Wildly unexpected, sometimes subtle, frequently confusing—Braxton Hicks contractions have a way of weaving themselves into the everyday narrative of pregnancy with astonishing unpredictability. One moment, everything feels serene; the next, a gentle, tightening sensation across the belly triggers a cascade of questions. Is this the prelude to real labour? Are these signs to worry? For so many parents-to-be, such sensations evoke more curiosity than clarity. The world of pregnancy is already brimming with transformations—physical, emotional, and psychological. Adding mysterious “practice contractions” to that mix? That’s enough to make anyone pause and wonder.
Navigating the landscape of Braxton Hicks contractions, parents often seek a compass: What exactly are these contractions? Why do they occur? When should you rest versus when should you reach for medical advice? This journey will shine a light on definitions, timings, biological realities, strategies for managing discomfort, and—most importantly—how to trust your instincts while respecting medical science. With a blend of scientific insight, practical advice, and a rhythm that moves from quick tips to deeper explanations, let’s untangle the realities behind these famed contractions.
What are Braxton Hicks contractions? Nature, timing, and origins
Imagine the uterus as an athlete, training quietly in the background—invisible but persistent. Braxton Hicks contractions are these training sessions: brief, irregular, surprisingly gentle tightenings of the uterine muscle, starting around the second trimester, sometimes as early as week 16-20. First documented by Dr. John Braxton Hicks in the late 19th century, these episodes serve as a preview, not the main event.
Scientifically, these contractions reflect a natural rehearsal. Without warning, the abdomen becomes firm—almost as if the belly is quietly “practising” for the marathon of true labour. They mostly come unnoticed in first pregnancies, but can be front-and-centre in subsequent ones, sometimes louder, almost unmistakable. Are they painful? Rarely. Are they regular? Almost never. And crucially: Braxton Hicks contractions never initiate the changes in the cervix that real labour demands.
When do Braxton Hicks contractions appear? Timing, frequency, and what influences them
The calendar of pregnancy is unpredictable. While Braxton Hicks contractions can technically emerge from the mid-second trimester, most people will recognise them only in the final weeks. And yet, some feel nothing until days before delivery—or not at all. The variation can be dizzying. Those with previous pregnancies often report earlier or more noticeable sensations, while first-timers may brush them off as simple stretching or gas.
Their hallmark is not just when, but how: always erratic, popping up predominantly towards the end of the day, after a brisk walk, or a period of busyness. A typical episode will last anywhere from a fleeting few seconds to a minute or two; never threatening a regular timetable and never inching closer together. Ten to fifteen a day is quite typical, sometimes less, usually harmless.
Does this irregularity ever become something to worry about? Only if the rhythm persists, the pain intensifies, or other warning signs accompany the tightening. Otherwise, these contractions come and go like waves—sometimes noticed, sometimes forgotten, always part of the background choreography of late pregnancy.
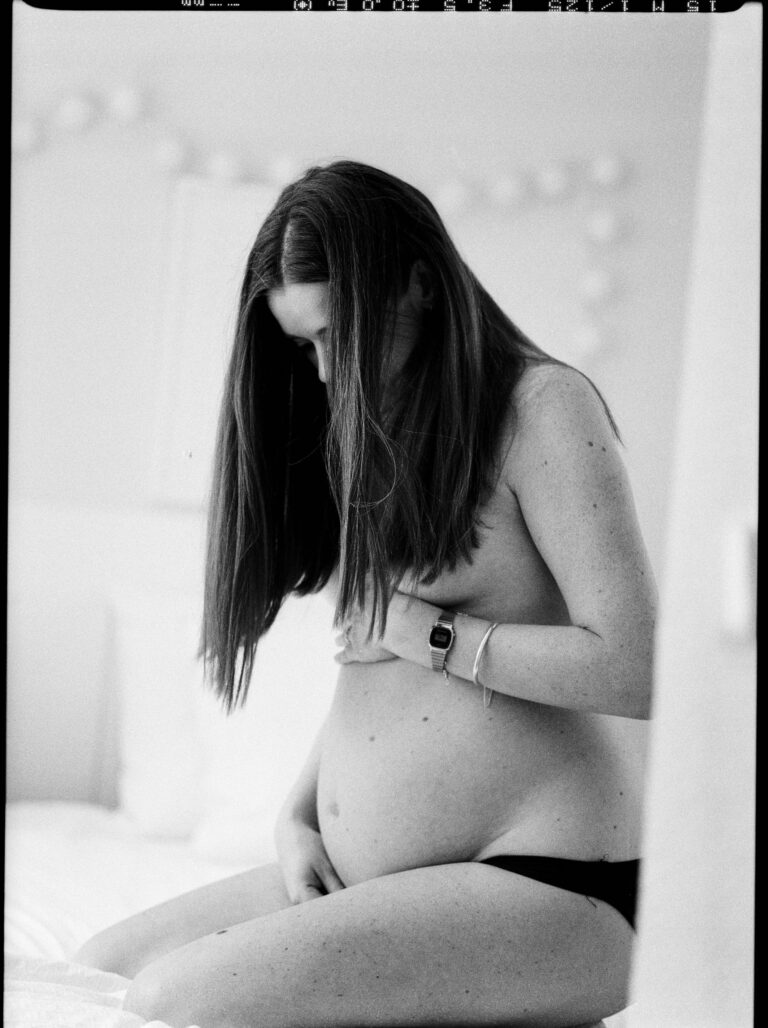
What do Braxton Hicks contractions feel like? Sensations and individual experiences
Picture this: a swell of tightness, almost as if someone gently squeezed around your belly, creating a sensation of firmness—a “balling up” rather than sharp pain. That’s the classic description. Sometimes it draws the attention; sometimes it whispers by, barely noticed. Discomfort ranges from non-existent to mildly awkward—a vague cramping, a stretch across the lower abdomen, or even a sensation radiating to the back.
Unlike menstrual cramps, the sensation is rarely persistent or deeply uncomfortable. Where menstrual cramps tend to arrive with a dull ache, Braxton Hicks contractions favour brevity and respond quickly to rest or a sip of water. The location? Primarily across the front, occasionally lower down or wrapping to the back, but never following a clear, marching pattern like true labour does.
Some may question—is it abnormal to feel nothing? Absolutely not. The spectrum is broad: total silence, frequent awareness, or anything in-between. Each pregnancy writes its own script.
Causes, triggers, and physiological role
What sets off these mysterious tightenings? Science points to several culprits:
- Dehydration: Even mild fluid loss heightens uterine irritability, increasing the tendency for these “practice” waves.
- Overexertion: A busy, tiring day can amplify sensations.
- Full bladder: Sometimes, just needing a toilet break is enough to stimulate the uterus.
- Sexual activity and orgasm: Not dangerous, just a predictable hormonal response, primarily due to oxytocin release.
- Active fetal movements: A robust kick from the baby can occasionally prompt a sudden tightening.
- Emotional or physical stress: Sensitivity is heightened during pregnancy; stress compounds it.
- Evenings: Fatigue accumulates, and episodes often rise towards night.
Biologically, what’s the purpose? Think of these episodes as a warm-up—a chance for the uterus to flex, stretch, and prepare for the intensity of active labour contractions later on. Increased uterine tone may help improve blood flow to the placenta, keeping the pregnancy in optimal shape.
Spotting the difference: Braxton Hicks versus true labour contractions
The confusion between Braxton Hicks contractions and true labour is legendary—so how to tell one from the other? The differences, though sometimes subtle, are critically important:
- Pattern: Irregular, unpredictable, never getting closer together (Braxton Hicks) versus a steady rhythm, intensifying and drawing closer (true labour).
- Sensation: Usually mild-to-moderate, not painful, fading with rest or hydration (Braxton Hicks); in contrast, real labour escalates, bringing persistent, strong discomfort that cannot be eased by changing positions.
- Effect on cervix: No dilation or changes with “practice” contractions, while true labour actively prepares the birth canal.
- Response to activity: Get up, move, drink water—Braxton Hicks usually subside. But labour contractions remain relentless, unmoved by such interventions.
It’s natural to be wary, especially as the due date approaches. But maintaining a record of frequency, intensity, and whether discomfort fades with rest can clarify the situation in most cases.
Soothing strategies: practical relief and daily comfort
What if the tightening becomes uncomfortable, or simply too distracting? A few notice-worthy routines can help:
- Hydration: Sipping water throughout the day, especially after a contraction, works wonders.
- Rest: Lying on the left side can optimise blood flow and relax the uterus.
- Change of position: Move, walk, stretch—sometimes a simple shift calms everything down.
- Warmth: A gentle (never hot) bath or a warm pack on the abdomen may offer significant comfort, unless a doctor advises against it.
- Prenatal stretching and yoga: These gentle exercises support flexibility and reduce strain.
- Breathing techniques: Slow, deep breathing actively reduces tension—beneficial for both body and mind.
Above all, the principle remains: listen to your body. If activity triggers tighter spells, take it slower. If exhaustion mounts, prioritise rest. Balance is the foundation.
Warning signs: when to reach out for help
A pause. Sometimes, even the most reassuring explanation isn’t enough—certain symptoms call for rapid action:
- Frequent, regular, intensifying contractions before 37 weeks (say, five or more per hour).
- Persistent or severe lower abdominal or back pain.
- Vaginal bleeding, watery discharge, or sudden loss of fluids—possible signs of preterm rupture.
- Noticing much less fetal movement.
- Fever, malaise, or an all-over feeling of being unwell.
Especially with higher-risk pregnancies—twins, previous preterm birth, underlying health issues—it pays to be extra attentive. Take notes on timing, intensity, and associated symptoms; your healthcare provider relies on this narrative to guide safe, evidence-based care.
Emotional wellbeing, misconceptions, and the role of family
The emotional undercurrent of Braxton Hicks contractions should not be ignored. First-timers, in particular, may cycle from anxiety to frustration, sometimes feeling caught between uncertainty and hope. Popular myths keep circulating—that these contractions mean imminent labour, or are dangerous, or that everyone feels them acutely. Reality, however, is softer. Most of these tightenings are harmless—nature’s way of rehearsing, not signalling an emergency.
Family and partners play a pivotal role. Sometimes, just a cool hand, a gentle massage, or a reassuring chat makes all the difference. Shared observation (tracking sensations together), open mutual support, and practical offers to help manage daily comfort lift some of the load from the pregnant parent’s shoulders.
Effects on pregnancy and fetal health
Here, the science lends reassurance: for the overwhelming majority, Braxton Hicks contractions pose no threat to either the pregnancy or the baby. There is no risk of hypoxia, no fear of precipitating preterm labour—unless those aforementioned warning signs begin to appear. In fact, these episodes foster uterine elasticity, optimise placental blood flow, and, over time, may even contribute to the body’s smooth transition to postpartum recovery.
However, emotional strain or unaddressed questions can add a layer of discomfort. Open communication with healthcare professionals is paramount. Each question deserves an answer, and reassurance is always justified.
Different types of contractions: a simplified overview
To truly make sense of all the vocabulary around pregnancy and labour, here’s a simple rundown:
- Braxton Hicks contractions: Irregular, mild, not progressive, with no cervical dilation.
- Prodromal contractions: More frequent but non-productive; a “dress rehearsal” just before labour.
- Active labour contractions: Regular, powerful, changing the cervix and propelling labour forward.
- Transition contractions: Short, highly intense, immediately preceding birth.
- Postpartum (“afterpains”): Help the uterus shrink post-delivery.
Whenever confusion arises, focus on the pattern, intensity, and response to rest. This approach sharpens communication with healthcare providers and builds autonomy.
Lifestyle strategies and prevention
How can daily habits support comfort and reduce unnecessary contractions?
- Drink water often—especially if weather is hot or you are physically active.
- Alternate activity and rest; don’t wait for fatigue to prompt a break.
- Opt for gentle exercise (walking, prenatal yoga) but pause if discomfort increases.
- Adjust routines—resting with legs elevated, shifting positions periodically, noting how activities correlate to tightening spells.
- Track and avoid triggers—monitor responses to activity, lack of fluids, or emotional stress.
- Engage in self-care—unhurried meals, relaxation, and time spent in calm environments are not luxuries, they’re foundations.
The daily dance between rest and gentle movement, balanced hydration and nutrition, empowers parents not just to be passive observers but active participants in their own wellbeing.
Key Takeaways
- Braxton Hicks contractions are typically harmless rehearsals, preparing the uterus for true labour without causing dilation or immediate risk.
- Timing, frequency, and sensations are highly individual—mild, irregular tightenings that ease with rest or hydration.
- Relief often comes from simple lifestyle strategies featuring hydration, rest, gentle exercise, and attentive self-care.
- Be vigilant for persistent, regular pain, bleeding, fluid loss, or fewer baby movements—such symptoms call for immediate medical advice.
- Partners, family, and professionals offer a network of support. Open conversations ease anxiety and bring clarity.
- Parents can download the application Heloa for tailored advice and free child health questionnaires at any time—empowering information, always at hand.
Equipped with knowledge, reassurance, and a clear understanding of their own body’s rhythms, parents can approach each episode of Braxton Hicks contractions with increased confidence and calm, secure in the knowledge that support and guidance are always available.
Questions Parents Ask
Can Braxton Hicks contractions feel different with each pregnancy?
Yes, absolutely. Many parents observe a wide variety in their experience—some hardly notice these waves during their first pregnancy, while others find them more intense or frequent with subsequent pregnancies. This difference has a lot to do with increased awareness, variation in the uterine muscle’s tone, and the fact that every pregnancy writes its own unique story. Only your experience is the benchmark—there’s no single way these contractions should feel.
Should I be worried if I don’t feel any Braxton Hicks contractions?
Not at all. It is completely usual to pass through pregnancy without any conscious recognition of these uterine tightenings. Every body’s sensitivity is different. The absence of obvious Braxton Hicks contractions does not indicate any issue for the pregnancy or for the baby’s progress. If you are healthy and your healthcare provider is pleased with the routine progress, then all is as expected.
Do Braxton Hicks contractions affect the baby?
Relief is near-total here—Braxton Hicks contractions are viewed as a normal and safe part of pregnancy, not impacting the baby or leading to labour. Babies continue to thrive in the womb, unaffected by these gentle, irregular tightenings. However, if you start spotting symptoms like regular, painful contractions or changes in baby’s movement, reaching out to your doctor always remains a wise step.