Food poisoning during pregnancy can make anyone pause mid-bite: was that street pani puri washed properly, did the milk boil enough, did the fridge stay cold through the power cut? Most episodes are short and settle within a couple of days, and the main goal is simple – keep yourself hydrated. Still, a few infections (especially listeriosis and toxoplasmosis) need extra attention because they can cross the placenta.
Knowing what to look out for, how quickly symptoms can start, and which foods commonly cause trouble in Indian kitchens and eateries helps you act fast – without turning every meal into a worry.
What food poisoning means in pregnancy
Food poisoning during pregnancy is a foodborne illness caused by eating or drinking something contaminated with:
- Bacteria (for example Salmonella, Campylobacter, Listeria monocytogenes)
- Viruses (often norovirus)
- Parasites (notably Toxoplasma gondii)
- Toxins (uncommon, botulism from improperly processed foods, or histamine fish poisoning from poorly stored fish)
Most of the time it looks like acute gastroenteritis: nausea, vomiting, diarrhoea, crampy abdominal pain, and sometimes fever. Medically, the gut lining becomes inflamed and leaky, so fluid and salts (electrolytes like sodium and potassium) move out of the body faster than usual.
Why pregnancy can make foodborne illness more concerning
Pregnancy involves normal immune adjustments that support the growing baby. This does not mean you are weak. It does mean that in food poisoning during pregnancy:
- Fluid losses from vomiting and diarrhoea can feel harsher and become significant sooner.
- Some germs can enter the bloodstream (bacteraemia) and potentially reach the placenta.
And yes, it can happen after everyday scenarios: a family function meal, catered food sitting out, a salad kept too long, curd rice left at room temperature, or cross-contamination (cutting raw chicken and then slicing cucumber with the same knife – easy to miss in a busy kitchen).
Food poisoning vs stomach flu (viral gastroenteritis)
The symptoms overlap: vomiting, loose motions, cramps, sometimes fever.
Clues suggesting food poisoning during pregnancy include a clear exposure – leftovers that tasted off, undercooked meat, eggs that were runny, food from a place where hygiene looked doubtful. Viral gastroenteritis (often norovirus) spreads very easily person-to-person and through surfaces, so several people at home or in the office may fall sick around the same time.
At home, the priority is not perfect labelling. The priority is early red-flag spotting and protecting hydration.
Common causes of food poisoning during pregnancy
The two infections to know well: listeriosis and toxoplasmosis
Listeria monocytogenes (listeriosis)
Listeria is monitored closely because it can cross the placenta and be severe for the baby even when the pregnant person has mild symptoms. It is often linked to refrigerated ready-to-eat foods.
In an Indian context, think beyond deli meat: risk can rise with foods kept refrigerated for many days and eaten without reheating.
Higher-risk examples include:
- Soft cheeses made from unpasteurised milk
- Ready-to-eat refrigerated foods kept for long periods
- Cold smoked fish
Symptoms may resemble a mild flu – fever, body ache, fatigue – sometimes without diarrhoea.
Toxoplasma gondii (toxoplasmosis)
Toxoplasma is a parasite typically acquired from undercooked meat and foods contaminated with soil (unwashed fruits and vegetables). Many maternal infections cause few or no symptoms.
Common exposure routes:
- Undercooked mutton, pork, or other meats
- Unwashed salad leaves, coriander, fruits, and vegetables with soil residue
- Handling cat litter (less common than food, but still discussed)
Common “stomach infection” causes: bacteria and viruses
Salmonella
Often linked to undercooked eggs, poultry, and egg-based preparations, plus cross-contamination.
Campylobacter
Often linked to undercooked poultry and unpasteurised milk.
Pathogenic E. coli (including STEC/EHEC)
Often linked to undercooked minced meat and unpasteurised dairy. Bloody diarrhoea is a warning sign.
Norovirus
Very contagious and often spreads person-to-person, it can also be food-related. In pregnancy, the main risk is dehydration.
Toxins: rare, but important to recognise
- Botulism (exceptional): can cause blurred vision, drooping eyelids, difficulty swallowing, weakness
- Histamine fish poisoning: flushing, headache, palpitations soon after eating poorly stored fish
- Mycotoxins: exposure through mouldy foods, concern is more about repeated exposure
Symptoms to watch for during pregnancy
Digestive symptoms
In food poisoning during pregnancy, the most common symptoms are:
- Nausea and vomiting
- Diarrhoea (sometimes very watery and frequent)
- Abdominal pain and cramps
- Bloating, weakness, fatigue
Some people feel mildly uncomfortable. Others feel completely drained. Both deserve attention.
Fever and dehydration: the two key concerns
Fever may come with chills, body aches, and headache. Watch closely for dehydration:
- Strong thirst, dry mouth
- Dark urine or urinating much less than usual
- Dizziness or feeling faint
- Marked tiredness, weakness
Fever plus poor fluid intake is a common reason for same-day medical advice in pregnancy.
Few symptoms can still matter
Some infections can be subtle:
- Listeriosis may look like mild flu, sometimes without diarrhoea
- Toxoplasmosis is often asymptomatic
An unexplained fever during pregnancy deserves a call, even if the tummy symptoms are not dramatic.
Timing: incubation and expected course
Quick onset: hours to 48 hours
Many episodes begin within a few hours after a meal, or within 24-48 hours.
Longer incubation: listeriosis and toxoplasmosis
- Listeriosis can incubate for a long time – sometimes up to 8 weeks.
- Toxoplasmosis timing varies, it is often picked up through blood tests rather than obvious symptoms.
Typical duration and signs it is not settling
Most episodes improve within 1-3 days. Medical advice is especially useful if you have:
- Persistent fever
- Severe or prolonged diarrhoea
- Blood in stool
- Inability to drink enough
Dehydration during pregnancy: why it matters
Vomiting and diarrhoea cause loss of water and electrolytes. In pregnancy, dehydration can contribute to dizziness, weakness, and uterine irritability (tightening that can feel like contractions). If significant, dehydration may reduce uteroplacental blood flow.
Seek urgent care if you cannot keep fluids down, your urine output drops significantly, you feel faint, or symptoms are paired with fever.
Risks and complications for parent and baby
For the pregnant person
The most immediate risk in food poisoning during pregnancy is dehydration, sometimes with electrolyte imbalance. High fever is exhausting and may trigger contractions. More rarely, some bacteria can invade beyond the gut.
For the baby
Risk depends on the germ:
- Listeria and toxoplasma can infect the fetus.
- Severe dehydration can reduce uteroplacental perfusion.
Miscarriage and preterm birth: when risk increases
Risk increases especially with:
- Persistent fever
- Suspected invasive infection (including suspected listeriosis)
- Uncontrolled vomiting or very heavy diarrhoea without adequate rehydration
How trimester can shift the focus
- First trimester: high fevers deserve careful attention, primary toxoplasma infection can be more concerning for fetal development.
- Second trimester: dehydration may trigger contractions, fetal infection risk depends on the pathogen.
- Third trimester: higher preterm labour risk when contractions occur with significant illness.
When to contact a healthcare professional urgently
If you are thinking, “Should I wait or call?”, these are practical thresholds in food poisoning during pregnancy:
- Fever ≥ 38°C or fever that persists
- Inability to keep liquids down
- Very frequent watery diarrhoea, or diarrhoea lasting more than 48-72 hours
- Blood in stool
- Signs of dehydration (very dark urine, urinating much less, dizziness, weakness, faintness)
- Severe abdominal pain
- Contractions, vaginal bleeding, or fluid leakage
- Neurological symptoms (confusion, stiff neck, visual changes, seizures)
- Reduced fetal movement (especially later in pregnancy)
Medical evaluation and tests you may be offered
What your clinician will ask
Expect questions about:
- When symptoms started and how severe they are
- Maximum temperature
- Foods eaten (unpasteurised dairy, leftovers, refrigerated ready-to-eat foods, raw eggs)
- Anyone around you who is sick
- Ability to drink and urinate
- Pregnancy symptoms (contractions, pelvic pain, bleeding, fluid leakage, fetal movement)
Possible tests
Depending on severity, your clinician may suggest:
- Blood tests (complete blood count, electrolytes, kidney function)
- Stool tests when diarrhoea is feverish, bloody, or persistent
- Blood cultures if fever is high, chills are present, or listeriosis is suspected
If listeriosis is suspected
Fever plus a relevant food exposure may lead to prompt assessment, blood cultures, and sometimes antibiotics.
If toxoplasmosis is suspected
Diagnosis relies on blood tests (antibodies and interpretation tests). Depending on gestational age and results, targeted ultrasound and specialist review may be offered.
When fetal monitoring may be suggested
Later in pregnancy, or when illness is significant, your care team may advise fetal monitoring and contraction assessment.
Treatment options in pregnancy
At home when it is safe: rest and rehydration
If you feel generally stable and there are no red flags:
- Rest
- Take frequent small sips of water, coconut water, thin dal water, clear soups
- Use oral rehydration solution (ORS) if diarrhoea is watery or vomiting is repeated
A useful check: are you passing urine at reasonable intervals and able to keep fluids down? If not, call.
Symptom relief (with caution)
- Fever and pain: paracetamol can be used as per recommended dosing
- Nausea and vomiting: antiemetics may be considered with medical advice
- Diarrhoea: avoid self-medicating if there is fever or blood in stool
Antibiotics: only in selected situations
Most episodes do not need antibiotics. They may be discussed when:
- Invasive infection is suspected
- Fever is high and persistent
- A specific pathogen needs treatment (notably listeriosis)
Hospital care: when it may be needed
Hospital care may be considered for:
- Dehydration needing IV fluids
- High fever with worsening overall condition
- Maternal-fetal concerns needing monitoring
Higher-risk foods in pregnancy and safer choices (Indian context)
Unpasteurised dairy
Avoid raw milk and products made from unpasteurised milk. Prefer pasteurised milk, boil milk if you are not sure.
Ready-to-eat refrigerated foods and undercooked meat
Avoid foods kept in the fridge for many days and eaten without reheating. Avoid raw or undercooked meat dishes.
Raw fish, chilled smoked fish, and raw seafood
Avoid sushi with raw fish, chilled smoked fish, and raw shellfish.
Raw or undercooked eggs
Avoid runny eggs, homemade mayonnaise, mousse, and raw batter.
Unwashed produce and raw sprouts
Wash fruits and vegetables carefully. Avoid raw sprouts.
Storage and leftovers (very relevant in hot weather)
Cool cooked food quickly, refrigerate promptly, and reheat until steaming hot. If there was a long power cut and the fridge warmed up, be extra cautious with dairy and cooked foods.
Prevention in everyday life
Kitchen hygiene
- Wash hands with soap and water for 20 seconds
- Clean counters and cutting boards
- Keep raw and cooked foods separate
Cooking and reheating
Cook foods thoroughly, reheat leftovers fully, cook eggs till whites and yolks are firm.
Cold chain habits
- Keep the fridge at 4°C or below
- Store raw meat/fish at the bottom shelf in a closed container
- Minimise time food sits at room temperature, especially in summer
Eating outside: street food, buffets, and takeout
Prefer hot, freshly cooked items. Avoid lukewarm buffets, salads sitting out, raw chutneys of uncertain water quality, and desserts made with raw eggs. For takeout, bring it home quickly and refrigerate promptly.
If symptoms start
- Vomiting: small frequent sips, seek advice if you cannot drink
- Diarrhoea: ORS and fluids, seek advice if fever, blood, or very frequent stools
- Fever: paracetamol can help, but contact a clinician during pregnancy
- Contractions/pelvic pain: obstetric assessment is appropriate
Recovery and follow-up after an episode
Gradual return to food
Start gently: rice kanji, plain khichdi, bananas, toast, soups. Then return to well-cooked proteins and cooked vegetables. Avoid greasy, spicy foods for a few days.
What to monitor over the next days
Urine output, fever settling, stool frequency, and energy levels. Contact your clinician again if symptoms worsen.
Helpful details to share if you call
When symptoms started, number of vomiting episodes and stools, highest temperature, ability to drink, foods eaten, whether others are sick, medicines taken, and any pregnancy symptoms.
After recovery: what it usually means for pregnancy
Most of the time, if the illness is brief and hydration is maintained, pregnancy continues normally. If fever was significant, listeriosis or toxoplasmosis is suspected, or symptoms were severe, your care team may suggest targeted follow-up.
Key takeaways
- Food poisoning during pregnancy is often short-lived, but listeriosis and toxoplasmosis need extra attention because they can affect the placenta and fetus.
- The biggest risks are dehydration and fever.
- Incubation can be hours to weeks, listeriosis may incubate up to 8 weeks.
- Seek urgent care for fever ≥ 38°C, inability to drink, blood in stool, severe pain, contractions, bleeding, fluid leakage, neurological symptoms, or reduced fetal movement.
- Prevention relies on pasteurised dairy, thorough cooking, safe leftovers, clean hands and surfaces, and maintaining the cold chain.
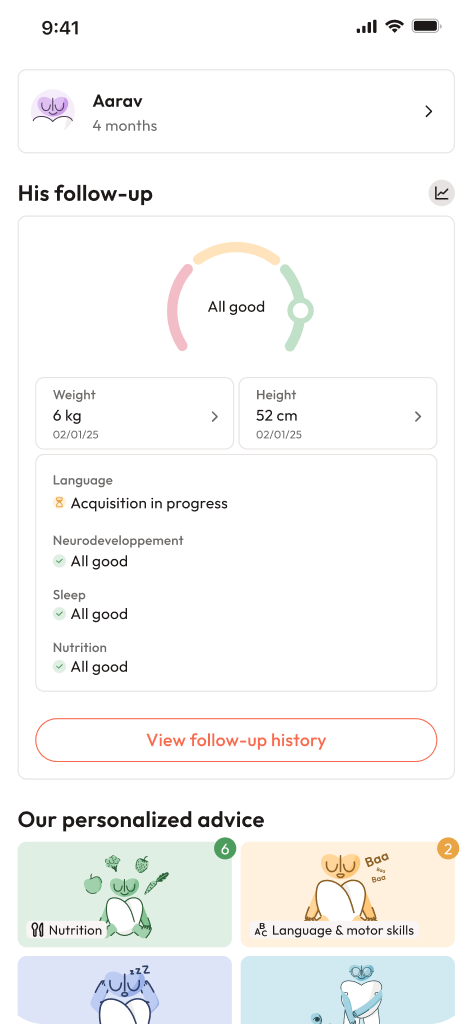
- Support exists: your obstetrician, local clinic, and maternity hospital can guide you. You can also download the Heloa app for personalised advice and free child health questionnaires.

Further reading: