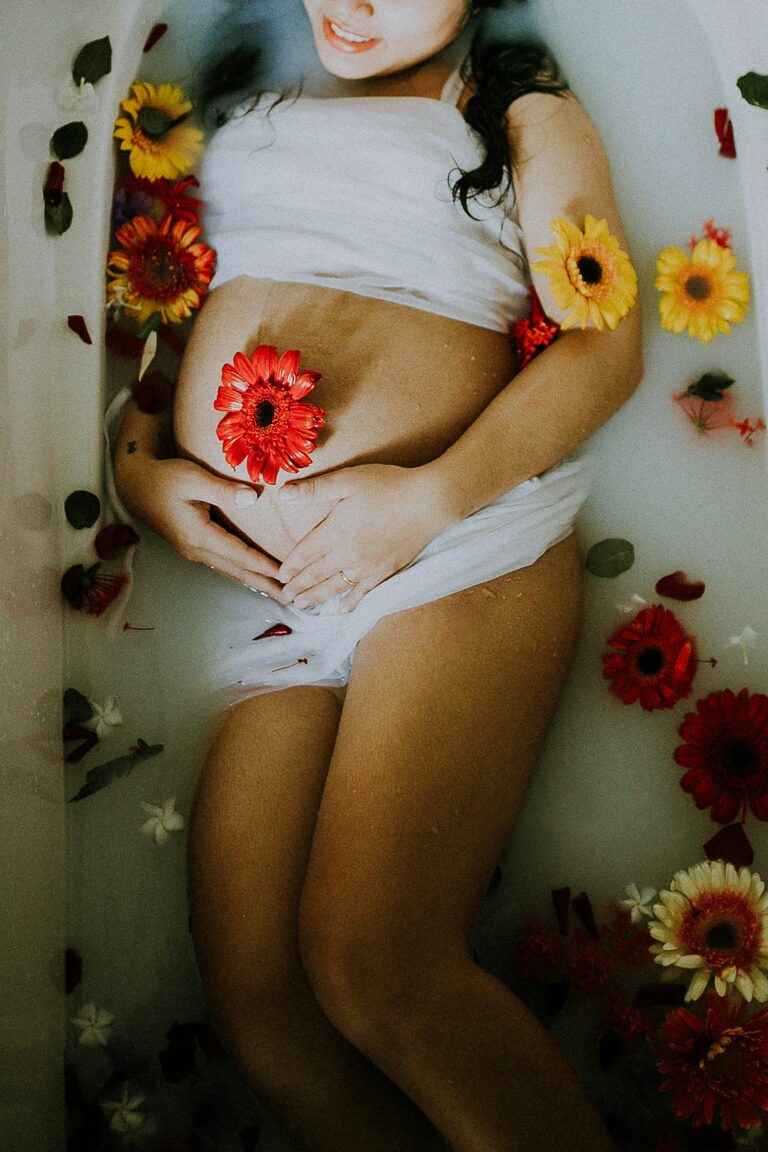
Transitioning from pregnancy to caring for a newborn—what an extraordinary yet demanding journey. Many parents, amidst all the excitement and responsibilities, find their bodies raising a quiet alarm: fatigue in the back, odd twinges in the pelvis, tension creeping up the neck and shoulders, not to mention worries about core weakness or healing after a C-section or episiotomy. If those sensations sound familiar, you are certainly not imagining things. Physical and emotional changes after childbirth can be unexpectedly complex, sometimes lasting weeks, sometimes months. Postnatal osteopathy enters this landscape with a gentle, yet targeted approach—helping restore comfort, boost well-being, and support daily bonding with your baby. Curious how it works, what exactly happens during a session, and how to blend it seamlessly into your recovery routine? Let’s delve into scientific explanations, practical advice, and real-world solutions for your postpartum concerns.
What Is Postnatal Osteopathy? Scientific Principles and Practical Benefits
Postnatal osteopathy stands as a holistic treatment approach focused on the days, weeks, and months following delivery. At its heart: hands-on care that honours the body’s remarkable, natural ability to heal. What sets postnatal osteopathy apart? Imagine a treatment not limited to muscles and joints, but addressing the entire interconnected system—bones, fascia, nerves, even the function of internal organs. Gentle manual therapy works to restore musculoskeletal balance, improving mobility and easing discomfort or pain. There’s a strong emphasis on physiological changes unique to each mother, with careful attention to the pelvic floor, abdominal region, and scar tissue.
The approach is not just about ‘cracking’ or ‘pushing’. Techniques include soft tissue mobilisation, joint mobilisation, cranial osteopathy—each one chosen based on your medical history, birth experience, and current symptoms. Postnatal osteopathy encourages restoration of posture, relieves tissue tensions, addresses circulatory issues, and fosters emotional equilibrium. Why does all this matter? Because women recovering from childbirth face enormous shifts—hormonal, muscular, structural—and today’s sedentary lifestyle, coupled with modern stressors, rarely helps our body adapt as smoothly as we’d hope.
Postnatal Changes: Why Does Your Body Need Extra Support?
Pregnancy transforms the body in ways difficult to anticipate: connective tissue stretches, ligaments loosen (thanks to hormones like relaxin), and the pelvis prepares for delivery by widening. Even after giving birth, these adaptations don’t instantaneously reverse. On the contrary, joint instability and vulnerability to strain can persist due to hormonal fluctuations and weakened muscle tone. The impact is felt most in the pelvic region, lower back, and—quite often—upper body, thanks to hours spent feeding, carrying, and soothing your newborn.
Two anatomic powerhouses take centre stage: the abdominal diaphragm and the pelvic floor. If their movement is limited or function compromised, breathing, core support, and continence may be affected. In practice? That can mean persistent back pain, a dragging sensation in the pelvis, or discomfort with even gentle activity. Postnatal osteopathy addresses these specific complaints, using gentle hands-on techniques to support the body’s gradual return to comfort, while considering scar tissue, cesarean recovery, or diastasis recti (abdominal muscle separation).
Common Concerns: How Postnatal Osteopathy Makes a Difference
Pain in the lower back or pelvis, often brushed off as ‘just part of new motherhood’, deserves attention. After all, weakened muscles and stretched ligaments can make simple movements feel awkward or uncomfortable. Postnatal osteopathy excels at identifying and releasing muscle tension—helping the body reclaim natural alignment and joint mobility.
Pelvic floor dysfunction appears in various forms—urinary leakage, heaviness, or even prolapse. Rather than offering one-size-fits-all advice, osteopaths use techniques to support pelvic realignment and help these deep core muscles recover. When diastasis recti is present, meaning the abdominal muscles have separated, the gentle approach of postnatal osteopathy serves to promote safe healing and core stability.
What about discomfort higher up? Feeding routines, especially breastfeeding, result in endless hours with a baby in arms. Postnatal osteopathy soothes neck and shoulder tension, and can even alleviate De Quervain’s tenosynovitis—a painful wrist condition frequently triggered by repetitive baby lifting.
Not to be overlooked: persistent headaches and fatigue, so common with sleep deprivation and emotional stress. Here too, focused osteopathic techniques relax fascial tissue, aid circulation, and may enhance overall mood.
And yes, support extends to your little one. Some babies experience latch difficulties, colic, or discomfort after a tough delivery; paediatric osteopaths offer gentle, non-invasive support for these concerns, ensuring baby’s comfort during feeding and rest.
Manual Techniques and Scientific Approach
You might wonder, what actually happens on the treatment table? The foundation: soft tissue massage, targeted stretching, hands-on techniques to mobilise joints, and cranial osteopathy. Postnatal osteopathy is never invasive, always working with your body’s natural healing rhythm. Each session is individually tailored, carefully tracking your stage of postpartum recovery.
Key outcomes sought:
- Restoration of comfortable joint and postural alignment
- Improved blood and lymphatic flow for tissue repair and reduced swelling
- Targeted pelvic floor and core muscle rehabilitation
- Modulation of the nervous and hormonal systems, which can ease anxiety, improve sleep, and stabilise emotional states
Patients often describe subtle yet profound shifts—lightness, greater range of motion, or a newfound sense of balance. While relief can be significant after just one session, a series of visits often supports a more lasting transformation.
Boosting Maternal Comfort and Bonding
Why pursue comfort after birth? The answer is simple: when the body is at ease, connecting with your baby feels more natural, feeding becomes less strained, and cuddling is pure pleasure rather than a physical challenge. Postnatal osteopathy allows for more ergonomic positions during breastfeeding or bottle-feeding, reducing stress on the spine and shoulders. Practitioners may demonstrate alternative holds, suggest using pillows or footrests, or propose practical daily adjustments.
For those encountering latch or feeding issues with their infant, paediatric osteopathy offers specific techniques to gently improve mobility in the jaw, neck, and upper spine—potentially smoothing out feeding difficulties for both mother and child.
There’s tremendous value in relieving maternal stress, too. When physical discomfort eases, emotional well-being often follows. The collective benefit? A smoother adjustment for the entire family, especially in those first challenging months.
When to Start, How to Choose, and What to Expect
Deciding when to begin postnatal osteopathy requires tuning in to personal recovery. For some, preventive sessions a few weeks post-birth make a world of difference; for others, addressing specific pain points is the priority. In any scenario, clearance from your usual doctor is important, particularly after cesarean or perineal injury. The key is attentive listening—both to what your body tells you and what your medical providers recommend.
Professional training and experience matter. Choose someone who understands women’s health, with clear qualifications in postnatal osteopathy. Compassion, attentiveness, and the ability to adapt treatment to your evolving needs are signs of a trustworthy provider. Increasingly, osteopaths collaborate with gynaecologists, physiotherapists, midwives, and mental health professionals for holistic postpartum recovery.
During a typical session, expect to discuss your body’s story in detail—pregnancy, delivery, current symptoms, stress factors. The hands-on assessment may include gentle mobility tests and tailored techniques, always respectful of sensitive or healing tissues. Sessions usually last 30 to 45 minutes, with occasional follow-ups for sustained results. The advice does not stop at the treatment room: practical tips on home exercises, ergonomics for holding and feeding, and strategies to avoid unnecessary strain are part of the package.
Integrating Postnatal Osteopathy with Everyday Life
Wondering how to maximise the benefits of postnatal osteopathy in daily life? First, gentle activity is your friend—especially pelvic floor and core exercises. Progressions should be gradual, avoiding high-impact movement until you’re truly ready.
Practical posture matters. Learn to switch arms when holding your baby, sit with your feet supported, and keep your back neutral while feeding or lifting. Supportive furniture, ergonomic carriers, and proper techniques all contribute to reducing accumulated strain.
Nutrition forms a key pillar of tissue healing and energy restoration. Collaboration with a dietitian may be worth considering, especially if you are struggling with fatigue or breastfeeding concerns. And never underestimate the power of mindful relaxation: simple breathing exercises, gentle stretches, or short moments of calm can dial down stress and boost your sense of well-being.
Postnatal osteopathy combines comfortably with physiotherapy (ideal for muscle rehabilitation), massage (for deep relaxation), and mental health or lactation support—aligning with a comprehensive, multi-professional model of postpartum care.
The Evidence: What Do Research and Mothers Say?
Early studies and clinical experience suggest that postnatal osteopathy can bring considerable relief—reducing pain, supporting recovery, and enhancing comfort for new mothers. While more large-scale research will deepen our medical understanding, the real-world consensus from many clients is encouraging: less pain, more mobility, and a greater capacity to engage joyfully with their babies.
The field keeps evolving. Integrated exercise plans, detailed assessments, and multidisciplinary collaboration are redefining best practices in postpartum care. Non-invasive, manual therapy approaches are increasingly sought after for their gentle yet effective results.
Key Takeaways
- Holistic care supports relief from pain, speeds healing, and improves post-delivery well-being
- Focusing on comfort helps foster relaxed feeding, stronger bonding, and a smoother parenting transition
- Postnatal osteopathy uses gentle manual techniques—safe for most, including breastfeeding mothers and those with healing scars
- Seek out practitioners with targeted training in postnatal osteopathy and value multi-specialist input for complex needs
- Growing clinical evidence and ongoing innovations point to substantial benefits, but always consult your medical team for personalised recommendations
And remember, resources and trustworthy professionals are available to guide your recovery. For personalised advice or free health questionnaires tailored to your child, explore the Heloa app.
Questions Parents Ask
How soon after childbirth can you start postnatal osteopathy?
Recovery pace differs for every individual. Some parents prefer to begin postnatal osteopathy just a few weeks after delivery, while others may choose to wait longer, guided by how their body feels or on the advice of their healthcare provider. Particular care is necessary in cases of cesarean or difficult delivery—medical clearance is always wise before starting any new therapy.
Is postnatal osteopathy safe while breastfeeding?
Yes—therapists utilise gentle touch and non-invasive methods, with full attention to the comfort and needs of breastfeeding mothers. Sessions often include practical guidance for comfortable feeding postures, helping reduce strain. Should you face any specific concerns, share them openly with your practitioner.
How to find a qualified postnatal osteopath?
Experience in women’s health and documented qualifications are important. Look for positive feedback from other parents, or recommendations from your healthcare community. Qualities such as attentive listening, respectful communication, and the ability to adapt treatment for individual recovery stages are valuable. If unsure, reach out to your midwife, doctor, or trusted parenting circles for suggestions.