Every expectant parent wonders—what shapes my baby’s development long before those first cries? The answer often lies deep within a barely visible world: the realm of prenatal sex hormones. From steering the earliest architectures of the brain to choreographing the formation of tiny reproductive organs, these chemical messengers are both silent designers and energetic sculptors. It’s natural to wonder whether hormonal shifts during pregnancy might affect your child’s behavior, health, or even future identity. Perhaps you’ve heard about conditions like congenital adrenal hyperplasia, or noticed fleeting signs—like a newborn girl’s brief vaginal discharge—and wondered, is this normal? The role of prenatal sex hormones is a blend of the expected, the mysterious, and the scientifically fascinating. Let’s illuminate the complexities, answering questions you may not even know you have, and offering practical guidance for every stage.
What are prenatal sex hormones? The unseen blueprint
Prenatal sex hormones—including androgens (testosterone, dihydrotestosterone), estrogens (estradiol, estriol, estrone), and progesterone—are biochemical powerhouses that shape your baby’s body and brain. These substances are created by your baby’s developing systems, the placenta, and, at times, your own maternal supply. Each hormone acts as an architect, guiding the differentiation of the gonads into either ovaries or testes, setting off a cascade of events that inspire the emergence of male or female internal and external genitalia. But their influence stretches far beyond the anatomy visible at birth.
Here is where the story becomes truly intricate: testosterone, originating mostly from fetal testes, surges between week 8 and week 24 of gestation. The effect? Construction of pathways in the brain—especially regions like the hypothalamus and amygdala—that will shape patterns of exploration, play, and even risk-taking later in life. Meanwhile, estrogens sourced mainly from the placenta and maternal contributions provide neuroprotective effects—shielding and nurturing neural growth. Each hormone, in a perfectly choreographed sequence, whispers instructions that build the physical and psychological blueprint that defines your child’s earliest foundations.
The timeline of influence: Critical periods and hormonal surges
Parents often ask—when do prenatal sex hormones matter most? The answer: windows of sensitivity, or “critical periods,” where hormonal actions shape long-term outcomes. Between weeks 6 and 12, and especially from week 8 to week 24, spikes in androgen (mainly testosterone) levels organize male reproductive structures and masculinize certain brain regions, even before these differences are visible in behavior.
Yet, the process is not limited to boys—girls, too, are influenced by nuanced patterns of hormone exposure. For example, the ovarian follicular reserve in female fetuses—essentially, a reservoir of potential eggs—peaks in number before birth, then diminishes gradually through life. The variety here is immense: millions of follicles dwindle to a mere few hundred in later adulthood. Estrogens and progesterone woven into this process support placental health, brain protection, and foundational reproductive capacity. The narrative? Hormonal choreography sets the tempo and rhythm, but the genetic and environmental “musicians” add countless variations.
The influence on your baby’s brain: From structure to behavior
How do prenatal sex hormones sculpt not just bodies, but personalities? Science paints a fascinating (and sometimes debated) picture. Testosterone’s surge influences development in sexually dimorphic regions—areas where male and female brains differ in structure and function. In both sexes, alteration of these hormone levels can lead to observable variations.
Consider girls born with congenital adrenal hyperplasia (CAH): here, increased prenatal androgen exposure often results in play preferences and behavioral patterns more commonly seen in boys. Studies link heightened fetal testosterone to a spectrum of traits—including increased spontaneous activity, certain cognitive abilities, and tendencies toward behaviors associated with autism or attention-deficit symptoms. Yet, it’s not a one-way street. Genetics, maternal health, and postnatal experience all help determine the child’s eventual path, underlining the sheer complexity parents must juggle—and the futility of blaming oneself for every twist and turn.
The physical story: Beyond anatomy
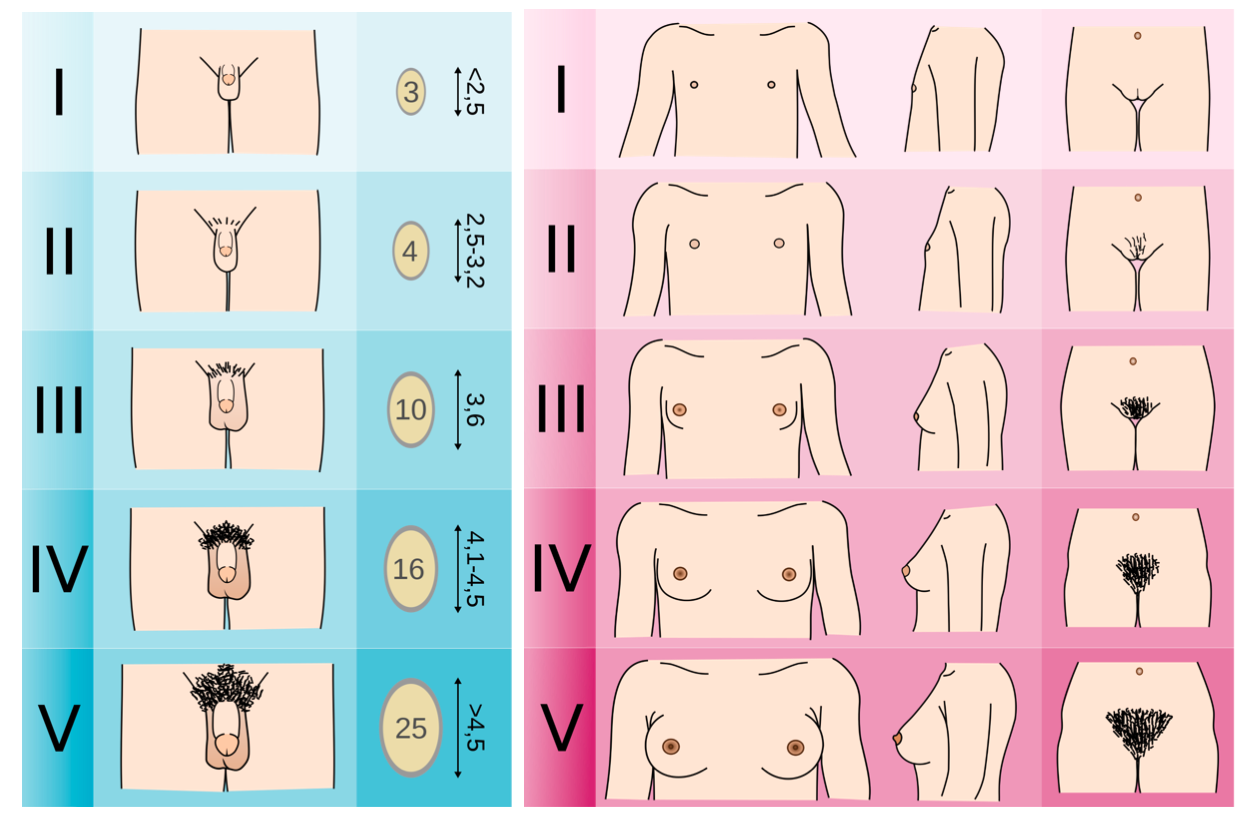
It’s easy to focus on the external, but the tale of prenatal sex hormones unfolds across the entire canvas of the body. Testosterone and androgens direct the formation of male reproductive structures; without such influence, female pathways develop by default. Interferences—be they genetic, medical, or environmental—may result in variations in genital appearance or function.
Moreover, these hormones don’t stop at reproductive systems. They leave fingerprints on muscle growth, skeletal formation, and even the method by which fat deposits shape the body over time. For parents of children born with differences of sex development (DSDs), awareness of these pathways provides empowerment—medical teams can offer targeted support, ensuring that each child’s unique configuration finds the best possible care.
Newborn changes: The “genital crisis” explained
You might be taken aback to see a brief vaginal discharge or even a spot of blood in your newborn daughter’s diaper. Far from rare, this “genital crisis” represents the sudden withdrawal of high maternal estrogen levels at birth—and a surge of infant-luteinizing and follicle-stimulating hormones as their own systems reboot. The result may be a mini “period” in the first days of life. Although unexpected, this is benign and self-limiting—a physiological echo of the hormonal theater that preceded birth.
For boys and girls alike, after the initial neonatal period, sex hormone activity settles into a relative dormancy, lying quiet until the hormonal overture of puberty begins years later.
Measuring and interpreting hormone exposure: Science meets challenge
When questions arise about a child’s development, you may hear about testing maternal blood, amniotic fluid, or even cord blood to estimate hormone exposure. Each method carries benefits and limitations. Maternal blood, for example, is easy to obtain but offers only an approximate reflection of actual fetal hormone concentrations, heavily filtered through the protective buffer of placental metabolism.
Sampling amniotic fluid grants a more direct window into fetal conditions but is invasive and offered only in select scenarios, typically for broader genetic testing. Cord blood tells a story right at birth, but not during those all-important “critical periods.” Sophisticated technologies like liquid chromatography–mass spectrometry (LC-MS/MS) enable precise readings even of very low hormone levels, but interpretation remains an art, requiring a knowledge of timing, context, and the body’s exquisite ability to regulate and compensate.
What shapes hormone levels? Genetics, maternal health, and environment
Prenatal sex hormones are influenced by an intricate interplay of genetics, biology, and environment. The XX or XY blueprint sketched from conception steers the destiny of the gonads: testes or ovaries. Genetic conditions—like those found in CAH—alter the trajectory, introducing higher than usual androgens. Maternal health, especially conditions such as polycystic ovary syndrome (PCOS), can amplify androgen exposure even further.
Yet, even the healthiest pregnancies experience change from the outside world—environmental endocrine disruptors, chronic stress, shifts in nutrition. The placenta emerges as a vigilant guardian, converting excess potent hormones into less active substances and modulating exposure. Recent advances in epigenetics highlight how gene expression, shaped without changing the underlying DNA, creates further layers of complexity. It is a delicate balance—sometimes unpredictable, always dynamic.
Neurodevelopment, behavior, and the broad spectrum of outcomes
Can prenatal hormone exposure shape neurodevelopment, influence future behaviors, even impact gender identity or sexual orientation? The science is clear: prenatal hormone environments modulate risk, not destiny. Increased prenatal testosterone correlates with a slightly higher incidence of autistic-like traits, or behaviors associated with ADHD, in both boys and girls. Research into DSDs, such as CAH or androgen insensitivity, demonstrates increased likelihood of non-heterosexual orientation or variations in gender identity—yet most individuals maintain gender identity and orientation typical for their sex assigned at birth.
Cultural, psychological, and social factors collectively interact with biology, reinforcing that identities are constructed through a multitude of channels. No laboratory measurement, no single test, can predict your child’s individuality. Every family’s story unfolds within a context of possibility, not prescription.
Ethical considerations and support: Respect, empathy, and empowerment
As a parent, it’s easy to feel overwhelmed when faced with medical jargon or stories of hormonal diversities. The most important lesson, however, is this: prenatal sex hormones contribute to the beautiful, sometimes bewildering spectrum of human variation, not to errors or deficiencies. Medical professionals are partners, offering genetic and physiological insights, but always within the context of observing and responding to your child’s unique temperament and needs.
Ethical best practices champion respectful, personalized care. Transparency, empathy, and affirmation empower families—particularly when facing unexpected diagnoses or differences in development. Ultimately, responsive parenting, open dialogue, and professional guidance pave the way for every child to flourish on their own terms.
Key Takeaways
- Prenatal sex hormones quietly orchestrate the formation of your baby’s reproductive organs, brain structures, and lay early foundations for personality and behavior.
- Genetic blueprint, maternal health—including conditions like PCOS—and environmental exposures all influence the hormonal environment in pregnancy.
- Laboratory results offer a fascinating glimpse into this undercurrent of development, but meaningful interpretation always depends on timing, context, and comprehensive care.
- Diversity in hormone exposure is universal—creating variation, not deviation. Each child’s pathway reflects a dance between biology and lived experience.
- Scientific inquiry continues to unlock new understandings, yet no single factor—genetic, hormonal, or environmental—determines fate.
- Compassionate, respectful, and flexible medical care supports families, whatever their journey holds.
- Reliable resources and dedicated healthcare professionals stand ready to accompany parents along every milestone and uncertainty.
- For continuous support, tailored advice, and health questionnaires designed for your child, you can download the Heloa app for free guidance and updates—empowering every parent to feel informed and confident, every step of the way.
Questions Parents Ask
Can prenatal sex hormones affect future fertility?
Fertility can be influenced by the prenatal hormonal environment, especially when there are significant hormonal imbalances. Sometimes, changes in fetal hormone exposure might alter the way reproductive organs develop or how many eggs a girl is born with, which may have an impact on fertility later in life. Most of the time, nature regulates these processes with remarkable precision. If you have concerns related to family history or specific medical conditions, you can always speak with your healthcare provider to receive personalized advice and support.
Do prenatal sex hormones influence the risk of certain health conditions later in life?
The environment in the womb, including levels of prenatal sex hormones, may have long-term effects on the risk of some health conditions such as polycystic ovary syndrome (PCOS), metabolic issues, or certain types of cancers. However, these are influenced by many factors, including genetics, postnatal environment, and lifestyle. Not every child exposed to higher or lower levels of particular hormones will experience problems. If you have a specific worry, discussing it openly with your healthcare team can help you feel supported and informed.