Sweating in the middle of the night, unpredictable mood swings, and conversations about bone health suddenly on the family agenda? If the term “hormones and menopause” feels more like the opening line of a riddle than a medical subject, you are far from alone. For parents juggling busy schedules, work obligations, and household dynamics, hormonal changes tied to menopause can raise a whirlwind of concerns. Is it hot flashes or just another fevered rush to the school run? Could sleep disturbances be hormonal, or simply the result of interrupted nights with little ones? Understanding what really happens during “hormones and menopause”, why bodies shift, and how to find balance amid it all can transform confusion into clarity—and maybe even empowerment. The journey through menopause is unique, yet the science is universal. What’s actually happening on the inside, and how can science-based strategies support everyday wellbeing? Here’s a deep dive for parents seeking clear answers, guidance, and reassurance as they navigate this vital life stage.
The Hormonal Landscape: Unraveling the Science of Menopause
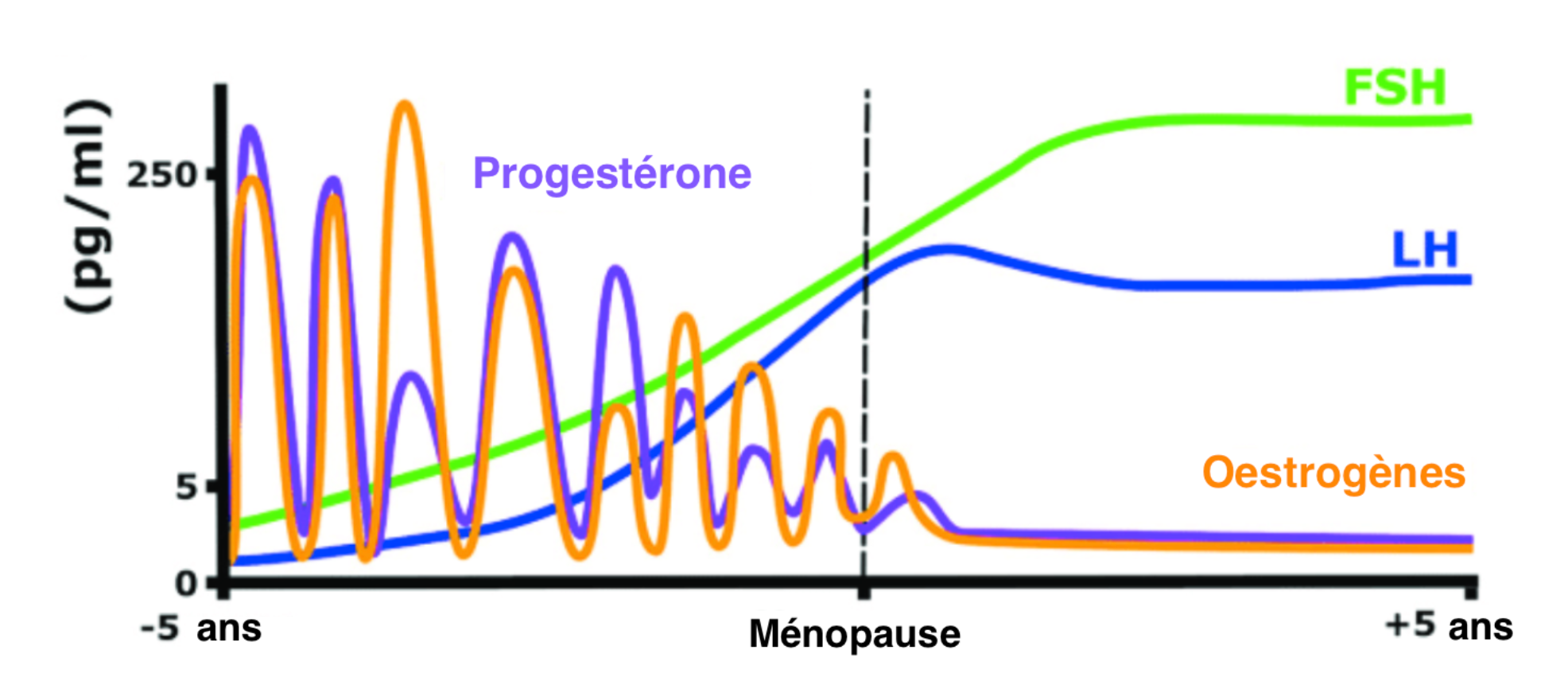
You’ve probably wondered: what causes the chaos of menopause, and how much is preordained by biology? At its core, “hormones and menopause” refers to the interplay of key chemical messengers—namely estrogen and progesterone—and a gradual shift in their levels as the ovarian reserve diminishes. Menopause, officially recognized when periods have stopped for 12 consecutive months, typically arrives around age 51, though genetics and lifestyle can tip the scales earlier or later.
Ovaries, once bustling with thousands of follicles, become less responsive to follicle-stimulating hormone (FSH) over time. As a result, estrogen production decreases. This decline, in turn, disrupts the hypothalamic-pituitary-gonadal axis, sending FSH and luteinizing hormone (LH) levels soaring. The result? Irregular, eventually absent, menstrual cycles. It’s a domino effect: as estrogen wanes, almost every system in the body feels the ripple—including the nervous, cardiovascular, and skeletal systems.
Beyond the textbook symptoms, the day-to-day impact is real. Hot flashes, those sudden surges of heat and sweat, stem from misfires in the brain’s temperature regulation (a direct hit from declining estrogen). Sleep becomes elusive, mood feels unpredictable, and a mysterious fatigue can settle in. The question, then, is not whether these changes happen, but why, and what to do about them.
Symptom Spectrum: What Shifts, What Stays, and Why It Matters for Parents
Every parent knows the value of predictability, yet “hormones and menopause” usher in a new era where rules change. Let’s explore the main zones of impact:
- Vasomotor Symptoms. Those infamous hot flashes and night sweats result from altered thermoregulation. Imagine your body’s thermostat breaking, flickering erratically—one moment freezing, the next drenched in sweat. These episodes often come with a flush, sometimes palpitations, and leave many parents feeling as though they hardly recognize their own skin.
- Urogenital Changes. Vaginal dryness, discomfort during intercourse, plus increased urinary urgency or frequency—these aren’t topics most parents anticipate discussing at the dinner table, but they’re rooted in thinning vaginal and urinary tract mucosa secondary to plummeting estrogen. Lowered estrogen also means diminished natural protection against urinary tract infections. While awkward to discuss, these symptoms are extremely common and deserve open, shame-free conversations.
- Skin, Hair, and Bones. Reduced estrogen means less collagen production and decreased skin elasticity. Fine lines may deepen, hair may thin or shift distribution, and the risk for osteoporosis—fragile, fracture-prone bones—rises. Because estrogen helps regulate calcium metabolism in bones, its decline accelerates bone resorption. Bone density screening (like DEXA scans) becomes an essential health tool.
- Mood and Sleep. Fluctuating levels of neurosteroids (hormones that affect neurotransmitters) contribute to shifts in mood, ranging from mild irritability to, in some, significant depressive symptoms. More than 40% of people in menopause report sleep disruptions; night sweats or insomnia challenge even the most organized parents. Notably, these symptoms can feed into each other in a feedback loop—poor sleep magnifies mood swings, which in turn impact sleep.
- Metabolism and Weight. Perhaps you notice weight creeping up or a shift toward central adiposity (“apple-shape”). Changes in fat distribution, slower metabolism, and increased insulin resistance combine with lifestyle stressors, making weight management more complex during menopause.
- Libido and Sexual Health. It’s not a myth—many report a dip in sexual desire, excitement, or satisfaction. While estrogen decline is partly responsible, psychological stressors, relationship dynamics, and self-image play significant supporting roles. The solution? Honest dialogues and, when needed, tailored medical advice.
Decoding Diagnosis: How Is Menopause Identified?
A common parental concern: “How do I know if it’s really menopause, and not something else?” The gold standard remains absence of menstruation for 12 straight months. Yet, when symptoms start before 45, or if the picture is unclear, checking hormone levels such as FSH (>30–40 IU/L) and low estradiol (<20 pg/mL) can be informative—though values may swing wildly in perimenopause.
Sometimes, doctors assess anti-Müllerian hormone (AMH) to evaluate ovarian reserve, but this isn’t routine. Other causes for missed periods—like thyroid abnormalities, polycystic ovarian syndrome (PCOS), or even pregnancy—require exclusion. When in doubt, medical evaluation ensures the right diagnosis and plan.
Hormone Replacement Therapy: Science, Safety, and Individual Choice
For many, the phrase “hormones and menopause” instantly triggers debates about Hormone Replacement Therapy (HRT). Is it safe? Effective? Necessary? Breaking it down:
- Estrogen-only HRT suits those who have had a hysterectomy.
- Combined estrogen-progestin HRT is preferred for those retaining a uterus, guarding against endometrial cancer risk.
- Bioidentical hormones mimic natural human hormones, yet compounded versions are not strictly regulated.
HRT effectively soothes vasomotor symptoms, genitourinary complaints, and bone loss. Yet, it’s not without risks: studies show a modest increase in breast cancer (especially with long-term, combined forms), and small rises in blood clot or stroke risk, particularly when started well after menopause or in high-risk individuals. Transdermal patches and gels are associated with lower risks relative to pills. The core message: timing, dose, and personal medical history matter. For some, non-hormonal treatments—SSRIs, SNRIs, gabapentin, or selective estrogen receptor modulators (SERMs)—may be preferable or necessary.
A genuinely personalized approach, led by open dialogue with healthcare professionals, ensures health decisions reflect individual risks and priorities.
Nutrition, Lifestyle, and Parental Wellbeing: Supporting Hormonal Harmony
Meeting the daily demands of parenting during hormone shifts is its own athletic feat. Proactive lifestyle choices can dramatically ease adjustments tied to “hormones and menopause”:
- Nourishing Diet. Choose calcium-rich foods to protect bones, vitamin D (think fatty fish, fortified milks, a dash of sunlight), plus phytoestrogens—natural plant compounds found in soy, flaxseed, and legumes—which may mildly support hormonal balance. Aim for a rainbow of vegetables, whole grains, and lean protein.
- Physical Activity. Weight-bearing exercises like brisk walking, resistance training, or dance classes not only bolster bone strength but also improve mood and metabolic health. Even brief activity breaks make a difference—consistency trumps perfection.
- Restorative Sleep. Regular sleep schedules, calming evening routines, cool and dark bedrooms, and limiting caffeine or alcohol can counter insomnia’s grip. If sleep issues persist, individualized support from a sleep specialist may help.
- Stress Reduction. Simple relaxation strategies—mindful breathing, meditation, or hobbies—support hormonal stability. Elevated cortisol levels amplify symptoms; managing stress can be transformative.
- Social Connection. Shared meals, family rituals, or support from other parents lend emotional resilience. Seeking professional advice (dietitians, mental health providers) is always wise for tailored recommendations.
- Avoid Smoking, Limit Alcohol. Both habits undermine bone, heart, and hormonal health. Reducing exposure matters at any stage.
- Family Awareness. Open conversations with partners, children, or loved ones foster empathy and understanding. When everyone’s informed, support flows more easily.
Emerging Treatments and Special Circumstances
The landscape of “hormones and menopause” management isn’t static. New therapies—such as SERMs (like ospemifene and bazedoxifene) and novel neurokinin 3 receptor antagonists (example: fezolinetant)—expand options with targeted, tissue-selective relief for specific symptoms. For people experiencing early menopause, especially following surgery (oophorectomy), abrupt hormone changes intensify risk for heart disease and osteoporosis—prompting earlier, sustained intervention with HRT or other modalities until the typical age of menopause.
Genetics, co-existing health conditions, and personal preferences shape every recommendation. Empathy—paired with cutting-edge science—remains the essential thread.
Andropause: The Male Perspective
While “hormones and menopause” are largely associated with women, attention sometimes turns to aging men. The term andropause occasionally surfaces to describe age-related declines in testosterone, but its medical validity remains debated. Some experience reduced libido, fewer morning erections, or erectile difficulties. However, these shifts are influenced by a broad interplay of health, lifestyle, and psychological factors, rather than a discrete hormonal ‘switch’ akin to menopause.
Hair loss may occur, but its roots are genetic as often as hormonal. Metabolic health—weight, cholesterol, and cardiovascular profile—merits monitoring for all parents as years advance.
Long-Term Health and Support: Strategy, Science, and Compassion
Regular health screenings transform worry into action. Bone density scans, lipid profiles for cardiovascular risk, and relevant cancer screening (mammograms, endometrial assessment) are powerful tools for prevention and peace of mind. Concerns about sexual health—whether lubrication, comfort, or intimacy—are thoroughly valid; options range from local estrogen to lubricants and specialist counseling.
Mental health remains paramount. If anxiety, mood changes, or cognitive shifts arise, compassionate and prompt support is available. The mix of hormonal, psychological, and social change can feel stormy—yet knowledge, resilience, and professional partnership make a tremendous difference.
Key Takeaways
- “Hormones and menopause” center around changes in estrogen, progesterone, and gonadotropins that touch nearly every aspect of health and daily routine for parents.
- Symptoms are highly variable, but each is a legitimate signal from the body, not a sign of failure or weakness.
- Most diagnoses hinge on clinical features—absence of menses, midlife onset, symptom constellation—with laboratory testing reserved for ambiguous or early presentations.
- Both hormone-based (HRT) and non-hormonal therapies offer meaningful relief, but decisions should always weigh individual health profiles, risk factors, and preferences.
- Optimal wellbeing rests on balanced nutrition, physical movement, restorative sleep, and steady stress management—tools fully within reach for busy families.
- Innovations in treatment, a multidisciplinary care team, and compassionate communication empower every parent facing the challenges of menopause.
- While aging brings hormonal changes for men, shifts are less abrupt and rarely rooted solely in testosterone loss.
- Lifelong learning, support networks, and trusted medical partners are valuable at every turn.
Resources, community support, and expert guidance are always at hand. For personalized tips and free health questionnaires tailored to your family, explore the Heloa app for practical support and advice right at your fingertips.
Questions Parents Ask
Can menopause affect memory or concentration?
Yes, it is common to notice changes in memory or concentration during menopause. Many parents report episodes of forgetfulness, difficulty focusing, or what some call “brain fog.” These changes are often linked to fluctuations in estrogen, which plays a role in cognitive function. If you experience these symptoms, rassurez-vous, they are typically temporary and tend to improve over time. Simple strategies like organizing your daily routine, taking notes, and practicing self-care can help. If memory problems are persistent or severe, seeking medical advice is encouraged.
Can menopause impact heart health?
Absolutely, menopause can influence heart health. The decrease in estrogen may increase the risk of cardiovascular issues such as high blood pressure or changes in cholesterol levels. It’s important to be attentive to your cardiovascular wellbeing at this stage. You can support your heart by eating a balanced diet, staying active, not smoking, and scheduling regular health check-ups. If you have concerns or a family history of heart disease, discuss them with your healthcare provider for personalized guidance.
How can I talk to my children about menopause?
Open communication is key. Explaining menopause to your children in age-appropriate language helps normalize the changes you are experiencing and can encourage empathy within the family. You might say something like, “Sometimes my body feels different as I get older—it’s completely natural, and nothing to worry about.” Answering questions honestly and reassuring your children that everything is okay supports an environment of trust. If you find it difficult, remember that it’s normal—many parents feel the same way. There are also books and online resources designed to help families discuss these topics together.
Further reading:









