The journey into parenthood often arrives with a wave of joy—sometimes intense, sometimes quiet, sometimes mixed with a disorienting rush of physical and emotional changes. Many parents, in those first fragile days, wonder why euphoria might trip into sudden tears, or where the sudden fatigue, sweats, or sense of overwhelm comes from. If you hesitate over strange new emotional tides or lingering aches as you cradle your baby, you are far from alone. Postpartum hormones orchestrate near-constant internal adjustments: molecular changes affecting everything from sleep, mood, skin, and hair, right through to powerful shifts in how you bond with your newborn. So what does the body actually endure, and how do these chemical messengers shape not just new life, but the parent adapting to it? Let’s untangle what’s happening, what’s normal, and what support is possible along the way.
Understanding Postpartum Hormonal Changes
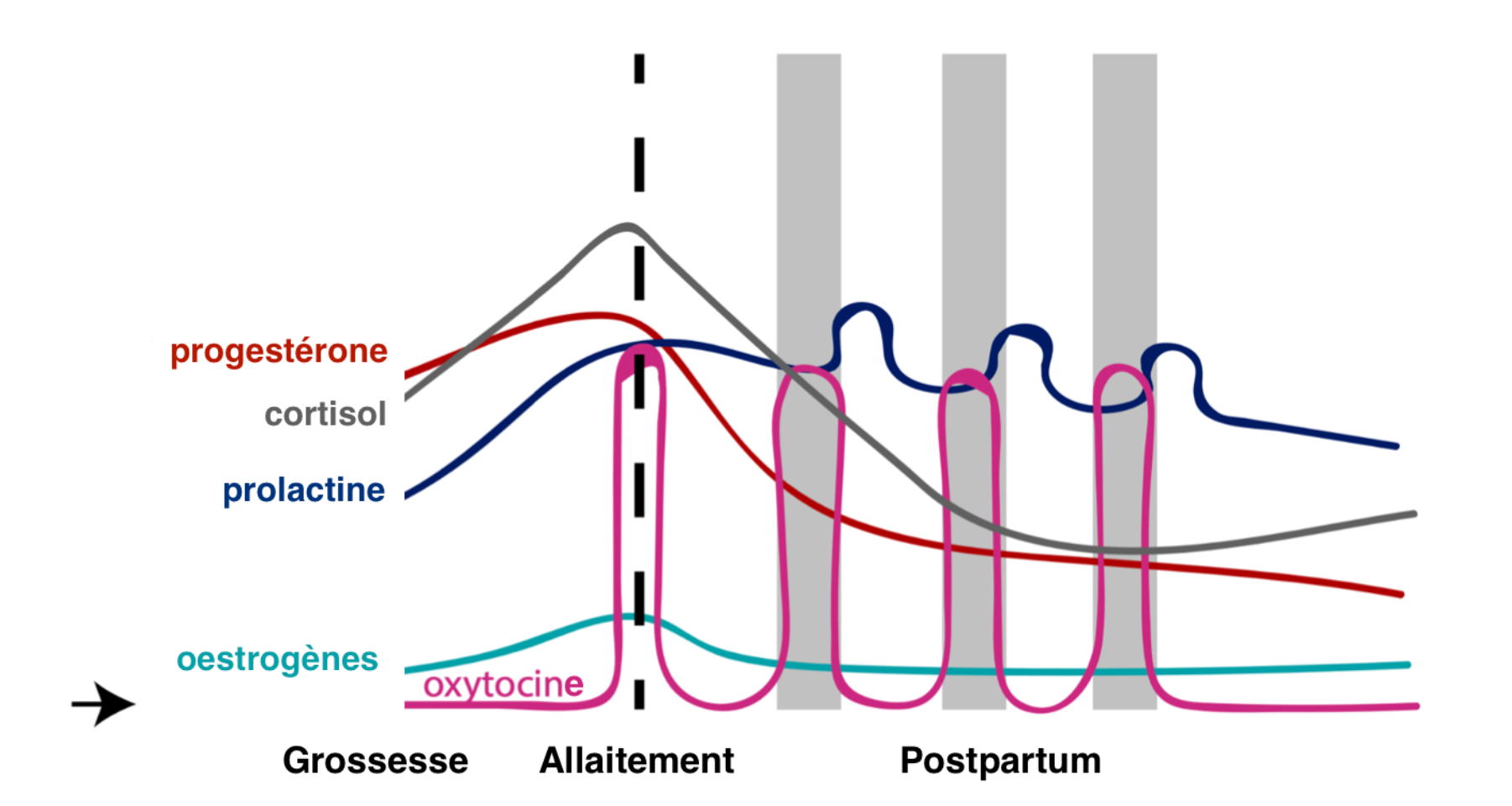
The drama of delivery marks only the beginning of change. During pregnancy, hormones such as estrogen, progesterone, and a complex array of placental hormones reach astonishing heights—levels that dramatically drop just hours after the placenta is delivered. Imagine descending from a hormonal summit: this sharp plunge triggers a cascade of recovery signals throughout the body. You might notice the sudden shift; you might just feel “off.” While these postpartum hormones start returning systems to baseline—tightening the uterus, activating milk glands, regulating mood—they also, paradoxically, create temporary chaos. Some parents describe it as feeling like a new version of themselves, emotionally raw and physically alert.
Cognitive changes may become apparent, even in the language used to describe each day: one moment, clear-headed and focused on your baby; the next, lost in distraction or anxiety. Why? Estrogen and progesterone—once protective to the brain and mood—fall so dramatically that neurotransmitters struggle to keep up. Beneath the surface, other chemicals like oxytocin, prolactin, and cortisol take the stage. Each has its own rhythm, each adds another thread to the emotional and physiological tapestry of early parenthood.
The Rapid Drop
The physical mechanism is striking in its simplicity: with the placenta gone, the supply of estrogen and progesterone collapses almost overnight. This chemical withdrawal contributes to what’s commonly known as the “baby blues” (mood swings, weepiness, spurts of irritability). For most, these surges fade within two weeks as receptors adjust. But for others, the lingering effects may deepen into postpartum depression—less a sign of weakness, more a consequence of these potent hormonal imbalances.
What’s happening behind the scenes? Estrogen governs mood, cognition, even sexual function; progesterone quells anxiety, provides calm, and, through its metabolite allopregnanolone, directly soothes the brain’s stress pathways. Their withdrawal is a physiological jolt. Yet, in contrast, prolactin—rising rapidly—offers tranquil moments, encouraging nurturing and promoting milk production. Fatigue is heightened by surging cortisol, which may remain high from both labor and ongoing stress. The tempo of hormonal transformation explains why parents can swing from elation to exhaustion, sometimes within a single hour.
Key Hormones After Pregnancy
Estrogen and Progesterone: Both vanish rapidly after childbirth. Their absence can trigger hot flashes, vaginal dryness, mood lability, and sometimes a dimmed libido. During pregnancy, estrogen is at its zenith; afterwards, its sudden retreat removes the support structures for mood and emotions.
Progesterone loss means less allopregnanolone in the brain—a neuroactive steroid with profound calming effects—leaving some parents more vulnerable to symptoms like anxiety or insomnia.
Prolactin: This hormone, crucial for milk synthesis, rises with every feed. It not only fuels lactation but can bring a surprisingly calming, even sedative effect, helping manage the stress of round-the-clock newborn care. Research also draws a link between prolactin drops and postpartum depression symptoms.
Oxytocin: Sometimes termed the bonding hormone, oxytocin surges with contractions, peaks during skin-to-skin, and ensures let-down during breastfeeding. But its influence is larger: it primes the nervous system for social contact, deepening emotional attachment, and even moderating stress. Lower oxytocin has been associated with depressive symptoms, suggesting its central role in postnatal wellbeing.
Cortisol: High in the postpartum phase, cortisol is intended to mobilize energy and readiness. Persistent elevation, however, may fuel sleep disruption or emotional upheaval—a biological tug-of-war between recovery and survival.
Thyroid Hormones: Up to 10% of parents experience thyroid changes (postpartum thyroiditis) that can mimic depression or anxiety, causing profound fatigue, mood oscillations, or sudden weight changes.
Placental Hormones (hCG, relaxin, hPL): With delivery, these hormones collapse, setting in motion uterine recovery and, eventually, a return to ovulation.
The Science of Hormonal Fluctuation
The sharpest collapse occurs within the first 48 hours. Estrogen and progesterone are the first to plummet, shadowed by the rise of oxytocin and prolactin—especially potent for breastfeeding parents. Those bottle feeding typically see a faster return to ovulatory cycles, while ongoing breastfeeding delays the reappearance of periods due to sustained prolactin dominance.
A fascinating detail: elevated cortisol in the early postpartum acts as a buffer, supporting survival and adaptation, but at a cost if prolonged. Thyroid irregularities, emerging weeks or even months after delivery, can further tangle symptom patterns—dry skin, lethargy, erratic weight—sometimes misread as “just motherhood.” Recognizing when these symptoms flag a deeper issue allows for intervention and individualized support.
Breastfeeding, Hormones, and Bonding: A Close Look
The interplay of prolactin and oxytocin is a marvel: one promotes milk, the other delivers it and deepens parent-infant bonds. Soothing stress, fueling connection, and even lowering heart rate, these postpartum hormones create an environment attuned to baby’s needs. Interestingly, partners—regardless of birth experience—show rising levels of oxytocin and even prolactin, fostering attachment and caregiving (albeit on a different timeline).
Bonding is not a one-size-fits-all process. Some feel elated instantly; others find connection grows slowly. No hormone chart can script the perfectly smooth path—expect a spectrum, with science offering reassurance in the biology of attachment.
Timeline of Postpartum Hormonal Shifts
First 48 Hours
A hormonal maelstrom defines these earliest days: radiant surges of oxytocin yield both overwhelming love and fierce protectiveness; prolactin stimulates tight, sometimes uncomfortable breast engorgement; estrogen and progesterone crater, ushering in night sweats, unpredictable mood drops, dramatic fatigue, and tender afterpains. Tearfulness peaks as chemical signals recalibrate.
Weeks to Months: Gradual Stabilization
While emotional swings typically lift by the second week, physical symptoms (especially for breastfeeding parents) may linger. Menstrual cycles restart anywhere from 6 weeks to many months later, shaped primarily by prolactin‘s suppression of ovulation. By 3 to 6 months, most postpartum hormones approach pre-pregnancy levels, unless ongoing breastfeeding prolongs this unique endocrine environment.
Physical and Emotional Impact
Physical Symptoms
What changes might parents spot during hormonal upheaval?
- Hot flashes, chills, and night sweats arise as estrogen reversal scrambles body temperature controls.
- Hair loss peaks at three to four months—a normal redistribution as follicles exit pregnancy growth sync.
- Skin shifts—new dryness, sudden fading of pregnancy pigmentation, sometimes unexpected acne.
- Weight changes, driven by both hormone shifts and new routines.
- Breast fullness and engorgement as prolactin and oxytocin rev up lactation.
- Vaginal dryness and low libido, tied to reduced estrogen, especially in those still feeding at the breast.
Emotional and Psychological Symptoms
Why so much emotional turbulence? Neuroscience explains: as estrogen and progesterone disappear, mood-regulating neurotransmitters can become less responsive, amplifying anxiety, irritability, or tearfulness. While about half of parents ride these waves (the ‘baby blues’), most recover quickly. Persistent sadness, rising anxiety, or difficulty bonding, however, can herald postpartum depression—a state driven as much by neurochemical change as by life transition.
Symptoms warranting attention:
- Lasting sadness or anhedonia (loss of interest in enjoyable things)
- Constant anxiety, inability to rest, persistent fatigue
- Appetite and sleep disruption
- Trouble engaging with or caring for baby
Medical help is essential if symptoms persist beyond two weeks or escalate—thoughts of self-harm or harm to baby always require urgent intervention.
When Hormones Go Awry: Postpartum Depression and Beyond
What precisely makes mood unstable for some and peaceful for others? The sharp descent of estrogen and progesterone, with erratic cortisol and possible thyroid shifts, affects neural circuits responsible for joy, motivation, and energy. One in four may experience postpartum depression, with anxiety and panic attacks also appearing. Recognizing symptoms—especially those suggesting thyroid dysfunction—can be transformative, as effective treatments exist.
Therapy might range from supportive counseling and antidepressants, to careful hormone or thyroid replacement (all tailored for breastfeeding if needed). Social support, rest, and practical help are not ‘nice to haves’, but form part of medical best practice.
Deep Dive: Hormones in Focus
- Estrogen and Progesterone: Both shape mood, sexual health, and physiological recovery. Loss often means temporary instability, improved by rest, nutrition, and medical care when needed.
- Prolactin and Oxytocin: Twin architects of milk and bonding; their sustained influence offers calm, supports maternal behaviors, and even underpins the neurobiology of love.
- Cortisol: Both shield and antagonist; it prepares the body for recovery, but when unchecked, exacerbates fatigue and distress. Gentle exercise, mindfulness, and connection can help modulate its effect.
- Thyroid Hormones: Too high or too low, these govern energy, metabolism, and emotional tone. Blood tests, not guesswork, determine underlying issues and direct optimal care.
- Placental hormones, hCG, relaxin: Fallen to background, their withdrawal signals the end of pregnancy and the gradual restoration of ovulatory rhythms.
Nutrition and Lifestyle: Supporting Hormonal Resilience
What practical steps help harmonize postpartum hormones?
- Embrace nutrient-rich foods: Iron, lean protein, omega-3 fatty acids, whole grains, and an abundance of vegetables fortify both recovery and mental clarity.
- Targeted micronutrients—vitamin D and magnesium—underpin mood, immunity, and restful sleep.
- Hydration is not an afterthought; breastmilk itself is more than 80% water.
- Rest, even brief naps, accelerates healing.
- Gentle movement—walking, postnatal yoga, stretching—restores strength and lifts spirits.
- Stress management strategies (breathing exercises, journaling, meaningful conversation) build emotional tools for coping.
- Lean on support networks—whether through a partner, relatives, friends, or parent groups. Asking for help is not weakness.
Medical Care and Professional Support
If symptoms persist or physical discomfort interferes with daily life (persistent fatigue, severe anxiety, unmanageable mood swings), seeking medical input ensures safe and effective intervention. Medical treatment may involve counseling, antidepressants, regulated hormone or thyroid therapy, and nutritionally-targeted supplements (multivitamins, omega-3s, iron, vitamin D). Complementary care—aromatherapy, gentle massage—can provide comfort, but should enhance, not replace, professional healthcare.
When Symptoms Persist: Long-Term Hormonal Changes
Some parents find certain postpartum hormones remain imbalanced for months—occasionally over a year. Recurrent issues (pervasive fatigue, hair loss, erratic cycles, persistent mood changes) require careful evaluation. Sometimes underlying thyroid disorders or even early signs of perimenopause explain “stuck” symptoms. Management may include endocrinological assessment, targeted hormone therapy, more focused nutritional strategies, and psychological support. The earlier these markers are recognized, the quicker recovery and restoration of well-being.
Key Takeaways
- Postpartum hormones drive a dramatic and rapid recalibration after birth, influencing mood, energy, sleep, bonding, and physical recovery.
- Key players—estrogen, progesterone, prolactin, oxytocin, cortisol, and thyroid hormones—work in harmony and disarray, explaining emotional and bodily shifts.
- The “baby blues” typically fade within 14 days, but lingering symptoms (sadness, exhaustion, anxiety, struggles to connect) raise the flag for professional input.
- Physical symptoms—ranging from night sweats and hair loss to vaginal dryness and fluctuating appetite—reflect underlying hormonal transitions.
- Nutrition, rest, hydration, gentle exercise, and mindful stress-reduction strategies all foster better hormonal balance and smoother recovery.
- Medical assessment for prolonged fatigue, strong mood changes, reproductive changes, or suspected thyroid imbalance is paramount for ongoing health.
- A broad spectrum of support exists—from healthcare providers to peer groups—encouraging personalized, effective recovery.
- Download the Heloa app for tailored parenting advice and free health questionnaires for your child. Personalized guidance is only a few taps away.
Questions Parents Ask
How long does it take for postpartum hormones to balance?
Hormonal fluctuations after childbirth are part of the recovery process. For many, hormone levels begin to stabilize gradually over three to four months. That said, the pace can differ for each person. Some parents notice emotional or physical shifts balancing sooner, while others may feel ongoing changes for a longer period. Rassurez-vous, if you continue to feel “not yourself” after a few months, talking with a healthcare professional can offer clarity and support.
What are the signs of hormone imbalance months after delivery?
Sometimes, hormone levels can remain unsteady even after the first several months. Persistent mood swings, fatigue, sleep difficulties, changes in appetite, or feelings of anxiety and sadness can signal that hormonal adjustment is still ongoing. Some parents also notice physical signs, such as hair loss or changes in weight. If these symptoms linger or interfere with your daily well-being, n’hésitez pas à consulter un professionnel de santé pour un accompagnement adapté.
Can postpartum hormones affect sleep even if the baby sleeps well?
Absolutely. Even when your baby enjoys restful nights, hormonal shifts—especially following the drop in estrogen and progesterone—can influence your sleep quality. Some parents experience trouble falling asleep, early waking, or vivid dreams during the first weeks or months after birth. With time, as hormone levels even out and daily rhythms settle, sleep often improves. En attendant, prenez soin de vous et cherchez du soutien si le manque de sommeil devient difficile à supporter.