Parenting rarely follows a predictable script, and the shock of hearing the words “ectopic pregnancy” can stop even the most composed in their tracks. Questions erupt: Why did this happen? Could it have been prevented? Is future fertility at risk? When hope collides with complexity, clarity is desperately needed. An ectopic pregnancy signifies that the fertilized egg has implanted outside the womb—most often in the fallopian tube, but occasionally in the cervix, ovary, abdomen, or within the scar left from a cesarean section. Fast, accurate detection and informed support do more than save lives—they lay the groundwork for recovery and resilience. Parents deserve answers, attentive care, and strategies to protect their health and their future families. In this journey, every detail counts, from subtle warning signs to emotional healing and preparing for tomorrow.
Let’s unravel the key facts, risks, and possible paths forward.
What Is Ectopic Pregnancy? Risk Factors and Prevalence
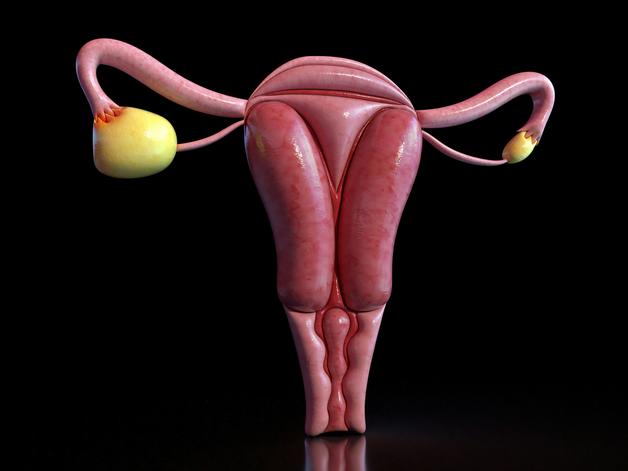
The term ectopic pregnancy describes any situation where a fertilized egg lodges outside the uterine cavity—a location unable to support a growing embryo. Nature intends that after fertilization, the egg travels smoothly through the fallopian tube to reach the uterus. What disrupts this route?
Damage is often the culprit. Scarring from pelvic inflammatory disease (PID), infections (especially chlamydia or gonorrhea), or past surgeries leaves the delicate lining of the fallopian tube misshapen or less mobile—nudging the embryo off course. Sometimes, infertility treatments like in vitro fertilization (IVF) inadvertently increase the risk of an ectopic location. Age—especially over 35—tilts the odds, as does smoking, a factor that subtly reshapes tubal health through its effect on cellular function.
Statistics are sobering, if not exactly reassuring: about 1–2% of pregnancies involve implantation outside the uterus. Yet, for women turning to assisted reproductive technologies, this risk climbs sharply. Importantly, half of all ectopic pregnancies emerge in those with no obvious risk factors, underscoring the value of vigilance.
Where Do Ectopic Pregnancies Occur? Types and Locations
While the fallopian tube remains the main setting for an ectopic pregnancy (especially the ampullar region), anomalies abound. Implantation can take place in the ovary, abdominal cavity, cervix, or a cesarean scar—each harboring unique dangers and requiring specialized attention. Sometimes, a heterotopic pregnancy emerges, where both a normal intrauterine and an ectopic gestation coexist, a scenario seen more frequently following fertility treatments.
Symptoms, complications, and treatment all hinge on the exact location. Cervical or abdominal pregnancies may silently progress longer, their warning signs muffled until later.
What Causes Ectopic Pregnancy? The Medical Underpinnings
At its heart, an ectopic pregnancy is the endgame of impaired embryo transport—but why does this happen?
- Infections: Notably, chlamydia trachomatis or neisseria gonorrhoeae can set off a cascade of tubal scarring and dysfunction.
- Prior surgery: Whether from previous ectopic pregnancy, tubal reconstruction, or sterilization reversal, any surgery near the reproductive tract leaves its mark.
- Infertility interventions: Procedures such as IVF or ovulation induction can inadvertently seed an egg where it cannot thrive.
- Advancing age: Declining tubal motility after age 35 subtly erodes the smooth passage of the fertilized egg.
- Lifestyle: Smoking emerges as a silent saboteur, impairing ciliary action (microscopic hair-like structures that guide eggs to their destination).
Surprisingly, in about half of all cases, no clear cause is found. The silent nature of tubal damage is often to blame—a reminder that even the keenest eye cannot predict every outcome.
Warning Signs and Symptoms: What Should Parents Look Out For?
Questions swirl: Is spotting normal? When does discomfort cross the line from benign to worrying? Early on, the signs overlap with standard pregnancy—missed period, mild breast tenderness, subtle fatigue. But as the ectopic pregnancy progresses, red flags may unfurl, sometimes suddenly and dramatically:
- Sharp or localized pelvic pain (often on one side, increasing in intensity)
- Abnormal vaginal bleeding—may be lighter or darker than a typical period
- Sudden, severe lower abdominal pain—sometimes radiating to the shoulder (a tell-tale sign of internal bleeding irritating the diaphragm)
- Dizziness, faintness, or sudden collapse—signals to seek help immediately
If the fallopian tube ruptures, pain can surge, bleeding may turn heavy, and the rapid drop in blood pressure leads to pallor, confusion, or loss of consciousness. This scenario is an emergency; every minute matters.
Diagnosing Ectopic Pregnancy: Testing and Imaging
Diagnosis blends clinical acumen with technological precision. Healthcare teams begin with a positive pregnancy test (urine or blood) and a careful review of symptoms and risk factors. But the real workhorse is the quantitative beta-hCG blood test, which measures the level of human chorionic gonadotropin—a hormone that, in a healthy pregnancy, roughly doubles every two to three days. Slower-than-expected increases, or plateauing levels, prompt further investigation.
A transvaginal ultrasound (TVUS) is indispensable: when levels of beta-hCG exceed a certain threshold and no gestational sac is seen in the uterus, suspicion for an ectopic pregnancy skyrockets. Sometimes, ultrasound uncovers an adnexal mass (a bulge near the fallopian tube or ovary) or signs of internal bleeding. Rarely, if diagnosis remains uncertain and the patient is stable, diagnostic laparoscopy (a minimally invasive surgery to directly visualize the reproductive organs) bridges the gap.
Other conditions—early miscarriage, ovarian cyst, even appendicitis—can mimic the symptoms. Detailed assessment helps distinguish among these possibilities, guiding treatment from here.
Treatment Options: Restoring Health and Protecting Fertility
Therapy for ectopic pregnancy hinges on early detection and the body’s response:
- Medication: In many cases where the pregnancy is small and unruptured, methotrexate—a medication that halts the division of pregnancy cells—may resolve the issue, preserving future fertility. Regular blood tests track the fall of beta-hCG levels to ensure full resolution.
- Surgery: If the pregnancy is larger, at risk of rupture, or not amenable to medication, laparoscopic surgery steps in. Surgeons may perform a salpingostomy (removing the ectopic tissue and leaving the tube intact) or a salpingectomy (taking out the entire tube, often when extensive damage exists). Occasionally, ovarian, cervical, abdominal, or scar pregnancies need specialized techniques or a combination of surgery and methotrexate.
- Expectant management: In select, highly monitored situations, the ectopic pregnancy may resolve without intervention.
The journey doesn’t end with physical recovery. Serial beta-hCG tests confirm clearance of all pregnancy tissue—the numbers must fall to zero to safely rule out lingering cells. Physical healing usually spans several weeks, while emotional turmoil may linger much longer.
Life After Ectopic Pregnancy: Health, Fertility, and Emotional Recovery
For many, the words “ectopic pregnancy” conjure images of dashed hopes and future uncertainty. Yet, the path forward is not set in stone. Women often conceive again—statistically, about 90% will have future pregnancies, though there’s a 10% chance of recurrence (higher if tubal disease persists). Even with one tube removed, the remaining tube may compensate, but if underlying risk factors endure, close monitoring becomes the new normal.
Medical research and clinical practice highlight preventive steps:
- Prompt STI treatment: Prevent infections from silently damaging tubal health.
- Stop smoking: Reversible, yes, but often overlooked. Quitting boosts chances for future intrauterine pregnancies.
- Recognize symptoms early: Heightens the odds of less invasive care, preserves fertility, and dramatically improves outcomes.
Emotionally, this experience can shake the strongest parent. Grief, confusion, even guilt can shadow recovery. What helps? Access to counseling, participation in support groups, or simply being heard by a caring professional or empathetic friend. Each parent’s journey is unique. Giving space for emotions—and seeking help if burdens grow—is nothing less than an act of strength.
Prevention and Planning for the Future
Thoughtful planning smooths the road to recovery. Healthcare teams often suggest waiting at least three months before trying again—time for both body and mind to heal, for scars (visible and invisible) to settle. Meanwhile, discussing contraception avoids surprises and ensures that when parents are ready, the odds are stacked in their favor.
For future pregnancies, preconception counseling with a healthcare provider and an early ultrasound to confirm location can reduce anxiety and detect problems at the earliest stage. Community organizations, online forums, and medical professionals each offer vital guidance and reassurance during this period of transition and anticipation.
Key Takeaways
- Ectopic pregnancy means the fertilized egg has implanted outside the uterus—most often in the fallopian tube, but not always, and it can become a threat to health if untreated.
- Half the time, there are no obvious warning signs or risk factors—making knowledge and vigilance paramount.
- Prompt diagnosis uses a combination of urine and blood pregnancy tests, quantitative beta-hCG assessment, and transvaginal ultrasound.
- Symptoms like one-sided pelvic pain, abnormal vaginal bleeding, or shoulder pain demand urgent consultation.
- Treatments range from methotrexate medication (for early/unruptured cases) to sophisticated surgical options, each tailored to the individual and the specifics of their condition.
- Fertility is preserved for most, and the dream of parenthood remains within reach, but monitoring is key for future pregnancies.
- Emotional wellbeing matters—counseling, support groups, and compassionate care form the backbone of holistic recovery.
- Always reach out for help, trust your intuition about symptoms, and know that specialized health resources are available every step of the way.
Need customized advice, timely alerts, or structured support? Discover the Heloa application for tailored health tips and free pediatric health questionnaires—your ally in navigating family health with confidence.
Questions Parents Ask
Can you have a normal pregnancy after an ectopic pregnancy?
Absolutely, many parents go on to have successful, healthy pregnancies after experiencing an ectopic pregnancy. The majority of women keep their fertility, même with only one fallopian tube. It’s normal to feel mixed emotions about future attempts—rassurez-vous, with the right support and follow-up, a positive outcome is often possible. If concerns about fertility persist, speaking openly with a healthcare provider can provide encouragement and practical guidance for the next steps.
What are the chances of an ectopic pregnancy happening again?
After an ectopic pregnancy, the risk of recurrence exists but remains relatively low for most people—around 10%. If there were risk factors like previous tubal surgery or ongoing infections, a closer follow-up may be recommended, simply to ensure the best care going forward. Chaque parcours est unique; rester à l’écoute de son corps et aborder les prochaines grossesses avec un accompagnement attentif offre les meilleures chances d’une expérience rassurante.
How long should you wait before trying to get pregnant again?
Il convient de laisser à la fois le corps et l’esprit le temps de récupérer après une grossesse extra-utérine. Souvent, un délai de trois mois est conseillé avant de retenter une nouvelle grossesse. Cela permet non seulement à l’organisme de guérir, mais aussi de retrouver un équilibre émotionnel. N’hésitez pas à discuter avec votre professionnel de santé pour déterminer ensemble le moment le plus adapté à votre situation et vos envies.
Further reading:









