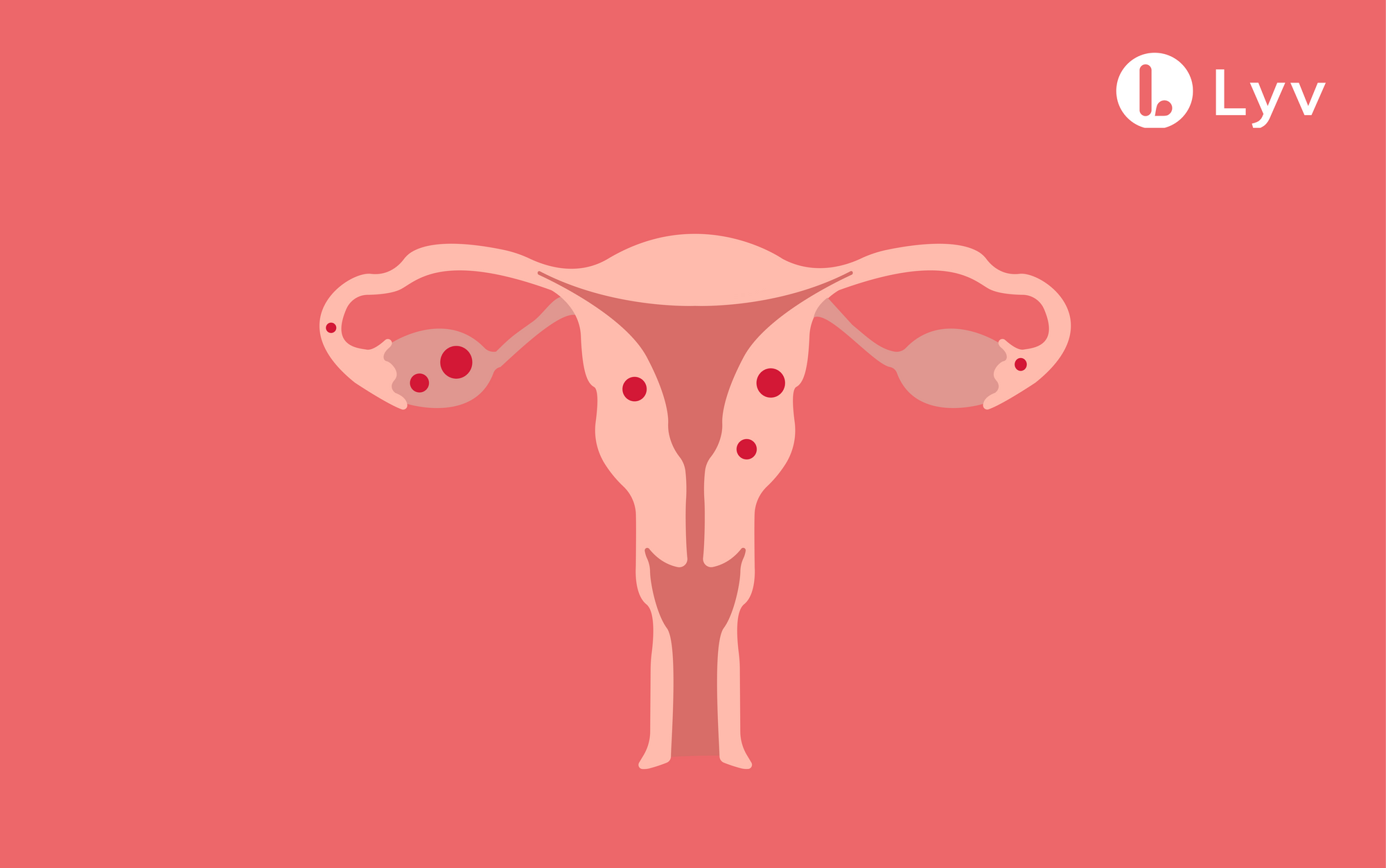
Imagine tissue behaving like a wayward mimic. Endometrial tissue—which should line the inside of the uterus—begins growing in places it simply doesn’t belong: on the ovaries, around the pelvic cavity, in rare cases even the lungs or intestinal tract. Ruled by hormones, this tissue swells and bleeds during each menstrual cycle. Yet, with no natural escape like menstruation provides, it triggers a cascade—inflammation, adhesions (bands of scar tissue), and the formation of chocolate-colored cysts called endometriomas. Over months and years, the impact multiplies: pelvic pain becomes a recurring guest, fertility may falter, and daily rhythms can be disrupted at unexpected turns.
But every case writes a different story. Endometriosis can lurk silently for years, or it can trumpet its presence from the very first periods of adolescence. Family history, genetics, and environmental factors each add a twist to the plot. Early diagnosis is rare; delays of seven to ten years aren’t unusual. So how should vigilant parents distinguish warning signs from normal growing pains?
The Many Faces and Types of Endometriosis
Medical science outlines several distinct forms—different shapes that endometriosis can take:
- Superficial peritoneal lesions: Tiny, scattered spots on the abdominal lining, often invisible to the eye or imaging.
- Deep infiltrating endometriosis: Lesions burrowing beneath the surface, sometimes invading vital organs—the bladder, rectum, or vagina—and producing amplified pain or bowel/bladder symptoms.
- Ovarian endometrioma: Blood-filled cysts, notorious for clinging to ovarian tissue and frustrating natural conception.
Variants abound, depending on precise location—bowel endometriosis (digestive symptoms), bladder endometriosis (urinary pain), and even lesions that settle into surgical scars after C-sections. The medical vocabulary is daunting, but the message is straightforward: endometriosis is a shapeshifter, rarely looking the same twice, and can co-exist in several forms within the same individual.
Who Is at Risk—And When?
Here’s a question that lingers in many parents’ minds: how early can endometriosis announce itself? For some, the trouble starts with the first periods—pain so intense it overshadows school and friendships. Yet the road to recognition can be serpentine, with many brushing off symptoms as “normal.” Factors tipping the odds include:
- Early onset of menstruation (before age 11)
- Long or heavy periods
- Never having given birth (nulliparity)
- Family history (a close relative with the diagnosis)
- Certain ethnic backgrounds (some populations experience delayed diagnosis due to healthcare disparities)
While most common in women of reproductive years, rare cases arise before puberty or continue into menopause. Ask yourself: is period pain interfering with life, or does it resist over-the-counter medications? If so, it may be time to dig deeper.
Symptoms: Listening to the Body’s Signals
No two experiences with endometriosis are identical. One teen may report “just” heavy periods, while another endures pain during ovulation or intercourse that stubbornly refuses to abate. Some common warning signs to watch for:
- Severe pelvic pain—cyclical, persistent, sometimes radiating to the back or legs
- Pain that starts before menstruation and lingers, defying conventional painkillers
- Dyspareunia—discomfort during or after sexual activity, commonly overlooked in teens
- Digestive disturbances: cramping, bloating, diarrhea, or constipation
- Urinary or bowel pain—difficult urination, discomfort during bowel movements
- Chronic fatigue—energy drain beyond what seems logical for a busy schedule
- Difficulty conceiving—though not all with endometriosis face this, about 40% report significant fertility challenges
- Localized pain—especially if associated with previous surgical scars
Psychological effects are often hiding in plain sight: anxiety, withdrawal from social life, and a persistent undercurrent of stress. It can be tempting to underestimate these signs, chalking them up to puberty or stress, but tuning in—and taking complaints seriously—may open doors to quicker care.
Importance of Early Detection
Why does speed matter? With diagnostic delays averaging nearly a decade, untreated endometriosis can leave scars—both literal and emotional. Parents who lend an attentive ear, advocating for respectful investigation, offer threefold protection: averting lasting pelvic organ changes, reducing psychological distress, and smoothing the journey toward specialist help.
How Is Endometriosis Diagnosed?
Diagnosis unfolds in layers. It begins with attentive listening and a medical history that covers family background, symptom patterns, and broader health. Examinations may hint at tender areas or palpable masses, but especially for young people, physical signs can remain hidden. Transvaginal ultrasound often serves as the first line of investigation, particularly for ovarian cysts. MRI scans provide a more detailed map, especially for deep or complex forms.
Yet, the gold standard remains laparoscopy—a minimally invasive surgical procedure using a tiny camera, delivering direct visualization and sometimes immediate tissue sampling. Research continues apace, seeking biomarkers (detectable in blood or urine) that could someday allow for non-invasive screening, but for now, patience and persistence are required.
Theories Behind Endometriosis: Why Does It Happen?
While no single explanation exists, several prominent theories guide research and treatment:
- Retrograde menstruation: Menstrual fluid, rather than exiting via the vagina, flows backward through the fallopian tubes, seeding the pelvis with wayward endometrial cells.
- Immune system irregularity: A sluggish immune response may fail to clear stray tissue, allowing inflammation to persist.
- Genetic predisposition: A family member with endometriosis? Risk can climb significantly.
- Hormonal factors: The estrogen-dependent nature of the disease underscores the importance of monthly hormonal fluctuations in driving symptoms.
- Environmental exposures: Contact with endocrine-disrupting chemicals, such as those found in certain plastics or pesticides, may play a role.
Multiple factors likely interact, which is why endometriosis can emerge in those with very different backgrounds and health profiles.
Severity: Stages and What They Mean
Doctors reference four stages—from minimal to severe—based on lesion depth, number, and organ involvement:
- Stage I (Minimal): Scattered, superficial lesions
- Stage II (Mild): Greater number, some deeper tissue involvement
- Stage III (Moderate): Many deep lesions, the presence of endometriomas, maybe some scar tissue
- Stage IV (Severe): Widespread, deeply infiltrating lesions, dense adhesions, and substantial impact on organ function
Severity doesn’t necessarily match symptom intensity. Someone with stage I may suffer excruciating pain, while another with stage IV experiences only mild discomfort.
Complications and Associated Risks
The ripple effects of endometriosis extend beyond pelvic pain. Real risks include:
- Chronic, treatment-resistant pelvic pain
- Adhesions that twist or bind organs, complicating future surgery or conception
- Ovarian endometriomas—cysts prone to rupture and hormonal disruption
- Digestive and urinary tract symptoms, especially if lesions invade the bowel or bladder wall
- Rare, but possible: pulmonary (lung) complications during menstruation
- Slightly increased risks of ovarian cancer and related conditions like adenomyosis
- Emotional distress, with the cumulative weight of pain and uncertainty clouding work, friendships, and home life
These knock-on effects highlight the value of comprehensive care—physical, psychological, and social.
Endometriosis and Fertility: What Parents Should Know
For families pondering the future, fertility questions hover at the forefront. Estimates suggest 30% to 50% of those with endometriosis may face difficulty conceiving. Inflammation, distorted anatomy, and scarring can each block the intricate steps necessary for pregnancy. Even after successful conception, higher risks of miscarriage and complications persist. Regular check-ins with a gynecologist, open communication, and timely referrals to fertility specialists shift the odds in a positive direction.
Approaches to Treatment and Daily Living
No definite cure for endometriosis exists—yet relief and resilience are within reach. Management strategies reflect the diversity of individual needs:
- Hormonal therapies: Suppressing menstruation through oral contraceptives or progestins can ease pain and limit disease progression.
- Medical menopause: For refractory cases, inducing temporary menopause calms hormonal surges, though side effects mandate careful monitoring.
- Surgery: Excision or ablation (removal or destruction) of lesions, sometimes coupled with hysterectomy in select cases.
- Medication: NSAIDs address pain; newer drugs such as GnRH antagonists target hormonal pathways with increasing precision.
- Physical therapies: Gentle exercise, physiotherapy, acupuncture, and heat pads provide tangible relief for some.
- Reproductive assistance: In vitro fertilization (IVF) or intrauterine insemination (IUI) open new paths when natural conception proves difficult.
- Mental health support: Counseling, mindfulness, and peer groups counter isolation and build resilience
Long-term management demands a multidisciplinary approach: gynecologists, pain specialists, pelvic floor therapists, and psychologists collaborating. Every individual travels a unique pathway, with personal values and life plans steering decisions. Ongoing research continues to yield new therapies and advance personalized care.
Prevention and Early Support: Empowerment Before Problems Escalate
True prevention remains beyond reach, but certain factors—a history of pregnancy, breastfeeding, or long-term hormonal contraceptive use—may slightly lower lifetime risk. However, the cornerstone remains vigilance and prompt parental support: recognizing symptoms, validating lived experiences, and ensuring swift access to specialists. Early action prevents complications that can echo through adulthood.
The Battle Against Delayed Diagnosis
A sobering reality: average diagnosis takes seven to ten years. Why the gap? Cultural taboos, dismissive attitudes toward pelvic pain, and knowledge gaps play their part. Shifting the narrative means honoring young people’s complaints, fostering open family discussions, and eliminating stigma. Directing families to dedicated resources or advocacy groups accelerates positive change, breaks the silence, and shapes better health outcomes for the next generation.
Science Moving Forward: Hope on the Horizon
Recent years have brought optimism. Researchers chase after novel biomarkers, refine imaging technologies, and cultivate non-hormonal treatment alternatives. Integration of care—unifying gynecology, pain medicine, physiotherapy, and psychology—puts science and empathy hand in hand. Community education initiatives amplify awareness and encourage families to push for answers when doubt persists. Every new discovery broadens the promise of early detection, effective treatment, and a life not dictated by pain.
Key Takeaways
- Endometriosis is a stealthy, sometimes invisible condition that can start as early as adolescence, disrupting daily routines in unpredictable ways.
- Symptoms are multifaceted—pelvic pain, digestive troubles, urinary discomfort, fatigue, and emotional strain.
- Early, attentive intervention by parents accelerates diagnosis and lessens complications.
- Hormonal, surgical, and integrative therapies provide real relief, opening doors to fertility and emotional well-being.
- Scientific progress is tangible—with breakthroughs in biomarkers, imaging, medical therapy, and personalized multidisciplinary care underway.
- Resources and specialists are available: don’t hesitate to reach out for expert guidance.
For parents looking to support the health journey of their daughters—and themselves—knowledge is empowering. Trust your instincts. Listen actively. When questions arise, connect with medical professionals and credible resources. For practical guidance and free health questionnaires designed for children, you can download the Heloa app, a trusted companion for parents navigating the twists and turns of family health.
Questions Parents Ask
Can endometriosis occur in young girls and teenagers?
Yes, endometriosis can sometimes start early, even during the teenage years or just after puberty. Although it is often diagnosed in women in their twenties or thirties, painful or heavy periods that interfere with daily life—even in adolescence—can be linked to endometriosis. If your child experiences these symptoms, especially if pain persists despite usual remedies, don’t hesitate to reach out for medical advice. Early support can help avoid delays in care and offer your child much-needed reassurance.
Is endometriosis hereditary?
Endometriosis does tend to run in families. If a close relative, such as a mother or sister, has experienced the condition, the chances of developing endometriosis may be higher. However, genetics is just one piece of the puzzle—other elements such as environmental factors and immune system responses also play a role. If endometriosis is present in your family history, sharing this information with healthcare providers can be helpful for early recognition and support.
Can lifestyle or dietary changes help manage endometriosis symptoms?
While there’s no magic diet or specific lifestyle change that can cure endometriosis, some families notice that thoughtful choices bring a degree of relief. A balanced diet rich in fruits, vegetables, and whole grains, as well as regular gentle exercise, may ease discomfort for some individuals. Reducing stress, getting adequate sleep, and keeping a symptom diary can also make day-to-day management a bit smoother. Each person responds differently, so it’s important to try different approaches and see what brings comfort to your child. Always talk with your healthcare provider before making significant changes, so strategies are tailored and safe.
Further reading :