A diagnosis of Autism Spectrum Disorder (ASD) often sparks a storm of questions in parents’ minds. What do those early signs really mean? Does “spectrum” imply all experiences are the same? How do you know what support your child truly needs, and where to turn for answers grounded in evidence, not internet hearsay? The world of ASD is vibrant and nuanced, brimming with scientific discoveries, evolving care options, and deeply individual journeys. If you’ve found yourself wondering why your child repeats certain actions, shies away from noisy gatherings, or insists on sameness, you are far from alone in your concerns. Let’s delve into the essentials—key medical knowledge, lived realities, and indispensable tools—to help you move forward with confidence.
Understanding Autism Spectrum Disorder (ASD): The Spectrum Unveiled
What exactly does it mean when clinicians speak of Autism Spectrum Disorder (ASD)? The phrase “neurodevelopmental condition” may sound technical, but it simply signals a difference in how the brain develops and interacts with the world, especially regarding social interaction, language, and behavior. There’s no single way ASD presents itself; one child may speak with ease yet avoid eye contact, another may be non-speaking but light up around familiar faces. Roughly 1 in 100 children globally, and up to 1 in 31 in the United States, will be diagnosed with ASD—numbers that reflect heightened awareness and refined screening, not an “epidemic.”
Notably, ASD is about variability—heterogeneity is a hallmark. Intellectual and verbal abilities span from minimal speech to advanced vocabulary. Some children display intense preferences or rituals, while others quietly observe from the periphery. Sensitivities to sounds or textures, a fascination for spinning objects, or an uncanny memory for details might coexist with struggles to understand playmates’ facial expressions. Autism does not “look” one way.
The prevalence discrepancy between genders is striking: ASD is diagnosed three to four times more commonly in boys, yet specialists now recognize that girls often fly under the radar due to subtler cues and adeptness at masking difficulties. This diversity challenges stereotypes and demands personalized support.
Recognizing ASD: Symptoms, Signs, and What to Watch
Social Communication and Interaction
Does your child seem lost during group play or rarely join in back-and-forth chatter? Deficits in social reciprocity—the natural give-and-take of interaction—form the backbone of ASD. Limited eye contact, few gestures like pointing, and difficulty “reading” emotional cues frequently emerge early. Conversations may feel one-sided, or filled with misunderstood idioms.
Repetitive Behaviors and Restricted Interests
Hand-flapping, rocking, or insistent adherence to routines are more than “quirks”—they are often self-stimulatory behaviors (known as “stimming”) offering comfort or emotional regulation. Deep interests, whether for train schedules or dinosaur facts, can consume hours. Some children echo speech (echolalia), while others line up toys or become visibly distressed at unexpected changes.
Sensory Features and Early Childhood Clues
Heightened responses to noises, aversion to certain clothing fabrics, or refusal to participate in familiar games may seem puzzling at first. Delayed babbling, lack of response to one’s name, or an absence of spontaneous smiles or mimicry (think “peek-a-boo”) warrant gentle observation. It’s not about missing milestones by a set age, but watching for persistent, meaningful differences in communication and play.
Variability: Gender, Age, and Individuality
Here’s a compelling question: Why are girls so often diagnosed late, sometimes even in adulthood? Girls with ASD may demonstrate less visible repetition or compensate by mimicking socially adept peers. As school or social demands rise, difficulties can become more apparent, shifting the “diagnostic window.”
Causes and Risk Influences: Genetics Meets Environment
Genetic Foundations and Heritability
Science has advanced rapidly. Twin and family studies consistently reveal a strong genetic component, involving many genes (polygenic) rather than one culprit. Rare single-gene disorders, such as fragile X, can explain a subset of ASD cases. Yet, the interplay of genetic “susceptibility” is tangled and individualized.
Prenatal and Environmental Factors
Fast-paced parental lives, higher maternal or paternal age, and exposures such as gestational diabetes, specific medications (valproate), preterm birth, or increased environmental stressors (like air pollution) act as modifiers, not standalone triggers. Genetics sets the stage; the environment shapes the scene.
Disputing the Myths
Vaccines? Resounding scientific consensus, built on large-scale studies from reputable institutions (CDC, WHO), confirms absolutely no link between vaccines and ASD. The earlier myth connecting the MMR vaccine to autism has been categorically debunked. Avoiding vaccines puts all children at greater risk—there’s no health benefit for ASD prevention.
Diagnosis: From Screening to Multidisciplinary Insight
How ASD is Diagnosed
There’s no blood test for ASD. Diagnosis combines careful observation, comprehensive parent interviews, and standardized tools such as the Autism Diagnostic Observation Schedule (ADOS) and the Autism Diagnostic Interview-Revised (ADI-R). These instruments measure social engagement, repetitive actions, language, and play, while other assessments capture cognitive strengths and adaptive abilities.
A multidisciplinary team—pediatricians, psychologists, speech and occupational therapists—ensures a well-rounded evaluation, considering possible co-existing conditions like anxiety, ADHD, or epilepsy.
Special Challenges: Girls, Women, and Adults
Girls often slip through the cracks: less overt stimming, better camouflage, and interests that veer toward the socially “acceptable” mean diagnosis can be delayed by years. Adults, who may have built up coping strategies, also experience frequent mislabeling.
Spectrum of Support Needs
ASD encompasses a vast range of support levels:
- Level 1 (needing some support): Communicates clearly but struggles with nuanced social situations.
- Level 2 (requiring substantial support): Has marked verbal, nonverbal, or behavioral challenges.
- Level 3 (requiring very substantial support): May be non-speaking, highly dependent, and require daily tailored care.
Associated Conditions: The Broader Picture
Many children with Autism Spectrum Disorder (ASD) experience additional medical or psychological issues—comorbidities. Anxiety affects approximately one in five, attention difficulties abound (ADHD and ASD frequently overlap), and some may show symptoms reminiscent of Obsessive-Compulsive Disorder (OCD). Intellectual disabilities are present in about a third, while others thrive with average or above-average cognitive ability.
Epilepsy (involuntary electrical activity in the brain) affects 10%, gastrointestinal complaints like chronic constipation surface often, and sleep disturbances are notorious—sometimes caused by heightened sensory sensitivities. Recognizing and addressing these is paramount; they impact well-being, behavior, and education.
Evidence-Based Interventions and Support Strategies
Behavioral and Developmental Therapies
Applied Behavior Analysis (ABA) remains a widely validated intervention, aiming to increase adaptive behaviors and curb those that interfere with daily living. Younger children benefit from Early Intensive Behavioral Intervention (EIBI) and hybrid models, like the Early Start Denver Model, which combine play-based learning and skill-building in naturalistic settings.
Pivotal Response Treatment (PRT) leverages children’s own motivation and interests, enhancing communication and social skills through daily activities.
Communication, Language, and Alternative Systems
Speech therapy spans spoken language work to facilitating communication via augmentative and alternative communication (AAC) devices or sign language, especially for non-speaking children.
Occupational, Sensory, and Daily Living Supports
Occupational therapy builds independence—self-care (feeding, dressing), sensory integration (tolerating sounds, lights, crowded environments), and fine motor skills. Sensory diets curate tailored input, providing relief and improving participation in routines.
Educational Planning
A bespoke plan is essential. Individualized Education Programs (IEPs), visual supports, and structured teaching methods like TEACCH optimize classroom participation. Cognitive Behavioral Therapy (CBT) addresses anxiety and helps manage emotions or transitions.
Medication Considerations
No medication treats core ASD features, but targeted options exist for severe irritability (risperidone), symptoms of ADHD, anxiety, or sleep disorders. Risk-benefit is assessed case by case, with thorough monitoring for side effects.
Alternative and Emerging Therapies
Sound therapies, music, mindful movement, and animal-assisted interventions generate interest but must be scrutinized for evidence. Caution: Approaches like chelation or hyperbaric oxygen lack scientific backing and may present safety hazards.
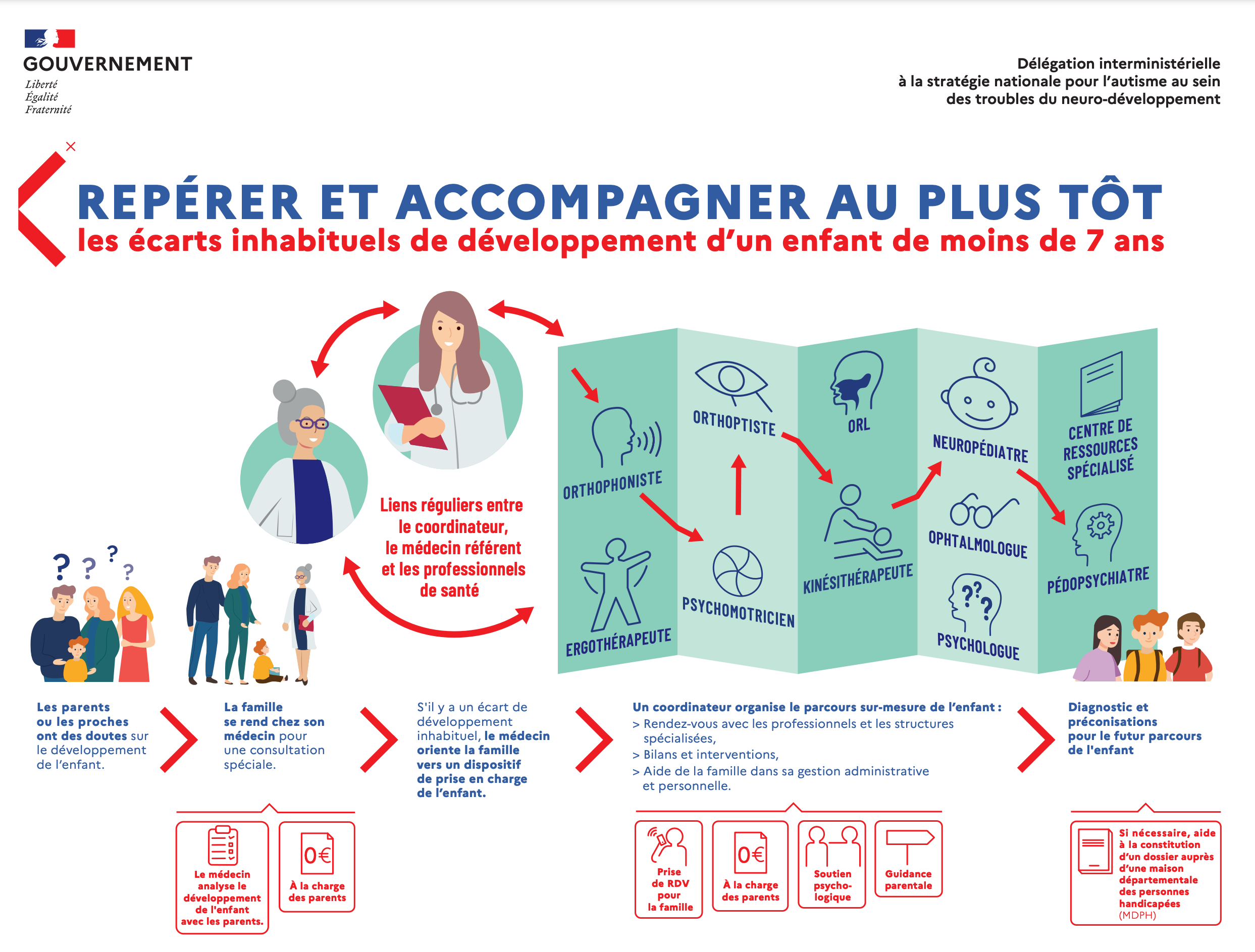
Early Identification and Coordinated Care Pathways
When a child struggles with language, learning, or social engagement, early monitoring is the gold standard. Parents, as keen observers, play a vital role here. Primary care visits initiate developmental surveillance, screening, and, if needed, referrals to specialist teams—developmental pediatricians, speech therapists, psychologists—who collaborate to assess strengths and challenges.
Specialized care platforms, where multidisciplinary teams create individualized intervention plans, help parents avoid going it alone or feeling lost in a maze of appointments. Developmental tracking at home, guided by evidence-based resources, maximizes progress and adaptation.
Care pathways often interweave supports for other neurodevelopmental disorders—dyslexia, dyspraxia, ADHD, intellectual disabilities—ensuring a holistic approach.
Life with Autism Spectrum Disorder (ASD): Strengths, Hurdles, and Day-to-Day Experiences
School and Employment
Children and teens with ASD often shine in areas like memory, detail-spotting, or technical interests—sometimes revealing true “spiky profiles” where certain skills outpace others. Sensory-aware classrooms, patient educators, and thoughtful job coaching unlock these talents.
Social Relationships
Making and sustaining friendships can prove daunting, but skill-building—like social stories or interest-based groups—can help. Instead of molding children to “fit in” at all costs, the focus trends toward celebrating diverse social styles and supporting community connection.
Independence and Routine
Predictable routines don’t just bring comfort—they buffer anxiety. Occupational therapy, life skills coaching, and gradual exposure to new challenges encourage genuine autonomy, shaped by each child’s developmental pace.
Sensory Adaptations
Think designated quiet corners, fidget objects, visual timetables. Small environmental tweaks can transform daily life—making parties, classes, and family outings less overwhelming.
Celebrating Neurodiversity
Spotlighting a child’s strengths—artistic flair, number sense, vivid visual thinking—nurtures confidence. Self-advocacy grows naturally when children are heard and accepted for who they are, rather than what they’re not.
Advocacy, Inclusion, and Social Change
From schools embracing inclusive practices to national groups fighting stigma, the world is gradually moving toward accepting, valuing, and uplifting the contribution of people with Autism Spectrum Disorder (ASD). As awareness shifts, so do opportunities for meaningful participation on every level.
Family and Caregiver Support: Guidance Without Judgment
Coping with Diagnosis and Daily Life
Hearing the words “Autism Spectrum Disorder (ASD)” brings a rush of emotions. Relief at finally having an explanation may intermingle with uncertainty. Adjustment is a process, not a moment. Parents, siblings, and caregivers will all need time—and practical help.
Accessing Resources
Healthcare professionals knowledgeable about ASD, supportive educators, and experienced therapists form a scaffolding for the whole family. Early intervention, clear record-keeping, and Individualized Education Programs (IEPs) ease the journey.
Finding Your Network
Parent support groups, community resources, and specialist clinics are more than lifelines; they are spaces for honest questions and shared tips. Advocacy groups demystify legal rights, educational access, and break down the red tape surrounding care.
Family Well-Being and Self-Care
Balancing a child’s support needs with those of siblings and personal well-being is not an indulgence—it’s essential. Family routines, counseling, peer connection, and moments of rest matter profoundly.
ASD Across the Lifespan: Evolving Needs, Ongoing Support
Childhood
Early years witness the richest developmental shifts—language acquisition, play, emotional growth. ASD may color these with unique shades but does not preclude joy or skill-building. Evidence-based intervention can foster enduring progress.
Adolescence
Puberty brings new uncertainties. Identity, self-awareness, emerging independence: autistic teens may find this stage turbulent, especially when navigating friendships or mental health challenges. Family and professional support remain pillars.
Adulthood
Adulthood is not an afterthought. While some autistic adults thrive independently, others require structured support for daily living or work. Recognition of individual preferences replaces one-size-fits-all objectives.
Aging
Aging with ASD may surface fresh medical, cognitive, or community needs. The landscape for older autistic adults is growing, with healthcare increasingly respectful of neurodiversity and personal dignity.
Medical Advances, New Perspectives, and the Future
Genetic and Neurobiological Breakthroughs
Research highlights: hundreds of gene variants, altered neurotransmission, and new insights into neural connectivity underpin our understanding of Autism Spectrum Disorder (ASD). Diversity in brain structure is not a flaw, but a facet worthy of acceptance.
Screening, Diagnosis, and New Models
Earlier, more sensitive screening tools empower access to supportive therapies at the right time. “Normalization” is no longer the ambition—instead, maximizing each individual’s well-being and autonomy takes center stage.
Embracing Neurodiversity
Once seen simply as a disorder, Autism Spectrum Disorder (ASD) now embodies a valued form of neurodiversity. Advocacy movements, self-advocate voices, and public awareness campaigns reshape not only policies but public attitudes.
Policy and Global Action
International organizations and advocacy networks partner to expand healthcare, educational opportunities, address stigma, and enshrine the rights of autistic individuals—laying the foundation for a more inclusive society.
Key Takeaways
- Autism Spectrum Disorder (ASD) reflects a spectrum, not a single story: each child’s strengths, challenges, and support needs are unique.
- Early recognition, coordinated intervention, and evidence-based therapies can optimize developmental, emotional, and educational progress.
- Symptoms and strengths shift with age, vary by gender, and evolve as demands change.
- No single test or intervention suffices—the best outcomes stem from personalized, multidisciplinary approaches.
- Family support, well-being, and advocacy are just as important as clinical care: parents and caregivers deserve compassionate, practical guidance throughout the journey.
- Resources, supportive communities, and health professionals are available to help families foster each child’s full potential. For additional support, personalized advice, and free health questionnaires for children, parents can download the Heloa app.
Questions Parents Ask
Can children with Autism Spectrum Disorder (ASD) form emotional attachments?
Absolutely. Children on the autism spectrum can and do develop strong emotional bonds with parents, siblings, caregivers, and even peers. However, the way they express affection or attachment may sometimes differ from what is typically expected. Some children may show their love through actions rather than words or eye contact, while others might express their feelings uniquely or subtly. Each connection is meaningful, even if it looks different from what you might have anticipated—your presence and understanding play an essential role in nurturing these bonds.
Does Autism Spectrum Disorder (ASD) only affect childhood, or does it continue into adulthood?
ASD is a lifelong neurodevelopmental difference, not restricted to childhood. While early signs and challenges might be most noticeable during young years, autistic traits and individual support needs often evolve as a child grows into adolescence and adulthood. Many autistic adults lead fulfilling, independent lives, sometimes requiring specific accommodations or support in social, educational, or professional settings. Rassurez-vous—people with ASD continue to learn, adapt, and thrive at every stage of life, with the right support and environment.
Are there activities or therapies parents can do at home to support a child with ASD?
Yes, and even small daily actions can make a big difference! Encouraging routines, offering clear visual cues, and breaking tasks into simple steps can provide structure and security. Engaging in shared interests—like reading together, building with blocks, or exploring sensory-friendly play—strengthens connection and fosters communication. Using positive reinforcement (such as praise or favorite activities) to support progress, and gently introducing new experiences, helps children build confidence in a safe space. Try to celebrate small successes and remain patient—every step forward matters. If you have questions or need guidance, don’t hesitate to connect with professionals who can offer tailored recommendations.
Further reading:









