Bringing a baby into the world stirs a whirlwind of emotions—wonder, anticipation, even a hint of anxiety. For many parents, whispers of the word episiotomy prompt a flurry of questions. What is it, when is it necessary, and how could it shape the experience of childbirth and recovery? This topic, surrounded by both myths and well-grounded science, deserves clarity. From the moment your medical team mentions “surgical cut” to the days spent healing and adjusting, every detail counts. Parents often wonder about pain, healing, or whether those stitches will leave a lasting impression. Let us unpack the essentials together—decision-making, real-world scenarios, ways to safeguard your well-being, and the support available, every step of the way.
Understanding episiotomy: facts and evolution
What is an episiotomy?
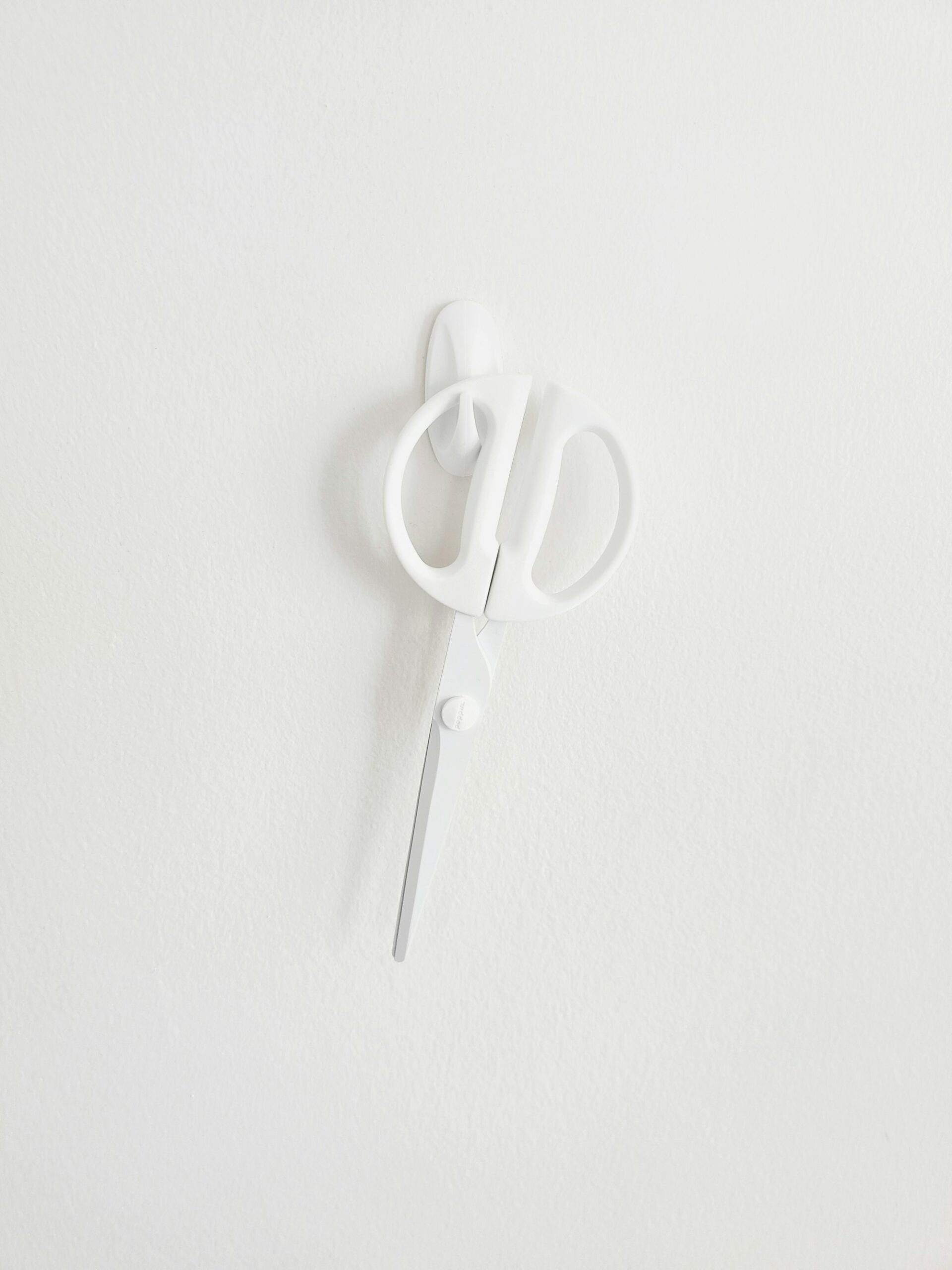
Picture this—a swift, controlled surgical incision in the perineum (that stretch of tissue between the vaginal opening and anus) made during the second stage of labor. The episiotomy isn’t carried out lightly. It is performed, usually under local or existing regional anesthesia, when your doctor or midwife is concerned that a wider opening is needed for birth, either for your safety or the baby’s. Think of it as a medical intervention designed to enlarge the passage, often using precise scissors or a scalpel, just as the baby’s head crowns. The perineal muscles must stretch significantly, and sometimes, such precision seems to offer more protection than chance.
Scientific perspectives have shifted over the decades. A surgical cut, once considered a kind of insurance against unpredictable, severe perineal tearing, is now approached with caution. Why? Because new research, especially from the 1980s onwards, has revealed that routine use of episiotomy may actually bring as many challenges as benefits.
Why and when is an episiotomy performed?
Indications: when does episiotomy make sense?
Not every childbirth requires a surgical cut. So, when does the medical team lean towards episiotomy? Here are the genuine, evidence-backed situations often confronted:
- Instrumental deliveries: Tools like forceps or vacuum are sometimes required, particularly if the baby is stuck or labor is prolonged. Creating extra space might reduce the risk of uncontrolled, deeper tears.
- Large baby: When the baby’s estimated weight creeps past 4000 grams, or the shoulders get stuck (called shoulder dystocia), a well-placed surgical incision can help reduce severe tearing involving the anal sphincter.
- Fetal distress: Quick delivery may suddenly become essential if the baby’s heart rate signals trouble.
Outside these contexts, regular, healthy vaginal births rarely call for episiotomy anymore. Indeed, guidelines shaped by organizations like ACOG, WHO, and NICE emphasize a restrictive, individualized approach.
Old routine vs. modern recommendations
Looking back, many mothers—especially first-timers—underwent episiotomy without strong medical need, simply because it was thought to prevent unpredictable tears or protect pelvic health. However, robust studies have revealed that naturally occurring tears might heal faster and with fewer complications compared to a surgical cut. Today, the pendulum has swung. Selective application is the norm, not the exception.
Natural tears versus episiotomy: what is safer?
The body is astonishing—perineal tissue can stretch up to 65% as the baby descends. Sometimes this results in minor, spontaneous tears (often small, easier to heal, and not extending into deeper muscles). On rarer occasions—less than 1%—more severe tears arise that may involve the anal sphincter. Interestingly, an episiotomy isn’t always an insurance policy against serious injury, but rather a tool tailored to specific high-risk births.
Different forms: midline and mediolateral episiotomy
- Midline (median): Neat, fast to repair, but can more easily extend into the anal area.
- Mediolateral: The incision angles away from the anus, used more often because it provides better protection for the anal sphincter, though is a bit more challenging to repair.
Other variants—lateral, J-shaped, or even rare modified approaches—find their use in special corners of clinical practice, often guided by unique anatomical or surgical needs.
The episiotomy procedure: what really happens?
When the baby’s head is about to emerge, and tension is at its peak, the decision is made. Local anesthetic (a quick numbing injection) or a boost from an epidural keeps you comfortable. The cut itself is brief—2.5 to 3 centimeters, strategic, precise.
Right after birth, the doctor or midwife closes the incision using absorbable stitches (no need to have them removed later). Layer by layer: vaginal mucosa, muscle, then skin. Healing, in most cases, unfolds over 4–6 weeks, although some discomfort may linger a bit longer. A general pattern emerges—most women feel significant improvement by week two, with the ache fading steadily.
Benefits and boundaries: when episiotomy helps, and when it doesn’t
No question, when complications rear up—rapid delivery needed, instrumental assistance required, risk of severe tear looming—a timely episiotomy protects both mother and baby. Think shorter high-stress moments and, sometimes, avoidance of the most daunting complications. Yet, the operation isn’t a magic shield. Research supports natural tears as less severe, faster to heal, and less likely to leave troublesome scarring.
The risks and potential side effects
Immediate recovery: what to expect
Pain. Swelling. Some bleeding—those early days post-delivery might not be a walk in the park. With proper hygiene and a gentle approach, complications like infections or hematoma (a small, painful blood pool under the skin) are infrequent, but possible.
Lasting effects: scarring and functionality
Every surgical cut leaves a trace. Minor scarring is almost guaranteed, but long-term problems—painful sexual intercourse (dyspareunia), pelvic floor discomfort, or changes in continence—are rare. High-quality repair and attentive postpartum care make a world of difference.
Weighing the two: episiotomy vs natural perineal tears
Science leans away from routine cuts. Natural tears often heal more quickly and involve fewer long-term issues. When episiotomy is the right call, mediolateral cuts stand out as the preferred, safer choice.
Can episiotomy and major tears be prevented?
Perineal massage: stretching nature’s potential
One small yet powerful tool—perineal massage—typically gets the green light from medical professionals around week 34–35 of pregnancy. Using natural oils, like almond or olive oil rich in vitamin E, gentle pressure applied to the perineum increases elasticity. Just a few minutes every day can yield notable benefits: softer, more resilient tissue and reduced unconscious tension that otherwise slows baby’s journey.
Additional protective strategies
- Warm compresses during labor: Helps keep tissue supple and reduces chances of tears.
- Choosing birth positions: Side-lying or upright postures ease pressure on the perineum.
- Controlled, slow pushing: Following your provider’s guidance during the final moments prevents abrupt stretching.
- Hands-on support: Experienced professionals guide your perineum, providing an extra layer of care just as delivery nears.
The indispensable role of healthcare teams
Experienced, supportive caregivers—doctors, midwives, nurses—hold a vital role in reducing unnecessary episiotomy. They monitor minute-by-minute, adapt strategies, and keep your preferences central, offering both expertise and reassurance.
Recovery after episiotomy: what is normal, and what needs attention?
The healing journey, day by day
Most recoveries wrap up in 4–6 weeks. Keeping the perineal area clean is non-negotiable—rinsing with warm water after urinating, patting dry (no rubbing), wearing loose, breathable fabrics. Consider cold compresses at first, then soothing sitz baths. Safe pain relief, such as acetaminophen or ibuprofen, often brings relief.
Feel up for gentle movement? Pelvic floor exercises (Kegels) help restore muscle tone and prevent future issues. But wait for a green light before any heavy lifting or strenuous activity.
When complications arise
Redness, pus, bad-smelling discharge, increasing pain, or fever—these may hint at infection. In such cases, an early visit to the doctor ensures no time is wasted. Prolonged discomfort, or any worries about healing, always merit a conversation.
Recovery beyond the body
The emotional landscape after birth can be bumpy—relief, expectation, frustration if healing is slow. Family, friends, or mental health support can make all the difference.
Global and regional rates: how common is episiotomy today?
A striking transformation: once routine, now rare in many places. For example, the episiotomy rate in the US has dropped from a towering 50% in the late seventies to about 12–31% today. In Europe, including France and the UK, the shift to a selective-use approach means less than 20% of vaginal births involve the procedure. However, in some regions—including parts of Latin America—rates remain high, shaped by deep-rooted medical traditions.
Factors influencing these numbers? Provider training, hospital protocols, scientific evidence, and broader accessibility of education all play their part.
Special scenarios in childbirth: high-risk situations and twins
In multiple births or challenging cases—twins, rapid labor, medical emergencies—providers may reach for their scissors. Each case is assessed on its own merits, guided by contemporary medical knowledge and the birth context. Instrumental deliveries often require extra space, so a mediolateral cut is typically chosen for optimal safety.
Episiotomy and future births: what about next time?
A properly healed site rarely causes trouble in future deliveries. Most women never need a second episiotomy—decisions depend entirely on the next labor’s unique path. Parents planning subsequent pregnancies should discuss birth history and strategies to keep the perineum safe, especially when aiming to avoid further intervention.
Navigating choices: ethics, communication, and autonomy
Once a universal practice, episiotomy has been redefined by modern research and open conversations. Informed consent now takes center stage—understanding the risks, the alternatives, and the preferences of each parent. Shared decision-making is the gold standard; it balances medical wisdom with personal comfort.
Key Takeaways
- Episiotomy is no longer common as a routine intervention, with clear guidelines supporting its selective use.
- Most vaginal births proceed safely without an episiotomy.
- Research links natural perineal tears to faster healing and fewer complications compared to surgical cuts, except in particular clinical scenarios.
- Regular perineal massage and careful, guided birthing techniques reduce the risk of requiring an episiotomy or sustaining major tears.
- Emotional and physical recovery deserves as much care and attention as the technical side of childbirth—help is always available.
- Open discussion with your healthcare team empowers you to make informed, personalized decisions during labor.
- For tailored guidance and no-cost health questionnaires for your child, discover the Heloa app.
Questions Parents Ask
What are the different types of episiotomy?
The most common types include mediolateral episiotomy (angled away from the anus) and midline episiotomy (a straight incision downwards). In rare circumstances, other forms such as lateral or modified incisions may be performed, all depending on the mother’s anatomy and real-time birth needs. Each choice is made to ensure the safest outcome for both mother and baby.
How do you care for an episiotomy after birth?
Post-episiotomy care is all about hygiene and comfort. Cleanse the area with warm water after visits to the washroom, avoid vigorous wiping, and wear loose, breathable clothing. Cold compresses offer relief from swelling, while sitz baths can speed up comfort. For pain, medications like acetaminophen or ibuprofen are widely recommended. If swelling, pain, or signs of infection (bad-smelling discharge or fever) surface, reaching out to your doctor promptly is best. With patience and gentle self-care, most recoveries are smooth.
What complications can occur after an episiotomy?
Minor concerns like swelling, bruising, or pain are common but usually short-lived. Rarely, complications such as infection, bleeding, hematoma (blood pooling under the skin), or prolonged pain surface. Any foul discharge, excessive redness, rising pain, or fever calls for prompt medical attention, helping nip issues in the bud.
How long does recovery from episiotomy usually take?
Most women experience considerable healing within 4–6 weeks, though minor aches may last a bit longer. Adhering to good hygiene, resting, and gentle movement support speedy recovery. Be attentive to symptoms and don’t hesitate to consult your care provider for reassurance or if new problems appear.
Can episiotomy impact future deliveries?
A well-healed episiotomy rarely poses issues in subsequent childbirths. Repeat surgical cuts are not automatically anticipated; the decision depends on the unique conditions of the next labor. Discussing your birth history with the doctor can help plan for an even safer delivery next time.
Is perineal massage really effective in preventing the need for episiotomy?
Clinical research confirms that regular, gentle perineal massage enhances tissue flexibility, which can lower the risk of a major tear or the need for an episiotomy. Start around 34–35 weeks of pregnancy, using a vitamin E-rich oil, for best results.
Does every mother need an episiotomy?
Absolutely not. Modern practice supports doing episiotomy only when medically justified—such as in cases of fetal distress, complicated births, or instrumental delivery. Many first-time and experienced mothers deliver with no need for surgical intervention.
What should you avoid after an episiotomy?
For optimal healing, avoid strenuous activities, lifting heavy objects, and resuming sexual intercourse until given the go-ahead by your doctor. Gentle movement, good hygiene, and rest are your strongest allies during recovery.
Further reading: