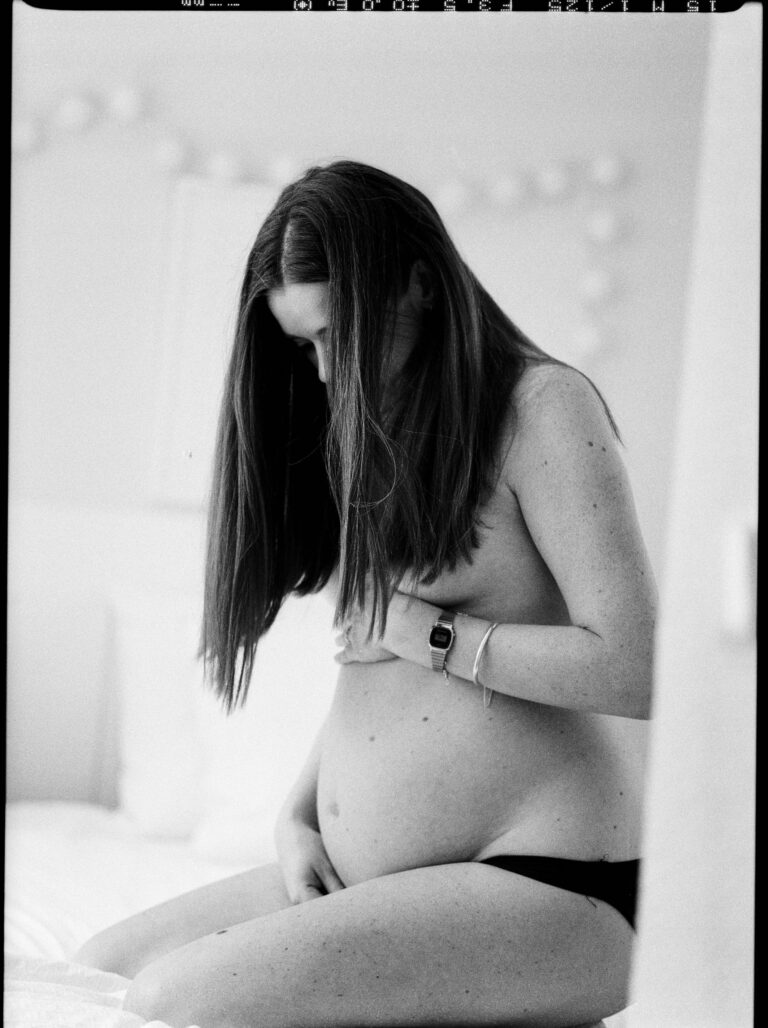
A whirlwind of joy, a wave of exhaustion, and then—quite unexpectedly for many—comes the onset of postpartum bleeding. Perhaps you braced yourself for sleepless nights, for baby’s first cries, for the all-encompassing embrace of parenthood, but the reality of continuous vaginal discharge after childbirth still catches most by surprise. Maybe you are wondering, will this heavy bleeding ever stop? How do you know what’s normal, and when should you be concerned? From the darker days right after delivery to those faint stains that linger for weeks, postpartum bleeding can raise countless questions, sometimes anxiety. Understanding the length, colour, and hidden meaning behind every change might seem overwhelming, but a few well-chosen explanations and simple tips will help you regain confidence. Direct answers, medical insights, and gentle encouragement—here’s what matters when caring for both your baby and your healing body.
Understanding Postpartum Bleeding: From the Delivery Room to Full Recovery
Postpartum bleeding, also known as lochia, is much more than an ordinary period. Imagine your uterus, having nurtured your child for nearly ten months, is now in the process of carefully shedding its extra lining. That discharge you’re seeing? It is a medley of blood, mucus, and small fragments of uterine tissue—all signs of healthy, progressive healing.
Straight after childbirth, whether by vaginal delivery or caesarean section, the uterus must shrink dramatically. It doesn’t just lose weight (dropping from around 1.5 kg to about 50 grams); it must also repair the spot where the placenta detached. As the wound contracts and heals, postpartum bleeding shifts in character.
You may notice:
- A significant but natural blood flow mimicking a strong menstrual period, especially during the first week.
- Later, a paler, almost watery or creamy discharge as healing continues.
- Episodes where discharge increases if you’ve moved suddenly, walked more, or breastfed (thanks to oxytocin-induced contractions).
It’s a process that lasts about four to six weeks, often zigzagging between lighter and heavier days.
The Science of Lochia: Phases and What They Mean
Lochia isn’t just red for a few days—its evolution can feel like deciphering secret signals from your own body. Here’s how it unfolds:
- Lochia rubra: First 3-4 days; expect a rich, red, heavy flow with possible small clots.
- Lochia serosa: Up to day 12; thinner, pink or brownish, composed largely of serous fluid and white blood cells.
- Lochia alba: Day 12 to six weeks; pale yellow or creamy, mostly mucus, with only traces of blood.
It’s not unusual if you think things have “stopped,” only for bleeding to resume later, especially after increased activity. Don’t be caught off-guard—stock up on sanitary pads (skip tampons and menstrual cups initially; they ramp up infection risk).
Triggers and Causes: Why Does Postpartum Bleeding Vary So Much?
Picture the uterine wall, freshly vacated by the placenta, dotted with tiny open vessels. The uterus clamps down, contracts, and works tirelessly to prevent prolonged blood loss. Still, if something interrupts this rhythm—uterine atony (a flabby, poorly contracting uterus), lacerations from rapid delivery, bits of retained placenta, or even rare blood clotting problems—the flow changes character.
Some risk factors make postpartum bleeding more erratic:
- Instrumental deliveries (forceps, vacuum extractions)
- Cesarean birth (tends to involve a greater initial blood loss)
- Multiple pregnancies, infections like endometritis, large babies, advanced maternal age, or anaemia
Underlying conditions—placenta previa, fibroids, clotting disorders—can stack the odds. Add obesity or a long, exhausting labour into the mix, and the story gets even more complicated.
Distinguishing Normal from Abnormal: When to Be Alert
What’s expected? Postpartum bleeding is heavy and red initially, then fades through the typical lochia stages. But certain warning signs deserve immediate attention:
- Soaking one pad in under an hour, or a sudden surge in flow after days of calm
- Clots bigger than a golf ball
- Bleeding that turns bright red and heavy when you thought recovery was on track
- Discharge that smells foul, paired with fever (over 38°C), persistent pain, or swelling
- Dizziness, rapid heartbeat, blurred vision, or weakness (possible indicators of blood volume loss)
If these symptoms emerge, don’t hesitate—your care team must know. Sometimes, an ultrasound is warranted to check for retained fragments, and laboratory tests may be needed to assess for anaemia or underlying clotting problems.
What Impacts Postpartum Bleeding?
Delivery methods shape outcomes profoundly. A cesarean section can mean larger immediate blood loss (about 1000 ml, compared to roughly 500 ml after vaginal delivery), and the ebb and flow of postpartum bleeding may feel different. Instrumental assistance increases the risk of trauma, while established infections, certain medications, and pre-existing health issues compound the picture.
A surprising twist: breastfeeding frequently intensifies uterine contractions, encouraging faster healing, sometimes making bleeding appear heavier during or after feeds, but often shortening the total recovery span.
Hygiene and Recovery: Practical Home Management Steps
Caring for the body—and soothing the mind—requires some gentle routines:
- Only sanitary pads or postpartum disposable underwear for several weeks; avoid inserting anything into the vagina to limit the risk of infection.
- Change pads often; wash hands before and after, simple but a powerful shield against infection.
- Daily showers with plain water (mild, unscented intimate cleansers if needed); patting rather than rubbing sensitive areas.
- Favour cotton pads—they are more breathable and less likely to irritate delicate skin.
- Employ ice packs for swelling, soft cushions, and, if required, prescribed pain relief.
- Loose clothing and slow return to physical activity—your body demands its own timeline.
- Nutrition isn’t a detail: prioritise an iron-rich diet (leafy greens, beans, eggs, fish, lean meats) and hydrate well. If significant blood was lost, iron supplements can help bridge the gap.
- Accept support—whether meals delivered by loved ones or simply a listening ear.
Emotional Well-Being: Recovery Is Not Just Physical
Modern medicine recognises what traditional cultures have long suspected: the postpartum phase is a major transition. There is value in rest, temporary solitude, and gradual resumption of social activities. Postpartum bleeding can feel isolating, but it also offers permission—almost a mandate—to slow down.
Be gentle with yourself if emotions rollercoaster: discussing feelings, leaning on support networks, or even reaching out to mental health professionals isn’t a weakness but a wise use of available resources.
Medical Monitoring for Postpartum Bleeding
Medical evaluations involve a mix of visual checks (sometimes by weighing used pads), monitoring vital signs, pelvic exams, and laboratory analyses for anaemia or coagulation disorders. If bleeding becomes persistent or severe:
- Treatments may include IV fluids, blood transfusions, medications to contract the uterus (like oxytocin or misoprostol), and, if necessary, procedures to remove retained tissues or repair trauma.
- Occasionally, advanced options like balloon tamponade or artery embolisation are needed.
- Proactive risk checks, routine administration of uterotonics after delivery, and vigilant follow-up improve outcomes.
In every case, clear communication with your medical team is fundamental; articulate your medical history and don’t overlook new or changing symptoms.
Awareness of Complications: Potential Challenges From Postpartum Bleeding
Rarely, postpartum bleeding opens the door to additional complications—endometritis (uterine infection); haematomas beneath perineal tissues; formation of dangerous blood clots (risking deep vein thrombosis or pulmonary embolism); or, in extreme cases, shock or organ injury.
Persistent fatigue points towards anaemia. Low energy can even impact breastfeeding or daily functioning. Occasionally, rare conditions like uterine inversion or Sheehan syndrome arise. A prior episode of postpartum haemorrhage boosts the likelihood of reoccurrence but, with planning and thorough follow-up, most families continue to experience healthy recoveries and pregnancies.
Tracking and Documenting Recovery
Monitoring patterns, changes, and symptoms helps both families and care teams. Record:
- Type and soak time of each pad (always pads, never tampons)
- Evolution of discharge: red, then pink to yellowish-white
- Size and frequency of clots
- New symptoms: fever, pain, dizziness, odour shifts
Keeping a diary—with pen and paper or phone apps—empowers you to spot changes and discuss accurately with your doctor. For some, taking photos for reference (if recommended) adds another layer of reassurance.
Recovery: Moving Beyond Postpartum Bleeding
Fatigue, low energy, and vulnerability often accompany postpartum bleeding, especially if blood loss was high. Beyond rest and adequate hydration, focus on balanced nutrition, iron supplementation if required, and physical healing of any stitches or scars.
Breastfeeding’s double-edged sword—encouraging healing but sometimes challenging if energy is low—is best managed with professional support and patience. Psychological and emotional recovery deserve equal respect: open communication, acceptance of help, and seeking expert guidance where necessary can transform the postpartum experience. Physical change and emotional evolution go hand-in-hand, and healing, in all its forms, demands both time and self-kindness.
Key Takeaways
- Postpartum bleeding is a normal, clear sign of recovery, progressing through predictable color and flow stages.
- Understanding what’s expected—and what isn’t—makes it easier to react calmly and promptly.
- Heavy, persistent bleeding; large clots; fever; pain; or foul-smelling discharge require immediate medical attention.
- Hygiene, rest, and an iron-rich diet speed healing and reduce infection risk.
- Tracking changes with a diary fosters autonomy and helps healthcare providers act swiftly if concerns arise.
- Professional healthcare teams are there to support every stage – never hesitate to reach out.
- For personalised guidance, practical health questionnaires, and emotional support, explore the application Heloa—a trusted companion for new parents.
Questions Parents Ask
How long does postpartum bleeding last after a cesarean section?
Generally, postpartum bleeding after a caesarean aligns with the same timeline—a steady pattern for about four to six weeks. Sometimes, the flow feels lighter in the first days than after a vaginal birth, but expect small fluctuations, especially when you are more active. If heavier bleeding, large clots, or unusual odour appear, contact your care provider. Everyone recovers at a unique pace.
Can breastfeeding affect postpartum bleeding?
Yes—breastfeeding prompts the release of oxytocin, which may intensify postpartum bleeding during and just after a feed. These extra-strong contractions tend to help the uterus heal faster overall, often shortening the bleeding’s total duration. Notice heavier flow each time you breastfeed? That’s normal, but pay close attention to any strange odours or rapid increases—keep monitoring changes closely.
What should I do if postpartum bleeding returns after it has stopped?
Sometimes, after a burst of activity, postpartum bleeding can temporarily resume. Slowing down, ensuring enough rest, and observing symptoms is usually enough. Yet, if bleeding turns bright red, becomes suddenly heavy, or comes with pain, fever, or unpleasant smell, talk to your care provider promptly. Trust the signals your body sends—seeking medical advice provides reassurance and timely solutions.
Further reading: