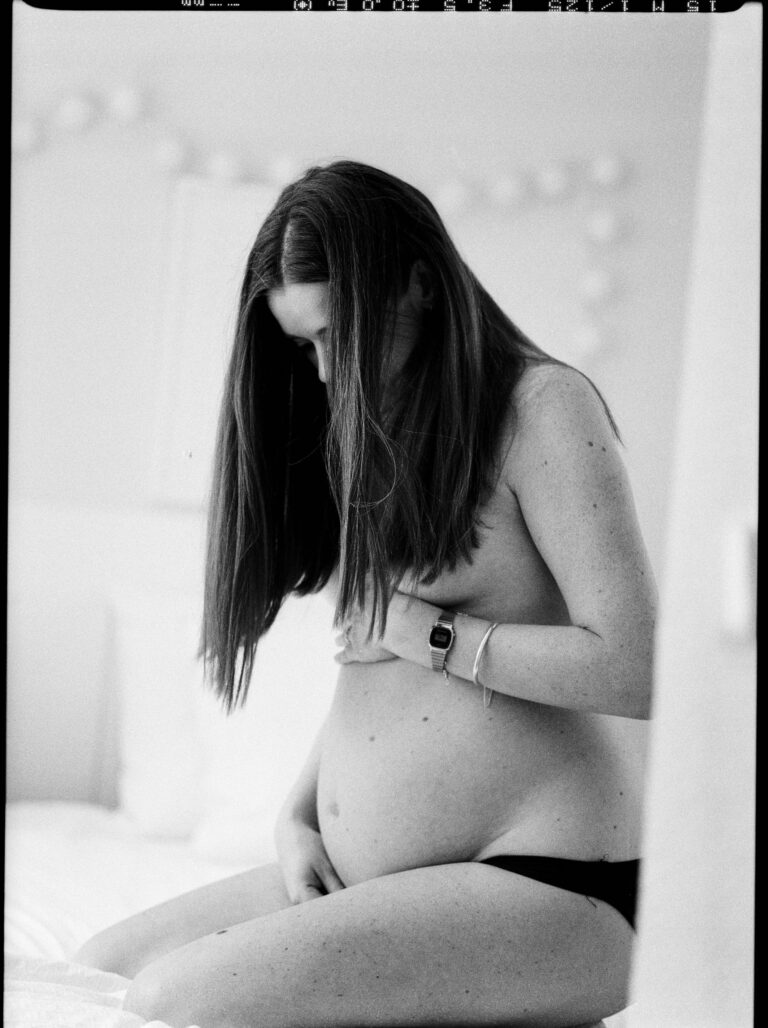
A woman’s body is a landscape of signals—some expected, others astonishingly silent. For many expectant parents, the milestones of pregnancy appear as clear signposts: the first flutters of movement, a slowly rounding belly, subtle (or striking) shifts in mood and energy. Now imagine, amidst the rush of ordinary days, that these signs are missing or misinterpreted. Denial of pregnancy—an experience as bewildering for families as it is for medical professionals—upends expectations and raises questions that can feel overwhelming. How could such a profound transformation pass unnoticed? What does this mean for the health of your partner and your baby? Questions spiral. Answers, fortunately, exist—and understanding is the first step. Here, you’ll find an exploration of what denial of pregnancy actually means, its causes, and how parents can approach discovery, support, and medical care with confidence and compassion.
What Is Denial of Pregnancy?
You may have heard the terms cryptic pregnancy or concealed pregnancy and wondered if these are just rare, sensational cases. Not quite. Denial of pregnancy lies at the intersection of physical biology and psychological protection—a woman carries a baby but remains unaware of her pregnancy. The body offers muted or atypical signals, and the mind, often subconsciously, shields itself from recognizing them.
This condition can stretch through months—even up to the day of delivery—without the expected ballooning abdomen or classic signs like morning nausea, breast tenderness, or distinct fetal movements. Some women maintain regular bleeding, much like a menstrual cycle, or attribute symptoms to stress, lifestyle, or other medical causes. Surprising? Absolutely. But statistics are telling: studies estimate that about 1 in 475 pregnancies reach the halfway mark without acknowledgment, and in rarer cases, some pregnancies remain unrecognized until labor itself.
Types and Psychological Subtleties
Denial of pregnancy doesn’t wear a single face. It ranges across a spectrum and includes both medical and psychiatric nuances.
- Partial denial: Recognition dawns between the fourth and ninth month—late, but before childbirth.
- Total denial: Awareness breaks only as labor begins.
Psychologists add further layers:
- Psychotic denial (rare): Deeply entwined with severe psychiatric disorders—schizophrenia, severe bipolar illness—where delusions may actively reinterpret physical symptoms.
- Non-psychotic denial: Far more common. Here, the mind distances itself from bodily reality as a defense (often called emotional denial), or simply doesn’t connect the sensations to pregnancy (sometimes termed pervasive denial, where both body and emotions are silent, or affective denial, where the mind knows but the heart cannot connect).
Concealed pregnancy warrants its own mention—a scenario where a woman is fully aware, but hides the pregnancy, often because of social, cultural, or private reasons. In sharp contrast, the phenomenon known as a “nervous pregnancy” flips the scenario: symptoms arise, but no fetus is present.
How Does the Baby Grow in Denial of Pregnancy?
From a medical perspective, it becomes even more fascinating—and perplexing. Ordinarily, the uterus expands outward, pushing against the abdominal wall, clearly visible by the midpoint of gestation. In denial of pregnancy, this physical growth may progress vertically along the spine, eluding both visual and tactile detection. The fetus develops normally, hidden in plain sight. Once recognition surfaces, physical changes can appear rapidly—sometimes abdominal muscles relax and the belly rounds out within hours or days, as if the body had pressed “pause” on outward signs.
Roots: What Drives Denial of Pregnancy?
No single thread explains every case. Instead, think of an intricate web where psychological, biological, and social strands are tightly woven.
- Psychological drivers: The mind sometimes shields itself from realities that provoke intense anxiety or threaten identity. Unresolved trauma or previous abuses (notably sexual trauma in childhood or adolescence), feelings of ambivalence toward motherhood, or overwhelming life stress can all contribute.
- Social forces: Family expectations, social stigma, and fear of judgment can render pregnancy unthinkable or intolerable.
- Biological elements: Hormonal fluctuations may suppress typical symptoms—continued or irregular menstrual-like bleeding, minimal weight changes, lack of abdominal growth. Contrary to common belief, denial of pregnancy does not spare women with prior pregnancies, nor is it exclusive to any specific age or body type.
Mulling over the possibility of pregnancy doesn’t create denial; reflection is a sign of awareness, not repression.
Signs and Presentation: The Invisible Pregnancy
Curious about what denial of pregnancy actually “looks like”? Physical cues may be faint, absent, or misinterpreted, making the condition remarkably discreet:
- No clear weight gain
- Little to no visible bump
- Absent or underestimated typical symptoms—nausea, fatigue, appetite changes
- Perceived or actual menstrual bleeding
- No felt fetal movements, or these sensations are dismissed as digestive shifts
Diagnosis can be delayed, sometimes discovered only when contractions start or labor unfolds—an emotionally charged scenario for parents and professionals alike.
The Diagnostic Puzzle and Medical Support
Even when the mind denies, biology is stubborn. Pregnancy tests—urine and blood—turn positive. Ultrasounds reveal the unmistakable presence of a developing fetus. Yet the absence of obvious symptoms, and an account that erases the possibility, mean many cases escape detection until late pregnancy or delivery.
Healthcare professionals who encounter unexplained physical, emotional, or behavioral changes in women of childbearing age may consider pregnancy testing as a default. Beyond the physical assessment, a truly supportive response demands an integrated approach: obstetric care, mental health support, and social services acting together.
Involving partners and family deserves more than a passing mention—rarely do loved ones suspect pregnancy before the dramatic reveal. They, too, can be caught in a whirlwind of shock, confusion, and adjustment.
Emotional Consequences and Psychological Recovery
The emotional fallout after denial of pregnancy can be seismic. Late discovery—sometimes during the birthing process—brings waves of guilt, disbelief, relief, or even trauma. Denial may have protected against emotional overload, but reality’s sudden return asks parents to process dramatic change overnight.
Support isn’t just luxury—it’s protective. Psychological care bolsters parental confidence, addresses guilt or anxiety, and smooths the mother-infant bond’s rocky introduction. Many mothers develop profound, even “hyper-protective” relationships with their infants, compensating for the months lost to unawareness. Yet frustration, sadness, and self-questioning are entirely normal. External reassurance and gentle guidance from mental health professionals or trusted family members can steady the transition and reduce risks of postpartum depression or strained attachment.
Medical and Neonatal Challenges after Denial of Pregnancy
The absence of prenatal care is the most pressing medical risk linked to denial of pregnancy. Without check-ups, nutritional advice, or monitoring, preventable complications can multiply:
- Higher rates of unplanned, unattended childbirth—sometimes in unsafe environments
- Increased likelihood of maternal hemorrhage, infection, and trauma
- Newborn complications: prematurity, low birth weight, growth restriction, and in rare cases, increased need for neonatal care
A stark point sometimes raised: where denial overlaps with severe psychiatric disturbance, risks of neglect or harm exist—though these are exceptional.
Family Reactions and Support Strategies
Discovery may transform family dynamics overnight. Most often, strong bonds form, even if tinged by anxiety or protectiveness. Open communication, reassurance, and the involvement of partners and extended family foster resilience. Social support groups, community healthcare teams, and mental health resources dampen isolation and help parents rebuild confidence. Seeking professional advice—without fear of stigma—can speed emotional adjustment and encourage a secure, nurturing environment for the child.
Legal and Ethical Nuances
Legal and ethical considerations can be nuanced, especially if mental health impairs capacity for consent or decision-making. Priorities include honoring a woman’s autonomy while safeguarding her wellbeing and the baby’s rights, particularly in emergencies near delivery. Mandatory treatment is rare, and used only in exceptional circumstances where severe incapacity is present. Collaboration between ethics panels, medical experts, and sometimes legal advisors guides respectful, balanced decisions.
Prevention, Education, and Raising Awareness
Empowering professionals and future parents through education stands out as a powerful remedy. Training healthcare providers to consider pregnancy—regardless of a woman’s account or lack of typical signs—boosts early detection and support. Public campaigns reduce stigma, encourage timely help-seeking, and reassure families that support exists, whatever their situation or feelings about parenthood.
Advocacy for comprehensive postnatal follow-up and mental health resources makes a measurable difference, smoothing recovery and building confidence after even the most unexpected journeys to parenthood.
Key Takeaways
- Denial of pregnancy is more frequent than most realize, with physical and psychological underpinnings that can confound even experienced parents.
- Physical signs may be muted or absent, and both women and families can remain unaware until late pregnancy or delivery.
- Underlying causes are a mix of psychological, biological, and societal forces—no single factor has all the answers.
- Support—from professionals, families, and communities—quickly reduces shock, promotes adaptation, and protects the health and confidence of both parent and child.
- Awareness among healthcare workers, regular consideration of pregnancy when symptoms are unclear, and open family conversations build safety and resilience.
- Dedicated resources, compassion, and early intervention shape the best outcomes—medical, psychological, and emotional.
- For personalized advice, practical tips, and free child health questionnaires, download the Heloa app and discover everyday tools designed to support parents like you.
In the end, while denial of pregnancy may seem shrouded in silence, clear information, trusted support, and proactive care can illuminate the path from confusion to confident, loving parenthood.
Questions Parents Ask
Can denial of pregnancy affect future pregnancies?
Denial of pregnancy does not automatically repeat itself in future pregnancies. Each experience is unique and shaped by individual, emotional, and situational factors. If you or someone you love has experienced denial of pregnancy, seeking attentive support—whether psychological or medical—can reassure and guide you for a future pregnancy. Remember, many women go on to have typical pregnancies afterwards without recurrence of denial.
How can partners or family members support someone going through denial of pregnancy?
Support from loved ones plays an essential role. It’s important to listen without judgment and offer reassurance rather than express surprise or disappointment. Gently suggesting medical follow-up, being available to talk through worries, and simply letting the person know they are not alone can make a big difference. If needed, encouraging professional psychological support may ease the transition and help everyone adjust to new feelings and responsibilities.
Does denial of pregnancy occur only in certain age groups or backgrounds?
Denial of pregnancy can affect women of any age, background, or life situation. There is no single profile. Emotional challenges, stress, stigma, or specific circumstances may contribute, but the phenomenon is not restricted to a particular group. The most important thing for families to remember is that experiencing denial does not reflect a personal failing or weakness—each journey is different, and support is always available.