When the phrase “ectopic pregnancy” appears in medical consultations or on a test report, it tends to spark uncertainty, alarm, and dozens of questions all at once. It’s a scenario many parents haven’t anticipated — wondering, can a pregnancy truly develop outside the uterus? What does this mean for health, future fertility, or the immediate days ahead? The anxiety is real, and so is the medical urgency. This condition isn’t rare, yet it remains shadowed by confusion and misconceptions. Here, every parent finds answers: How to recognise the signals? What are the real risks? Which actions protect, console, and empower?
What Exactly Is an Ectopic Pregnancy?
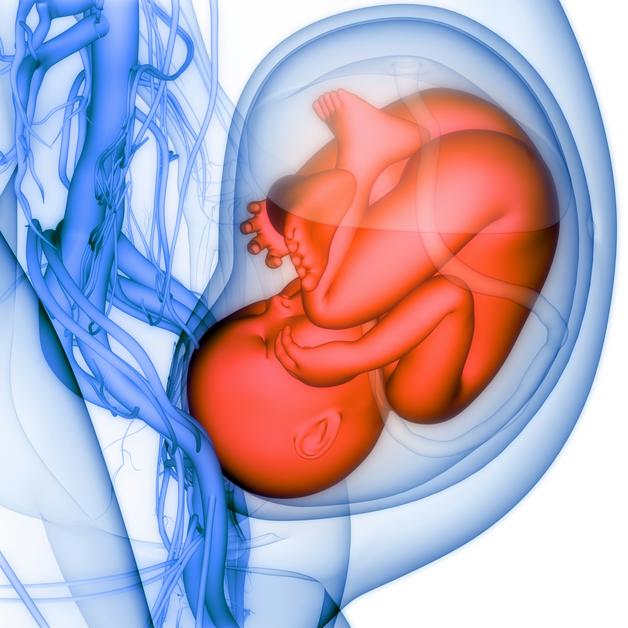
To start, imagine the journey of a fertilized egg—usually, it travels smoothly to the uterus, finds its place, and begins to develop. But sometimes, this process takes a detour. In ectopic pregnancy, the fertilized egg implants outside the uterine cavity—most often in the fallopian tube (tubal pregnancy), but sometimes in the cervix, ovary, abdominal cavity, or even a previous cesarean scar. Such “extrauterine pregnancy” can never develop into a healthy baby as the tissues involved simply aren’t built for this growing occupant.
What causes this? Abnormal implantation, damaged or inflamed fallopian tubes, or disturbance in embryo transport may all play a part. Sometimes, assisted reproductive technology (ART) like IVF slightly increases the odds. Yet for many, no clear risk factor is ever identified, turning ectopic pregnancy into a capricious adversary.
Where Does Ectopic Pregnancy Occur: Not Just the Tubes
It’s easy to fixate on “tubal pregnancy” — after all, about 90% of ectopic pregnancies settle in the fallopian tube (especially the ampullary region, with smaller numbers in isthmic and fimbrial segments). Yet, medical experience knows many variations:
- Cornual/interstitial pregnancy: Nestled at the junction of tube and uterus.
- Cervical, ovarian, or abdominal ectopic pregnancy: Rarer, each with unique hazards—cervical cases may cause serious vaginal bleeding, abdominal ones can remain hidden longer before symptoms show up.
- Heterotopic pregnancy: The striking coexistence of a healthy intrauterine pregnancy and a simultaneous ectopic pregnancy is possible—most commonly after fertility treatments.
Each location complicates both detection and care. Some, like abdominal ectopics, resist early detection and quietly bring trouble much later.
Understanding Causes and Risk Factors
Embryo implantation outside the uterus often traces back to one phenomenon: disruption in the passageway. Narrowed, scarred, or previously injured fallopian tubes—often following pelvic inflammatory disease (PID) or surgery—make travel perilous. Chlamydia and gonorrhea, the usual suspects behind PID, rank high on the guilt list, while prior tubal surgeries, use of certain intrauterine devices (IUDs), or tubal sterilization raise the statistical stakes.
Smoking adds its own risk—chemicals in cigarettes can interfere with the tube’s gentle sweeping movements, further heightening risk. The risk of ectopic pregnancy inches upwards with advancing age, notably after 35. But, if you’re holding no ticket to these risk factors, don’t relax completely—up to half occur in women without any preceding clue. Context matters: those using fertility treatments, like IVF, face a higher likelihood due to manipulated embryo placement.
How to Identify an Ectopic Pregnancy: Symptoms and Signs
Recognising an ectopic pregnancy can be a game-changer, preventing life-threatening complications. In the earliest days, it feels indistinguishable from a normal pregnancy—missed menstruation, subtle breast changes, perhaps vague pelvic uneasiness. But as the embryo grows—where it shouldn’t—distinctive warning signs surface:
- Pelvic pain more pronounced on one side
- Bleeding—usually not the classic heavy period, but often “abnormal vaginal bleeding”, dark or spotty
- Sudden, severe lower abdominal pain
- Dizziness, faintness, weakness—particularly worrying signs
Should the structure rupture, pain intensifies, might even radiate toward the shoulder (an odd but significant symptom, caused by internal bleeding irritating the diaphragm). Low blood pressure, rapid pulse, confusion, or fainting spell a medical emergency—hemodynamic instability and risk of hemorrhagic shock mean every minute is precious.
Imagine, if unexplained pelvic pain and abnormal bleeding take centre stage in the first trimester, ectopic pregnancy demands to be considered—especially with a previous ectopic or risk factor present.
Diagnosis: Getting to the Bottom of Ectopic Pregnancy
Science steps in fast when an ectopic pregnancy is suspected. A combination of pregnancy hormone monitoring—tracking serial beta-hCG levels in the blood—and high-resolution imaging ranks as standard protocol.
- If beta-hCG levels rise abnormally slow and transvaginal ultrasound (TVUS) fails to reveal a gestational sac within the uterus, doctors get suspicious.
- Sometimes, TVUS spots an adnexal mass (area beside the uterus) or identifies blood in the abdomen (hemoperitoneum), hinting at the site.
- Not every scenario is crystal clear—a diagnostic laparoscopy (a tiny incision in the abdomen to directly see the organs) confirms those difficult cases.
- Emergency situations may see the age-old culdocentesis—a needle test for internal bleeding—called into action.
Differential diagnosis gets broad—ovarian cysts, miscarriage, appendicitis—all possible mimics. Medical precision and clinical suspicion make all the difference.
Ectopic Pregnancy Treatment: What to Expect
Choice of treatment hinges on stage, size, location, and—importantly—the stability of the parent’s health. Here’s how the decision tree unfolds:
- Methotrexate treatment: This medication interrupts cell growth for early, unruptured cases where tubes have not yet burst. Repeat pregnancy hormone monitoring is non-negotiable—persistently high or rising hCG means closer watch or further treatment.
- Surgical intervention: Larger, advanced, or ruptured pregnancies demand intervention—often by laparoscopy (keyhole surgery).
- Salpingostomy: The ectopic pregnancy is removed, but an attempt is made to save the tube.
- Salpingectomy: Severely damaged tube gets removed to protect future health.
- In severe or unstable cases, open abdominal surgery (laparotomy) becomes the emergency plan.
- Non-tubal ectopics—cases in the cervix, ovary, or abdomen—sometimes require a combination: focused methotrexate, surgical removal, or other advanced techniques.
- Expectant management: If the body seems to resolve the ectopic pregnancy naturally, the option exists for close observation—careful monitoring is essential.
Recovery fluctuates—weeks to regain strength, sometimes longer for emotional wellness. Persistent or worsening symptoms always warrant swift medical reassessment.
Impact on Health, Complications, and Future Fertility
The major risk runs in a single word: rupture. Tubal rupture or bleeding in a less common site can trigger heavy internal bleeding, hemoperitoneum, even shock. Quick recognition and intervention save lives, preserve fertility, and avoid the devastating consequences of untreated cases.
What next? For many parents, a major concern is—could I become pregnant again? In the majority of cases, the answer is positive. Even after removal of one tube, the other often compensates. Odds improve with quick diagnosis and timely treatment, but repeated tubal damage or multiple ectopic pregnancies do affect future fertility chances—estimated recurrence risk stands at about 10%.
Prevention, though not infallible, revolves around sexual health—avoiding sexually transmitted infections, treating any pelvic infection promptly, and quitting smoking. Listening to your body matters if pelvic pain persists.
Emotional Journey: Coping With Ectopic Pregnancy
Beyond physical recovery lies an invisible terrain—called emotional healing. For many, the loss carries a weight that’s hard to express: grief, disbelief, frustration, or anxiety about the next attempt. Support is not a luxury, it’s a necessity. Consider:
- Psychological care with a mental health professional—sometimes a single session brings immense relief.
- Discussions with partners, family members, or trusted confidants—breaking the silence reduces the burden.
- Peer communities and support groups focused on pregnancy loss—exchange, comfort, and solidarity.
No experience, no pace for recovery, is wrong. Some parents feel renewed hope quickly, others need months. Every journey is equally valued.
Reducing the Risk: Prevention and Next Steps
While it’s not possible to erase every risk, addressing the known contributors goes a long way. Action points:
- Practising safe sex to prevent pelvic infections, seeking quick treatment for symptoms
- Quitting smoking (it improves both fallopian mobility and overall reproductive prospects)
- Recognising early signs and not delaying medical consultation—this singular decision can safeguard health
Discuss your fertility background openly with your healthcare provider—before conception, after a diagnosis, or between pregnancies—personalised advice and close follow-up become easier.
Life After an Ectopic Pregnancy: Recovery and Looking Ahead
The days, weeks, and months following an ectopic pregnancy—each person’s experience differs. Physically, most parents recover in a few weeks—with adequate rest, nutrition, and gentle activity as tolerated. Follow-up visits matter every bit as much—confirming the return of beta-hCG to zero and that no ectopic tissue is left behind. Emotional recovery, for many, takes longer.
Planning another pregnancy? Experts routinely suggest allowing at least three months for the body and mind to recover, reducing risks in future attempts. Discussing contraception during this waiting time with your doctor offers clarity and reassurance.
When you are ready: preconception care and an early ultrasound, checking the site of embryo implantation outside uterus in your next pregnancy, gives peace of mind and medical security. Parenting is a journey—each stage demands unique adaptation and courage.
Connecting with organisations devoted to pregnancy complications and recovery, or trying the Heloa app for more tailored advice and free health questionnaires, might offer guidance, reassurance, and knowledge at your fingertips.
Key Takeaways
- Ectopic pregnancy is a significant health emergency—prompt attention to abdominal pain, pelvic discomfort, or abnormal bleeding in early pregnancy keeps parents safe.
- Most cases involve the fallopian tube, but diagnosis and management shift if the site is cervical, ovarian, abdominal, or caesarean scar.
- Risk factors are wide: previous ectopic, pelvic infections, tubal or pelvic surgery, ART, age beyond 35, and tobacco use, among others—but many cases arise out of the blue.
- Treatment choices range from medical management (like methotrexate), through minimally invasive surgery, to close watchful waiting—personalised for each parent’s circumstances.
- Future fertility is preserved in most cases—with the right precautions, planning, and monitoring. Hope for a healthy pregnancy remains for the majority.
- Physical and emotional recovery happen at their own rhythm—resources, mental health professionals, and peer support play a pivotal role.
- For more personalised medical tips and free child health questionnaires, download Heloa application—a helpful ally in every parenting journey.
Questions Parents Ask
Can I have a regular pregnancy after experiencing an ectopic pregnancy?
Yes, in many situations, women have normal and healthy pregnancies after recovering from an ectopic pregnancy. If one fallopian tube has been removed, the remaining tube usually works efficiently. If doubts or emotional stress trouble you as you plan your next pregnancy, a detailed conversation with your healthcare provider can provide both reassurance and science-based advice.
What are the chances that ectopic pregnancy might happen again?
The risk of another ectopic pregnancy tends to be around 10%, sometimes a bit higher with certain factors like tubal damage or infection history. For some, extra monitoring or early scans offer safety. Individual circumstances vary—a cooperative relationship with your doctor ensures you’re best placed for a positive experience next time.
After an ectopic pregnancy, how long should I wait before trying again?
Giving your body and mind about three months’ time after an ectopic pregnancy is generally recommended. This interval helps healing and restores balance, reducing future risks. Discuss with your care provider—they’ll help choose the best timing and guide you toward your family goals with empathy and skill.
Further reading: