Pregnancy can feel like a long test of stamina—nausea that refuses to settle, anxiety that spikes at night, sleep that breaks into short fragments, back pain, headaches, and a body that feels constantly “on”. It is no surprise that CBD pregnancy is searched so often, especially when CBD is marketed as calming, “non-intoxicating,” and easy to buy.
But CBD is not a harmless home remedy. Cannabidiol is biologically active, pregnancy physiology changes drug handling, and fetal exposure is possible. The safest plan is often to step back, understand the main unknowns, and discuss symptom-specific options with your obstetrician, midwife, or pharmacist.
CBD pregnancy: why people consider it
Common reasons
Many expecting mothers explore CBD pregnancy products hoping for relief from:
- nausea and poor appetite
- anxiety, panic sensations, constant worrying
- insomnia and frequent night waking
- headaches/migraines
- back pain, pelvic girdle pain, body aches
Access also plays a role. CBD products are heavily marketed, available online, and sometimes framed as an alternative to prescription medicines.
A gentle reminder
Wanting relief is understandable. The difficult part with CBD pregnancy is that benefits are uncertain, while exposure to the baby can occur. A quick conversation with a clinician can clarify what you are trying to treat and what has better pregnancy safety data.
CBD, cannabis, hemp: clear definitions
CBD vs THC
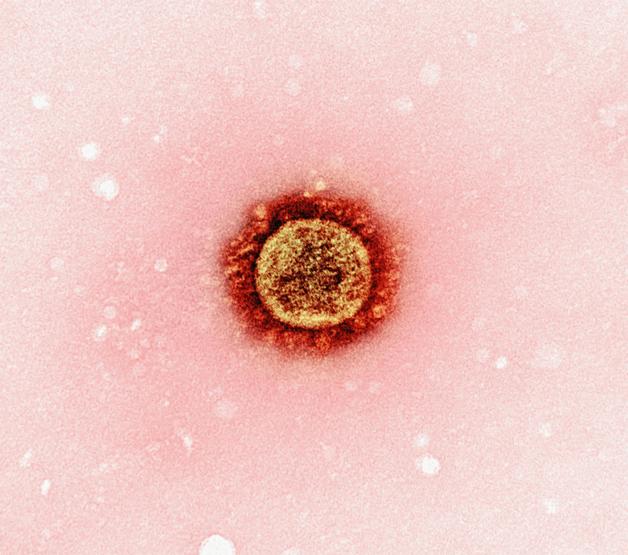
CBD (cannabidiol) and THC (tetrahydrocannabinol) come from Cannabis sativa.
- THC causes intoxication, crosses the placenta, and is discouraged in pregnancy because of concerns around fetal growth and neurodevelopment.
- CBD is not intoxicating, but “not intoxicating” does not mean “safe.” Human data for CBD pregnancy are limited.
What “hemp” really means
“Hemp” generally means cannabis with low THC, not zero THC. In pregnancy, repeated small traces can still become a sustained exposure.
Hemp seed oil vs CBD oil
- Hemp seed oil: mostly fats, not a reliable source of CBD.
- CBD oil: an extract intended to contain measurable CBD (sometimes with other cannabinoids).
Mislabelling matters in CBD pregnancy because it can mean hidden THC.
Full-spectrum, broad-spectrum, isolate, “THC-free”
- Isolate: mainly CBD (quality control still matters)
- Broad-spectrum: multiple cannabinoids with THC removed, traces may still happen
- Full-spectrum: wider plant compounds, THC may be present
- “THC-free/0% THC”: depends on the test method and batch stability
How CBD acts during pregnancy
The endocannabinoid system (ECS)
The ECS is a signalling system with receptors (CB1/CB2), natural messengers (like anandamide), and enzymes. It is involved in appetite, mood, pain, inflammation, and sleep.
In pregnancy, ECS signalling also participates in implantation, placental function, and parts of fetal neurodevelopment. That is why clinicians are cautious about CBD pregnancy: altering signalling during a tightly regulated phase may have unintended effects.
Why “unknown” is not neutral
Preclinical studies suggest cannabinoid exposure can affect placental transport and fetal development pathways. Animal findings do not automatically apply to humans, but they explain why safety cannot be assumed.
What research says about CBD pregnancy
Human data gaps
High-quality human evidence specific to CBD pregnancy is scarce. There are no strong trials to define a safe dose, a safe timing window, or long-term child outcomes.
Real-world reports are difficult to interpret because products, doses, and THC contamination vary.
CBD-only research vs cannabis research
Many pregnancy studies are about cannabis where THC is the main exposure, sometimes with smoking/vaping as an added variable. THC has clearer evidence of risk and is widely discouraged.
For CBD-only, preclinical research raises questions, but translation to human pregnancy is uncertain.
Key unknowns
Parents often want a simple answer. The reality for CBD pregnancy is unanswered questions:
- what dose leads to fetal exposure?
- which trimester is most vulnerable?
- are there subtle later effects on attention, learning, mood, sleep, metabolism?
- how much risk is CBD vs THC/contaminants?
Potential risks for the baby and pregnancy
Placental transfer and immature metabolism
Cannabinoids can cross the placenta. The fetus also has immature metabolism and clearance, so exposure may last longer than in an adult.
Neurodevelopment concerns
Fetal brain development relies on precisely timed signals. If effects occur, they may be subtle and noticed later (sleep regulation, behaviour, learning). This uncertainty drives cautious advice around CBD pregnancy.
Pregnancy outcomes
CBD-specific outcome data are limited. Broader cannabis studies (often THC-related) sometimes show associations with low birth weight and preterm birth, though confounding factors exist. Because CBD products may contain THC despite labels, clinicians often take a precautionary approach.
What clinicians may monitor
If cannabinoid exposure is known or suspected, teams may watch:
- fetal growth and birth measurements
- feeding and weight gain
- alertness, tone, settling
CBD pregnancy by trimester (why timing matters)
First trimester
Organ formation and early placental development occur here, with ECS involvement in early signalling. Exposure carries higher uncertainty.
Second trimester
Growth accelerates, the placenta matures, and brain pathways develop.
Third trimester
Brain maturation and metabolic programming continue. Fetal exposure is still possible even near term.
Side effects and health issues for the pregnant person
CBD may cause:
- drowsiness, fatigue, dizziness
- gastrointestinal symptoms (nausea, diarrhoea, abdominal discomfort)
- appetite changes
- blood pressure drop and faintness (falls are a real concern)
CBD has also been associated with liver enzyme elevation in some settings, especially at higher doses or with interacting medicines.
Extra caution is often used with growth restriction risk, preeclampsia/placental issues, threatened preterm labour, or liver disease.
Interactions with medicines and supplements
CBD can affect liver metabolism pathways (including CYP enzymes), which may alter levels of other medicines.
This can matter for anti-nausea medicines, antidepressants, anxiety medicines, anti-epileptics, and pain medicines. If you take regular medicines, CBD pregnancy decisions should involve a pharmacist or doctor.
Product types and exposure: why route matters
- Oral oils/capsules/gummies: higher systemic exposure, variable absorption, often the most discouraged route in pregnancy.
- Sublingual oils: faster onset but dosing is imprecise.
- Edibles: delayed onset can lead to unintentional re-dosing.
- Vaping/inhalation: rapid systemic exposure plus respiratory risks from heating products.
- Topicals: may still absorb, skin irritation and added fragrances are common issues.
Dose in CBD pregnancy: why “safe dose” isn’t established
Absorption varies by route, food intake, formulation, and individual metabolism. Product labels may be inaccurate, and batch-to-batch variability is common.
“Microdosing” is popular online, but there is no solid evidence that microdosing CBD is safe or effective in CBD pregnancy.
THC contamination and other quality risks
Hidden THC
THC contamination can happen even in CBD-labelled products. This matters medically (THC is discouraged in pregnancy) and practically (THC metabolites can trigger a positive drug test).
Contaminants
Possible contaminants include pesticides, heavy metals, residual solvents, microbes, and additives.
COA (certificate of analysis)
A batch-specific COA may show CBD/THC amounts and contaminant screening. It can be useful, but only if it truly matches the batch and the lab is reliable.
Safer alternatives for symptoms people hope CBD will help
Nausea and vomiting
Try small frequent meals, dry foods on waking, and frequent sips of fluid. Acupressure wristbands (P6 point) may help.
Seek care if you cannot keep fluids down, there is weight loss, or dehydration signs appear—hyperemesis gravidarum is treatable.
Anxiety and stress
Breathing exercises, progressive muscle relaxation, guided meditation, and perinatal mental health support have clearer pregnancy safety profiles.
Sleep
Work on timing, a cool dark room, screen limits, reflux management, and pregnancy pillow support. Persistent insomnia may need assessment for reflux, restless legs, or anxiety.
Pain
Gentle activity (walking), pregnancy-adapted swimming, physiotherapy, posture strategies, and heat in moderation can help. Seek urgent advice for sudden severe pain, fever, visual symptoms, bleeding, high blood pressure, or reduced fetal movement.
Medical guidance: how to decide safely
Clinicians often advise avoiding cannabinoids in CBD pregnancy because human safety data are limited, preclinical concerns exist, products may contain THC/contaminants, and medicine interactions are possible.
If you want to discuss it, bring specifics (product form, estimated dose, frequency, any COA) and ask:
- Could it contain THC despite the label?
- Could it interact with my medicines?
- What options have better pregnancy safety evidence for my symptom?
If you used CBD before you knew you were pregnant
Note the product, form, dates, approximate dose and frequency, and whether it was full-spectrum/broad-spectrum/isolate. Inform your prenatal provider, especially if it was first trimester or full-spectrum. Often the plan is to stop exposure and continue routine care, with added monitoring only if indicated.
CBD and breastfeeding
Cannabinoids can pass into breast milk. CBD-specific infant safety data are limited, and contamination is a concern, so many clinicians advise avoiding CBD while breastfeeding.
Key takeaways
- CBD pregnancy safety evidence in humans is limited, a precautionary approach is common.
- Cannabinoids can cross the placenta, and fetal metabolism is immature.
- THC exposure is discouraged, and CBD products may still contain THC.
- Contaminants (pesticides, solvents, heavy metals, microbes, additives) are a real quality issue.
- CBD can cause drowsiness, GI symptoms, blood pressure drops, and medicine interactions.
- For nausea, anxiety, sleep issues, and pain, discuss options with clearer pregnancy safety profiles with your maternity team.
- Breastfeeding also calls for caution.
- Support exists: speak with your doctor, midwife, or pharmacist, and you can download the Heloa app for personalised guidance and free child health questionnaires.
Questions Parents Ask
Is topical CBD (creams/balms) safe during pregnancy?
It’s a very common question—especially for back or pelvic pain. Even though topicals may lead to less whole-body exposure than oils or gummies, absorption isn’t zero and products can be mislabeled or contain added ingredients that irritate sensitive pregnancy skin. For peace of mind, many clinicians prefer options with clearer pregnancy safety data (physio, heat in moderation, pregnancy-safe massage). If you’re considering a topical, you can share the ingredient list and any COA with your pharmacist or maternity team.
Can CBD interact with prenatal vitamins, iron, or common pregnancy medicines?
Sometimes, yes. CBD can influence liver enzymes that help process medicines, which may change how some treatments work (for nausea, anxiety, epilepsy, pain, or sleep). Prenatal vitamins alone are less of a concern, but many parents take several products at once (iron, thyroid meds, anti-nausea tablets). If you’re using—or thinking about using—CBD, it’s completely normal to want a quick safety check: a pharmacist can review your full list and flag interaction risks.
I used CBD before I knew I was pregnant—what now?
No panic—you’re not alone. Many parents only find out weeks into pregnancy. The most helpful next step is to write down what you took (brand, form, approximate dose, dates, and whether it was full-spectrum) and mention it at your next appointment. In most situations, the plan is simply to stop exposure and continue routine prenatal care, with extra monitoring only if your clinician feels it’s needed.

Further reading :
- What You Should Know About Using CBD When Pregnant …: https://www.fda.gov/consumers/consumer-updates/what-you-should-know-about-using-cannabis-including-cbd-when-pregnant-or-breastfeeding
- Factors associated with ever using cannabidiol in a cohort …: https://pmc.ncbi.nlm.nih.gov/articles/PMC9992243/
- Fetal cannabidiol (CBD) exposure alters thermal pain …: https://www.nature.com/articles/s41380-023-02130-y