Feeling tethered to the bathroom, scrolling through endless advice, or lying awake and clocking another nighttime trip—frequent urination during pregnancy can quickly take center stage in daily life. Parents often juggle fatigue, uncertainty, and a barrage of physical changes, and amidst the whirlwind, a sudden need to urinate (sometimes hourly, sometimes in short bursts) may catch you off guard. Why does this happen? When should you worry? Are nighttime awakenings “just normal,” or could something else be going on? As bodies adapt to nourish and support new life, the bladder—once unassuming—finds itself at the heart of change. From physiological explanations rooted in increased blood flow and hormones, to solutions grounded in hygiene, pelvic floor health, and emotional support, discover the science and strategies for navigating frequent urination during pregnancy.
Understanding Frequent Urination During Pregnancy
What Is Frequent Urination During Pregnancy?
Imagine tracking your bathroom visits and noticing the count soar past 9—sometimes up to 15 times each day. This experience, medically termed increased urinary frequency, is a familiar companion for many expectant parents. Nocturia, defined as waking repeatedly at night to urinate, often intensifies the fatigue already present in pregnancy. What distinguishes this pattern? The urge: sudden, sometimes nearly overwhelming, involving even small volumes of urine. Many notice the feeling of an incompletely emptied bladder—a direct result of relaxed pelvic floor muscles and ongoing pressure from a growing uterus.
When Does It Begin? How Long Will It Last?
Curiously, frequent urination during pregnancy may set in as early as 6 to 8 weeks post-conception—sometimes before a positive test. In the first trimester, hormonal surges and the body’s effort to ramp up blood production become key contributors. As the uterus ascends into the abdomen during the second trimester, some relief might arrive… but as the third trimester looms and the baby’s weight nudges the bladder downward, the cycle typically returns. Post-delivery, the body eliminates accumulated fluids, and urination often spikes before returning to a pre-pregnancy rhythm within about 5 to 6 weeks. Still experiencing urgency after that? This warrants a discussion with a healthcare provider.
Recognizing the Signs
Short, recurrent bathroom trips. Waves of urgency, sometimes triggered by a simple laugh or sneeze. Interrupted sleep. Sometimes, a subtle (or not-so-subtle) leak. The sense of never feeling “done” even after using the bathroom. What unites these symptoms is their persistence—noticeably different from pre-pregnancy habits. While inconvenient, these sensations typically reflect physiological adaptations necessary for pregnancy.
Medical Explanations: Why Frequent Urination Happens
Blood Flow, Hormones, and Kidney Activity
Why the sudden need? During pregnancy, the body’s blood volume can surge by approximately 50%. This means greater kidney filtration as the body strives to process the extra load—more fluid processed equals more urine produced. Hormones, especially human chorionic gonadotropin (hCG) and progesterone, play pivotal roles. hCG stimulates increased blood flow to the pelvic region, dialling up bladder sensitivity. Progesterone—meanwhile—relaxes the smooth muscles of the bladder and urinary tract, increasing both urgency and the possibility of minor leaks.
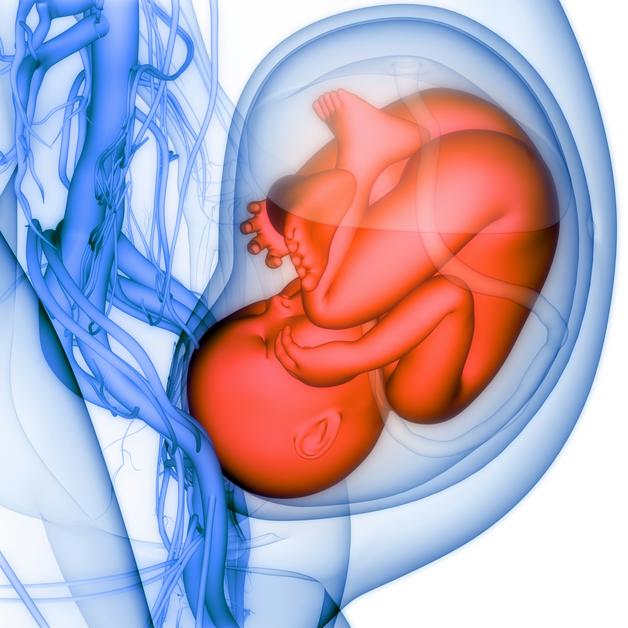
The Mechanics: Uterus and Bladder Dynamics
As pregnancy progresses, the uterus grows, encroaching on the bladder’s usual territory. The result? Diminished storage capacity and more frequent cues to empty. In early pregnancy, hormones dominate the landscape, while in late pregnancy, physical pressure becomes more pronounced—especially as the baby descends into the pelvis, crowding an already compressed bladder.
The Role of the Pelvic Floor
The pelvic floor is a group of muscles forming a supportive “hammock” for the bladder, uterus, and bowel. In preparation for birth, these muscles relax—enabling flexibility but reducing resistance against bladder pressure. If the bladder cannot fully empty, residual urine may accumulate, creating an environment more susceptible to bacterial growth and, potentially, infection.
Phases of Change: Frequent Urination Through the Trimesters
The First Trimester: Early Onset
From the earliest weeks, a cocktail of rising hormones and relaxing pelvic musculature may prompt more frequent bathroom visits. For some, this is the first physical sign of pregnancy, appearing before any visible changes.
The Second Trimester: Temporary Relief
As the uterus “lifts” into the abdominal cavity, bladder pressure can briefly ease. Not everyone experiences reprieve, however—individual anatomy varies, and for many, frequent urination during pregnancy persists regardless of trimester.
The Third Trimester: Pressure Returns
With the baby’s descent into the pelvis, bladder capacity reaches its lowest point. For many, this stage brings back repeated, often urgent, trips day and night. Fatigue from interrupted sleep is common, adding another layer of challenge.
Postpartum Period: Recovery and Recalibration
After birth, the body works hard to shed extra fluids retained during pregnancy. Temporary increases in urination are expected, but as hormonal levels stabilize and uterine size regresses, bathroom frequency typically returns to baseline by week six postpartum.
Differentiating Normal from Concern: Warning Signs
Not every change signals trouble, but parents should remain vigilant for:
- Dysuria (pain or burning during urination)
- Cloudy or foul-smelling urine
- Hematuria (blood-tinged urine)
- Persistent lower back or pelvic pain
- Fever or chills
- A sensation of never emptying your bladder, despite frequent attempts
- Sudden, ongoing loss of urine, or fluid leaks that are not urine
Such symptoms can point to urinary tract infection (UTI), cystitis, or, in rare cases, pyelonephritis (kidney infection). Untreated infections may compromise the wellbeing of both parent and baby, so prompt assessment is warranted—often beginning with a simple urine analysis.
Everyday Solutions: Prevention and Practical Tips
Smart Hydration
Continue drinking water regularly throughout the day, but consider dialing back intake after dinner to minimize nocturnal awakenings. Beware of caffeine and artificial sweeteners—they tend to irritate the bladder.
Bathroom Habits for Comfort and Safety
- Respond to bladder urges as soon as possible; holding urine can increase infection risk.
- Leaning slightly forward during urination can promote more complete bladder emptying.
- Emphasize front-to-back hygiene and consider urinating after sexual intercourse to further protect against infections.
Clothing, Environment, and Preparation
Opt for breathable cotton underwear and avoid restrictive clothing, which may encourage bacterial growth. When entering unfamiliar environments, locate restrooms in advance. If minor leaks occur, carry extra clothing or absorbent pads for emotional and physical reassurance.
Fueling Digestive Health
Fiber-rich foods can ward off constipation, which otherwise increases pelvic pressure and may exacerbate urinary frequency. Think whole grains, fresh produce, and gentle hydration.
Realistic Adjustments for Daily Life
Strategic bathroom visits—such as before outings—support confidence outside the home. A nightlight can transform nighttime bathroom trips, reducing stress and accidents. Periodically elevating your legs during the day may help prevent fluid accumulation, associated with increased nighttime urination.
Pelvic Floor Exercises: Foundation for Bladder Control
The Science and Technique of Kegels
Regular Kegel exercises—isolating and strengthening the pelvic floor muscles—are essential for bladder control before, during, and after pregnancy. Imagine pausing urine midstream (only as a mental cue)—hold the contraction 5 to 10 seconds, then release. Three sets daily, with focus on regularity over intensity, provide the best outcomes. Remember: doing these during active urination is discouraged, as this can lead to incomplete bladder emptying and promote infection.
Coping with Leaks
While absorbent pads can be practical for outings, they serve best as a complement—not a replacement—for ongoing pelvic floor training, which remains the gold standard for long-term support.
Preventing Urinary Tract Infections During Pregnancy
Couple prompt response to bladder urges with gentle hygiene:
- Use soft, unscented toilet tissues and avoid abrasive soaps
- Prefer loose, breathable clothing
- Change undergarments frequently
- Seek medical input if discomfort deviates from the norm—timely treatment is both effective and safe when indicated
Special Contexts: IVF and Frequent Urination
Undergoing in vitro fertilization (IVF)? The hormonal treatments involved can amplify urinary frequency. Enhanced medical monitoring offers reassurance, but foundational advice holds steady: maintain appropriate hydration, respond promptly to every urge, and remain attuned to any changes.
What If Frequent Urination Is Ignored?
Delaying urination or disregarding persistent urges can lead to bladder overdistention, promoting stagnant urine—a perfect environment for bacterial growth. Potential consequences? Infections, kidney involvement, or, in rare cases, premature labor. Attentive self-care always pays dividends.
Myths, Misconceptions, and Reassurance
Frequent urination during pregnancy is not a failing or a signal you’re “doing something wrong.” Restricting hydration is not the answer. Instead, balance fluid intake, prioritize movement, and adjust routines as needed. Inquiry with your healthcare team is always appropriate; no concern is too trivial. And remember—pelvic floor strengthening belongs not just to the postpartum period, but as a preventive and therapeutic practice, from early pregnancy onward.
Supporting Emotional Wellbeing
Physical symptoms like frequent urination during pregnancy can wear on patience, disrupt routines, or erode confidence. Acknowledging these feelings is the first step—these are genuine burdens. Open dialogue with loved ones and care providers, maintaining a symptom journal to track changes, or incorporating stress-soothing rituals such as walking, guided breathing, or gentle yoga, can all help to ground the experience. Partners matter, too—they can lend a hand in practical tasks, provide emotional encouragement, and join in activities to foster resilience.
Should anxiety or frustration become formidable, don’t hesitate to consult a healthcare professional or reach out to support networks.
Treatment and Return to Routine
If infection is diagnosed, antibiotics deemed safe for pregnancy are the mainstay of treatment. Persistent incontinence or urinary discomfort after six weeks postpartum invites further evaluation. Ongoing pelvic floor exercises and maintenance of supportive habits accelerate long-term recovery.
Key Takeaways
- Frequent urination during pregnancy arises from hormonal shifts, increased kidney activity, and physical changes linked to fetal growth.
- Attending promptly to bladder signals, practicing effective hygiene, and engaging in regular Kegel exercises can help diminish discomfort and stave off infection.
- Remain alert for warning signs—pain, fever, unusual urine, or persistent discomfort—these always merit medical attention.
- Recognize that every pregnancy follows a unique course, and even persistent urges are a valid reason to adapt your routines and seek guidance.
- Support, knowledge, and coordinated self-care tangibly boost comfort and peace of mind for both parents and growing families.
For tailored advice and practical health questionnaires for children, consider downloading the Heloa app—a valuable resource designed to support your family’s health journey.
Questions Parents Ask
Can frequent urination during pregnancy affect sleep quality?
Frequent trips to the bathroom at night are a common source of interrupted rest for many expecting parents. These awakenings can add to the fatigue already present during pregnancy and sometimes make it challenging to achieve deep, restorative sleep. While this experience may be temporary, it’s completely understandable that sleep routines feel disrupted. To ease the impact, you might try limiting fluids in the evening and keeping a gentle nightlight in the bathroom to make nighttime trips less intrusive. Remember, if sleep disruptions become overwhelming, sharing your concerns with a healthcare professional can offer additional reassurance and solutions tailored to your needs.
How can I differentiate between normal frequent urination and symptoms of a urinary tract infection during pregnancy?
It’s reassuring to know that needing to urinate more often is usually a natural part of pregnancy. However, if you notice pain or burning while urinating, cloudy or blood-tinged urine, fever, or a lingering feeling that your bladder is never fully emptied, these changes deserve gentle attention. Such symptoms may suggest a urinary tract infection, which is relatively common during pregnancy. In these situations, reaching out to your healthcare provider is always a wise and supportive step—many safe and effective treatments exist, and acting early can help protect your comfort and your baby’s well-being.
Are there foods or drinks that make frequent urination worse during pregnancy?
Certain beverages like coffee, tea, soft drinks, and drinks containing artificial sweeteners can irritate the bladder and increase the urge to urinate. Similarly, spicy or acidic foods sometimes have a stimulating effect on the bladder for sensitive individuals. You can try observing which foods or drinks tend to make symptoms more noticeable for you. Adjusting your diet gently, without restricting hydration, may bring a bit more comfort. Each pregnancy is unique, so finding the right balance that works for you is important—feel free to trust your instincts and consult your care team if you have questions.
Further reading: