Questions rush in fast—what does placenta previa mean for my baby? Will labor be dangerous? Should daily life change overnight? For many parents, stumbling across the term placenta previa—sometimes whispered by a sonographer during an ultrasound or unexpectedly noted in medical records—ignites a cascade of uncertainties. At the heart of these worries stands a very real need for clarity. Placenta previa can upend the calm of pregnancy with unexpected bleeding, hurried medical appointments, and new concerns about delivery, but knowledge and a supportive plan redefine the experience. Here’s how an understanding of placenta previa helps demystify the journey, what signals deserve your attention, and why expert care transforms risk into reassurance.
What is placenta previa? Understanding the diagnosis
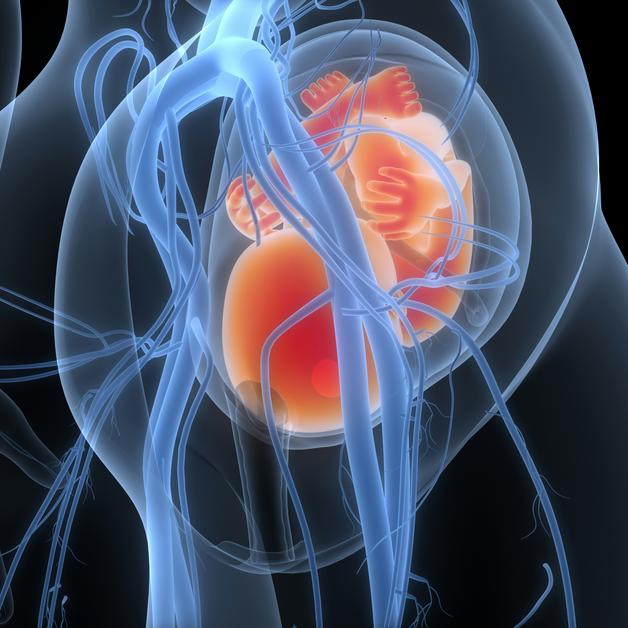
Imagine—the placenta, that extraordinary fetal lifeline, usually tucks itself safely along the upper uterine wall. With placenta previa, the placenta finds its spot close to, or covering, the cervix. Think of the cervix as the exit door for birth—when the placenta blocks that door (completely or even just at the edge), potential issues arise, especially as pregnancy advances.
How often does this scenario unfold? Current data highlights that placenta previa affects about 1 in 200 pregnancies. Sometimes, parents never see it coming—one moment, everything feels routine, and the next an ultrasound picks up the anomaly.
For many, a low-lying placenta seen early simply “climbs” upward as the uterus stretches, vanishing from the list of concerns by the final trimester. For others, the diagnosis remains, meaning regular ultrasounds, careful planning, and steadfast monitoring become essential companions on the road to delivery. This isn’t about blame; it’s about adapting. Spotting that vital sign—painless, vivid red bleeding beyond the pregnancy midpoint—can be transformative, offering a protective head start in seeking help.
Why does the placenta implant abnormally?
The reasons behind placenta previa are multifaceted, tangled with risk factors yet often surfacing with no obvious culprit. Consider these contributors:
- Uterine scarring—from a prior cesarean, removal of fibroids, or even surgical procedures like D&C—may disrupt the ideal landscape for placental attachment.
- Assisted reproductive technology may tweak implantation patterns. Hormonal factors, a uniquely shaped uterus, or being pregnant with twins or triplets nudge the odds higher.
- Age, too, plays a role: parents over 35, or those with a history of placenta previa, a high number of previous pregnancies, or certain lifestyle habits (smoking, cocaine use) find the risk notched up.
Still, most with these factors breeze through pregnancy without ever hearing the term placenta previa—while some, without any warning, meet it by chance. Migration—the gentle, upwards drifting of a low-lying placenta—remains a key phenomenon, so hope and attentive follow-up remain vital until birth.
Signs and symptoms: when to be alert
This condition’s signature is surprisingly distinctive. Suddenly, out of nowhere—often with no pain—a bright, red bleed presents itself after 20 weeks. Unlike the cramping stereotypically linked to miscarriage or placental abruption, placenta previa’s bleeding is silent and can erupt without any labor signs. Standing, sexual intercourse, light exercise, or simply the natural stretching of the uterus may be enough to trigger an episode.
Other clues? Occasionally mild anemia—paleness, fatigue—or even subtle uterine contractions, but without the telltale ache. The pain’s absence helps doctors distinguish placenta previa from other obstetric issues.
Never try a home inspection or self-examination if bleeding occurs—reach for medical support without delay. This simple step prevents sudden, severe complications, protecting both parent and child.
Does everyone notice symptoms? Strikingly, no. Many cases are discovered quietly, only because imaging uncovers a problematic location for the placenta. Even without a single spot of blood, attentive follow-up remains the best pathway to a safe delivery.
Diagnostic tools: the science of clarity
Ultrasound holds the key. Routine scans, first over the abdomen and then, increasingly, as pregnancy progresses, through the vagina for better precision, map the placenta’s position versus the cervix. There’s no need to worry—these internal ultrasounds are safe and provide the details that truly matter: is the cervix clear, partially covered, or completely hidden by placenta?
Sometimes, MRI comes into play. If a posterior placenta is hard to see or suspicion arises for a complication known as accreta, deeper imaging adds answers. Blood tests track any loss and ensure the parent remains healthy throughout.
Notably, the old-fashioned vaginal exam takes a back seat—if placenta previa is a possibility, stirring the area can trigger dramatic bleeding. Imaging leads the way, ensuring safety comes first.
The spectrum of placenta previa: types and delivery implications
- Complete placenta previa: The placenta entirely masks the cervix. Here, vaginal birth must be set aside, and cesarean delivery becomes the planned route.
- Partial placenta previa: With coverage of only a portion of the cervix, risk remains too high for vaginal birth—cesarean is scheduled in advance.
- Marginal placenta previa: The placenta grazes the edge of the cervix. In exceptional circumstances—when bleeding is absent and position remains stable—a vaginal birth may be considered, but only under expert observation.
- Low-lying placenta: The edge settles within a couple of centimeters of the cervix, yet doesn’t breach it. Some choose a careful attempt at vaginal delivery, always with a backup plan and open communication with the care team.
Each type shades the picture differently, but the unifying theme is safety first. When the cervix is even partly blocked, the risk of hemorrhage and the parent’s stability take precedence, guiding delivery decisions.
Risks and complications: what’s at stake?
For the parent, hemorrhage stands out—the body’s inability to control blood loss as the lower uterine segment stretches puts health at immediate risk. In rare cases, this spiral means blood transfusions or even hysterectomy—surgical removal of the uterus—to halt bleeding.
For the unborn child, the primary danger is prematurity. If heavy bleeding triggers a preterm birth, the baby faces challenges linked to immature lungs or low birth weight, sometimes requiring intensive support.
Placenta accreta spectrum steps in as a particularly complex concern when the placenta implants too firmly into the uterus—a scenario intertwined with placenta previa. Deep attachment can make placental separation at birth almost impossible, increasing the likelihood of major surgery.
Other associations, like abnormal fetal position, premature breaking of waters, or rare entities like vasa previa (where fetal vessels lie across the cervix), mean the care plan must flex and expand, responding to twists as they emerge.
Managing placenta previa: safety strategies for pregnancy
Once diagnosed, a clear shift may occur—activity modifications, rest periods, and more frequent monitoring start to define the rhythm of daily life. For some, home remains the safest setting; for others, hospital stays are advised, especially with recurrent or severe bleeds, or as delivery looms.
Anticipation is part science, part preparation. Corticosteroids may be administered to mature the baby’s lungs if premature birth seems likely. If contractions start too soon, certain medications can sometimes slow labor, unless bleeding is intense or non-stop.
As birth nears, delivery mode plans formalize—most with placenta previa, especially those falling into the complete or partial category, are offered a scheduled cesarean, usually around 36–37 weeks. When accreta is suspected, delivery is arranged in specialty centers, where advanced surgical teams and blood banks are prepared for any outcome.
Daily adjustments follow: strict activity restrictions, reliance on family or friends for practical support, careful watch for any new bleeding or contractions, and constant communication with healthcare providers.
Emotional well-being: caring hearts as much as clinical skills
Hearing the words placenta previa can tilt the emotional balance—swirling feelings of worry, guilt, or even shame may arise, sometimes without warning. These emotions don’t reflect failure but reveal a parent’s deep investment in their child’s future. Open conversations with healthcare teams build trust, dispelling myths and empowering parents to participate actively in decision-making.
Asking questions, voicing fears, or seeking psychological support represents strength, not weakness. Tapping into networks—partners, grandparents, friends, high-risk pregnancy communities—transforms burden into resilience. Sometimes, simply acknowledging uncertainty brings a new sense of stability.
Preparation takes many forms: organizing childcare, packing hospital bags, developing a clear birth plan, or finding time and space to process feelings all equip parents to face an unpredictable path with greater assurance.
Placenta previa and its look-alikes: differentiating related conditions
Clarity matters.
- Placenta previa: The placenta’s placement creates a bloodless, painless bleeding pattern, centered around the cervix, with risk peaking when labor approaches.
- Placenta accreta spectrum: Involves excessively deep placental attachment, which can trigger life-threatening bleeding at birth and frequently calls for complex surgery.
- Placental abruption: Unfolds as the placenta peels away from the uterine wall prematurely, marked by sharp pain, uterine rigidity, and acute risk for both parent and baby.
Understanding these nuances supports calm, practical decision-making—even amid uncertainty.
Key Takeaways
- Placenta previa describes a placental location covering or edging too close to the cervix, often picked up during a prenatal ultrasound.
- Its hallmark is sudden, painless vaginal bleeding—bright red, typically after 20 weeks gestation.
- Risks rise with prior uterine surgery, multiples, advanced parental age, assisted fertility, and certain lifestyle elements, but many cases occur without clear reason.
- Management revolves around regular scans, tailored delivery planning—cesarean for most, with rare exceptions for marginal or low-lying cases—and proactive monitoring of both parent and newborn.
- Emotional, practical, and informational support all help transform anxiety into confidence. Numerous resources, professionals, and community connections are available to guide and reassure.
- Download the Heloa app for tailored advice, free health questionnaires, and reliable information for every step of your journey—because facing placenta previa with knowledge and preparation makes all the difference.
Questions Parents Ask
Can I have sex if I have placenta previa?
Many parents wonder about intimacy during pregnancy, especially after a diagnosis like placenta previa. In most cases, healthcare providers recommend avoiding sexual intercourse when placenta previa is present, as it may trigger bleeding or contractions. It’s completely normal to feel unsure—don’t hesitate to ask your care team about what feels safe for you and your pregnancy. Open conversations help to reassure and support every parent’s unique situation.
Are there activities I should avoid with placenta previa?
When placenta previa is diagnosed, certain everyday activities may need to be adjusted for safety. Usually, it’s best to avoid heavy lifting, strenuous exercise, or anything that could put pressure on the lower pelvis. Pelvic rest—including skipping vaginal exams unless absolutely necessary—may be advised. If you’re unsure what’s safe, reach out to your medical team; together, you can tailor recommendations to your lifestyle and comfort.
Can placenta previa cause preterm birth?
Placenta previa can sometimes lead to preterm birth, mainly if significant bleeding occurs or if safety requires an early delivery. While this can feel worrying, il importe de rappeler that close monitoring, clear planning, and modern medical care all help reduce risks for both parent and baby. Every situation is unique, and your medical team will support you every step of the way, adapting as needed to keep you and your baby safe.

Further reading: