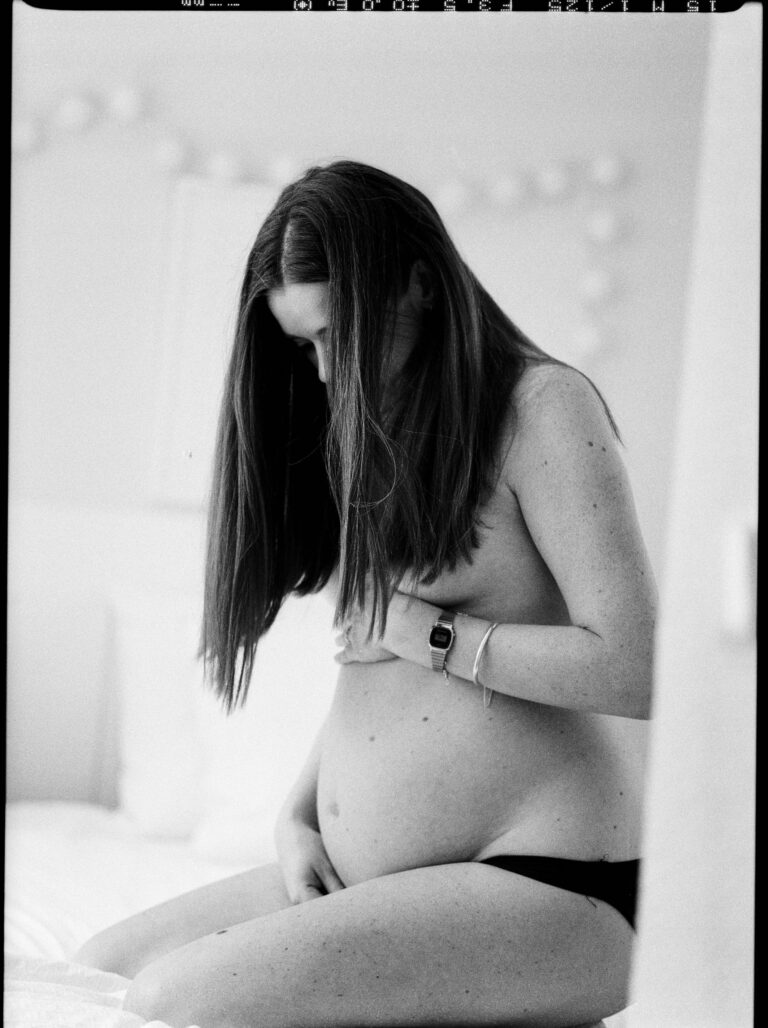
For new parents—whether this is your first encounter with the ribbons of new life or you already carry the echoes of previous labors—postpartum bleeding can spark a confusing swirl of questions and uncertainty. How much is too much? When is it still within the realm of normal, and when might it signal an issue that needs attention? The days and nights after birth are unique; they ripple with change, demand patience, and gently (or not so gently) nudge you into the world of postnatal recovery. Here, the focus shifts from dramatic delivery room moments back to the slow, methodical work of healing. The physical realities are unavoidable, but trust that important answers emerge when information is accessible, evidence-based, and tailored to your needs. Understanding postpartum bleeding, how it unfolds, and what patterns to expect, allows you to move forward with more confidence—and maybe even a little peace of mind.
Understanding Postpartum Bleeding: Facts for Recovery
Postpartum bleeding, or lochia, is the body’s brilliant yet messy way of returning to equilibrium. This vaginal discharge—melding blood, mucus, and sloughed uterine tissue—is entirely expected. Whether your baby arrived after a marathon of labor or through the swift hands of a cesarean section, your uterus enters its own performance, steadily contracting back to its original size.
Initially, postpartum bleeding may seem intense. You might be startled by its deep red color, the presence of small clots, or the slightly metallic tang of fresh blood. Over days, the discharge transitions: red to pink to pale yellow, a progression shaped by the different stages of lochia—lochia rubra, lochia serosa, and finally, lochia alba. Unlike a typical period, you’ll notice the volume and makeup shifting; activity like standing or breastfeeding can increase the flow for a moment, as oxytocin surges trigger stronger uterine contractions.
To fully grasp what’s happening, it’s helpful to spell out the physiological shifts. As soon as the placenta is delivered, your uterus begins the arduous process of shrinking—shedding the extra lining that nurtured your baby. What does that feel like? Sometimes, as dull cramps or “afterpains.” Sometimes, as nothing at all. These contractions might be sharper when nursing, brought on by the same hormone responsible for milk let-down.
The Three Stages of Lochia
Let’s clarify what you may see—and feel—by breaking down the three stages:
- Lochia rubra (days 1–4): Vividly red, with heavier flow. Small clots are common, but shouldn’t be larger than a small coin.
- Lochia serosa (days 5–12): A paler, rusty, or pink discharge. Blood mixes with a watery fluid known as serous exudate.
- Lochia alba (day 12 up to six weeks): The finish line. The flow lightens to a yellowish or creamy hue, evidence that healing is well under way.
Some days the bleeding may stop, only to surprise you anew after a walk around the house. This on-and-off rhythm is not unusual during the first two weeks, but never rush to abandon pads for regular underwear—you want to be ready if bleeding resumes.
Causes, Risk Factors, and Typical Patterns
Why does postpartum bleeding occur? In essence, it’s about uterine repair. Strong contractions pinch off blood vessels where the placenta was attached and prevent continued bleeding. These contractions can be amplified by breastfeeding, thanks to the hormone oxytocin. Most of the time, this process is smooth and self-limited, but sometimes complications emerge.
When might postpartum bleeding tip into abnormal territory? Here are key culprits:
- Uterine atony: The uterus fails to stay contracted, leading to excess flow.
- Trauma: Tears in the birth canal or surgical wounds may bleed persistently.
- Retained placental fragments: Tissue left inside the uterus interrupts healing.
- Coagulation disorders: Pre-existing blood clotting problems or certain medications can increase risk.
Higher risk is linked to previous hemorrhage, delivery by instruments or cesarean, very fast or very prolonged labor, abnormal placentas, and underlying conditions like obesity, anemia, or infection.
Distinguishing Normal from Concerning Bleeding
You’re likely asking: How will I know if postpartum bleeding is abnormal? First, notice the rhythm: heavy at first, tapering off, perhaps with brief increases after activity or nursing. Signs that suggest something is off—requiring immediate medical attention—include:
- Soaking a pad every hour for two or more consecutive hours
- Clots larger than a plum or golf ball
- Bleeding that turns bright red again after lightening
- Foul smell, fever exceeding 100.4°F (38°C), escalating pain, or new swelling
- Dizziness, rapid heartbeat, blurry vision, or overwhelming fatigue
Most of the time, these symptoms don’t occur. Still, knowing the warning signs empowers you to act swiftly when necessary.
Influencing Factors: Delivery, Lifestyle, and Medical Background
The amount and duration of postpartum bleeding are shaped by several factors:
- Type of birth: Vaginal birth usually leads to less blood loss (about 500 ml) compared to cesarean birth (roughly 1000 ml).
- Instrumental delivery: Forceps or vacuum extraction can elevate bleeding due to extra tissue trauma.
- Medical history: A past episode of hemorrhage, presence of fibroids, infections, clotting disorders, or certain medications can all increase risk.
Breastfeeding deserves special mention: while it sometimes triggers transiently heavier flow during feeds, over time it helps compress the uterus more effectively, ultimately reducing overall bleeding duration.
Hygiene and Home Management
Managing postpartum bleeding at home may seem overwhelming at first, but incorporating practical strategies can make a significant difference. Start with the right supplies—sanitary pads or dedicated postpartum underwear for about six weeks. Steer clear of tampons or menstrual cups until your provider gives the all-clear, as these can raise infection risk.
Other helpful practices:
- Change pads regularly and wash hands meticulously each time.
- Bathe or shower daily, rinse the perineal area with water, and gently dry.
- Choose cotton pads (if possible) to minimize irritation.
- Use a soft, pH-appropriate cleanser if your skin is sensitive.
- Ice packs soothe swelling; pain medication can be appropriate when recommended.
- Loose clothing, ample rest, and help from loved ones can ease physical recovery.
- Gentle activity such as walking is encouraged, but delay strenuous exercise or heavy lifting.
- Focus on iron-rich foods—for example, spinach, beans, eggs, fish, or lean meats—and remain hydrated. Iron supplements may be needed if tests reveal anemia.
Emotional Recovery and Societal Perspectives
Beneath the physical healing lies another sphere—emotional and psychological renewal. For some parents, postpartum bleeding is more than just a bodily event; it represents transition, sometimes isolation, and the beginning of a profoundly new identity. While past generations shrouded these weeks in secrecy, contemporary health advice encourages respect for individual experience, open communication, and support.
There’s no need to silence unwelcome feelings. If you’re feeling overwhelmed, anxious, or low in spirit, discussing these emotions with healthcare professionals or peer groups can bring relief and validation. Simple words, gentle encouragement, and allowing yourself time to heal—these are as essential as any physical remedy.
Assessing and Treating Abnormal Postpartum Bleeding
If postpartum bleeding deviates from the expected course, care teams employ several tools: visual inspections, tracking pad weights, vital sign monitoring, and pelvic examinations. Ultrasound is useful for detecting retained tissue. Blood tests may check for anemia or clotting problems.
In severe cases:
- Intravenous fluids or, if needed, blood transfusions restore volume.
- Uterine massage and medications like oxytocin or misoprostol coax contractions.
- Manual or surgical removal of retained tissue, or repair of injuries, is sometimes necessary.
- Rarely, more aggressive measures—such as a balloon to tamponade bleeding, arterial embolization, or even hysterectomy—are deployed.
Proactive care, such as administration of prophylactic oxytocin after birth, staff readiness, and monitoring, lower the risk of severe outcomes.
Complications Associated With Postpartum Bleeding
While most recoveries go smoothly, abnormal postpartum bleeding sometimes leads to medical complications like:
- Endometritis: Uterine infection requiring antibiotic therapy.
- Hematoma: Blood collection in tissue, causing pain or swelling.
- Blood clots: Potential for deep vein thrombosis or pulmonary embolism, especially with immobility.
- Shock, anemia, or organ injury: Consequences of major blood loss.
- Struggles with breastfeeding tied to low energy levels or reduced milk supply.
- Very rare events: uterine inversion, disseminated intravascular coagulation, or Sheehan syndrome (pituitary injury).
A history of such complications increases future risks, but with thorough follow-up and delivery planning, most parents enjoy full recovery and healthy experiences.
Tracking and Documenting Bleeding
Becoming your own health advocate means observing and recording the specifics. For parents, effective monitoring includes:
- Recording the pad type, quantity, and how quickly it’s saturated
- Noting changing discharge color (red → pink → yellow/white)
- Documenting clots—number and size
- Watching out for fevers, increasing pain, dizziness, or odor
A diary (digital or paper) or, as some suggest, photographs (if approved by your care provider) can sharpen your awareness. Sharing these details at appointments streamlines care and ensures personalized advice.
Recovery and Next Steps
After periods of heavy postpartum bleeding, fatigue and low energy aren’t uncommon. Recovery thrives on balanced nutrition, rest, hydration, and—when warranted—iron supplements. Tend gently to any stitches or scars, and wait for your provider’s confirmation before introducing anything inside the vagina to avoid infection.
If you’re experiencing breastfeeding difficulties, remember that blood loss can reduce milk supply and energy. Lactation consultants, when available, can offer much-needed support.
Emotional healing is just as important; the postnatal window opens space for rest, bonding, and even uncertainty. Naming your emotions, asking questions, and reaching out for help—whether informal or professional—will stir a smoother path through this transformative period.
Key Takeaways
- Postpartum bleeding is a typical, expected response to delivery, with variable patterns but predictable transitions in color and volume.
- Awareness of the distinctions between normal and abnormal postpartum bleeding has the power to decrease anxiety and foster timely, safer care.
- Promptly seek help for heavy bleeding, large clots, bad odor, fever, escalating pain, or any troubling symptoms.
- Consistent hygiene, pad changes, gentle routines, rest, and a nourishing, hemoglobin-boosting diet support speedy recovery. Iron supplementation can be needed if blood loss is significant.
- Document discharge characteristics and physical changes; share observations with your healthcare provider for individualized support.
- While complications are rare, swift intervention makes a world of difference.
- Postpartum recovery is inherently personal. Honoring your pace and seeking resources as needed will promote well-being in this vulnerable, hopeful season.
- Don’t hesitate to explore resources—for personalized health guidance and free child health questionnaires, you can download the Heloa application and step into parenthood with tailored, expert-supported advice.
Questions Parents Ask
How long does postpartum bleeding last after a cesarean section?
Postpartum bleeding after a cesarean section often follows the same pattern as after a vaginal birth, with lochia lasting around four to six weeks. However, the flow might be slightly lighter in the first days compared to a vaginal delivery. Some days may bring small fluctuations, especially if you become more active. If bleeding increases suddenly, if you notice large clots, or if there’s a foul smell, it is important to speak with your care provider. Every recovery is different, so trust yourself and check with your team if anything feels unusual.
Can breastfeeding affect postpartum bleeding?
Yes, breastfeeding can influence the pattern of postpartum bleeding. While nursing, the hormone oxytocin is released, which helps the uterus contract and may cause temporarily heavier bleeding during or right after feeds. Over time, these stronger contractions generally help the uterus heal faster, often shortening the overall length of bleeding. If you observe an increase in bleeding each time you breastfeed, sachez que cela est habituel—mais restez attentive aux signes inhabituels, comme une odeur désagréable ou des saignements très abondants.
What should I do if postpartum bleeding returns after it has stopped?
If bleeding revives briefly after it settled, especially after being more active, this is typically a natural sign that your body asks for more rest. You can try to slow down and allow more recovery time. However, if the bleeding becomes suddenly heavy, turns bright red again, or is accompanied by pain, fever, or a bad smell, do not hesitate to reach out to your healthcare provider. It is always reassuring to ask for professional advice if you feel uncertain—listening to your body is essential.
Further reading: