Pregnancy can feel like a full-body adjustment—sometimes smooth, sometimes achy, often both in the same day. If you are noticing pain during pregnancy, it is not a sign of weakness and it is not a “bad pregnancy”. Joints, muscles, digestion, circulation, and pelvic tissues are all adapting at speed.
What matters is pattern and context. Is the discomfort mild and settling with rest? Or is it severe, persistent, and paired with other symptoms? With a few clear cues, pain during pregnancy becomes less scary and more manageable.
Pain during pregnancy: what’s common and why it happens
Normal body changes vs pain that deserves extra attention
Many types of pain during pregnancy are mild to moderate, come and go, and ease with rest, hydration, gentle movement, or a position change. Common examples:
- pulling as the belly grows
- brief groin “stabs” when turning in bed
- lower back ache after standing or cooking
- short cramps after orgasm that settle with rest
Pain deserves extra attention when it is severe, constant, rapidly worsening, or paired with fever, fainting, breathlessness, bleeding, or fluid leakage. Also watch for pain that is regular and rhythmic—this can fit contractions rather than everyday discomfort.
Why pregnancy can change pain (hormones, relaxin, posture, circulation)
Several normal changes make pain during pregnancy more likely:
- Progesterone and relaxin loosen ligaments and joints. Helpful for birth preparation, but pelvic joints may feel unstable.
- Pelvic tissues become more vascular. Increased blood flow can make the vulva, vagina, and cervix more sensitive to touch or friction.
- As the uterus grows, your centre of gravity shifts forward and the lower back curve increases, loading lumbar muscles.
- Blood volume rises markedly (often quoted as ~40–50% more plasma by mid-pregnancy), supporting the placenta but also promoting leg swelling.
- The uterus can compress pelvic veins and the inferior vena cava, contributing to swelling, haemorrhoids, and dizziness when standing quickly.
Abdominal pain during pregnancy: common sensations and meanings
What abdominal pain can feel like
Abdominal pain during pregnancy is not one single feeling. Many parents describe:
- crampy, period-like aches low in the pelvis
- brief sharp pains with standing, twisting, coughing, or sneezing
- one-sided stabs lasting seconds to minutes
- tightening that comes and goes
Digestive causes are very common because gut motility slows. Gas, constipation, and reflux can create cramping or upper abdominal burning.
Faster medical advice is needed for severe pain that does not settle with rest, pain with fever, persistent one-sided pain, dizziness/fainting, or pain with bleeding/fluid leakage.
Stretching and uterine growth discomfort
As the uterus enlarges, the abdominal wall and supporting ligaments stretch. That stretching can cause pulling, tightness, or aching—often worse after activity or at the end of the day.
Mild cramps may also happen with dehydration, bladder fullness, or after orgasm. If tightening becomes regular, intensifies, or does not improve with rest and hydration, contractions should be ruled out.
Round ligament pain during pregnancy
Where it shows up and why it happens
Round ligament pain is a common, usually benign cause of quick stabbing discomfort. The round ligaments support the uterus, as the uterus grows and tilts, they stretch.
It is often felt:
- low in the abdomen
- in the groin
- near the hip crease
It typically appears with movement and fades quickly.
What helps day to day
- move slowly when rolling over, standing up, or getting out of the car
- support the belly when coughing or sneezing
- use warm compresses for short periods (avoid overheating)
Seek assessment if pain becomes constant, very severe, or comes with fever, vomiting, faintness, bleeding, fluid leakage, or regular contractions.
Leg cramps during pregnancy
What they feel like
Leg cramps often strike the calf, sometimes the foot or thigh. They can feel like a sudden knot that forces you to stop. Pain during pregnancy can be influenced by muscle fatigue, fluid shifts, venous stasis, and possible electrolyte imbalance.
Night cramps: relief and prevention
In the moment:
- straighten the leg and gently pull toes toward the shin (dorsiflexion)
- massage the calf, apply warm (not hot) heat
- walk briefly if you feel steady
To reduce recurrence:
- hydrate steadily through the day
- calf stretching before bed (20–30 seconds, 2–3 repetitions)
- moderate activity like walking or swimming
- include dietary sources of potassium, calcium, and magnesium, discuss supplements before starting
Important: if one leg is persistently swollen, warm, red, and painful—especially if stretching does not relieve it—seek urgent evaluation for a possible blood clot.
Back pain during pregnancy
Why it’s so frequent
Back pain is extremely common, especially in the second and third trimesters:
- forward shift of weight and increased lumbar curve
- stretched abdominal muscles giving less support
- ligament laxity around spine and pelvis
- gait changes and pelvic tilt
Small changes can help: supportive footwear, a lumbar cushion, frequent position changes, and side-sleeping with a pillow between the knees.
When to get assessed
Mild to moderate pain during pregnancy often improves with heat, gentle stretching, short walks, and posture support. Some parents find a maternity support belt helpful.
Get checked if back pain:
- wakes you repeatedly or prevents normal activity
- radiates with numbness, tingling, or weakness
- comes with fever or urinary symptoms
- occurs with regular tightening, bleeding, or fluid leakage
Pelvic, hip, vulvar, and nerve pain in pregnancy
Pelvic girdle pain (PGP/SPD)
Pelvic girdle pain comes from pelvic joints: the pubic symphysis (front) and/or sacroiliac joints (back). It can feel aching, stabbing, or grinding in the pubic area, groin, buttock, hips, or low back.
Often worse with:
- standing on one leg (stairs, dressing)
- getting in and out of bed or the car
- long walks or prolonged standing
- rolling over in bed
Physiotherapy with pregnancy experience is often very helpful. A pelvic support belt may reduce strain for some.
Vulvar heaviness and vulvar varicosities
Increased pelvic blood flow can make the vulva feel tender or heavy. Some people develop vulvar varicosities (vulvar varicose veins), causing heaviness or pressure, often worse after standing.
If you notice new bulging veins, increasing pressure, or worsening pain, mention it at your next visit.
Sciatica-like pain
Sciatica-like pain during pregnancy can shoot from buttock down the leg, sometimes with tingling.
Contact a clinician promptly if nerve pain comes with leg weakness, worsening numbness, walking difficulty, or bowel/bladder changes.
Pain during pregnancy by trimester
First trimester
Mild cramping can occur as the uterus starts changing. Nausea, headaches, and fatigue may also make the body feel sore.
Call promptly if there is severe or persistent one-sided pain, dizziness/fainting, or bleeding.
Second trimester
Stretching pains and round ligament pain often become more noticeable, along with low back ache.
If tightening becomes regular or painful, or if there is bleeding or fluid leakage, contact your maternity team.
Third trimester
Late pregnancy can feel heavy: swelling, calf cramps at night, pelvic pressure, vulvar heaviness, and sleep-related soreness are common.
New severe swelling with headache or vision changes needs assessment.
Pain by location: quick ways to describe what you feel
Lower abdomen vs groin/pelvis
Lower abdominal or suprapubic pain may relate to stretching, constipation, urinary infection, or contractions. Groin/pelvic pain more often fits round ligament pain or pelvic joint strain.
Track: exact spot, one side or both, trigger (standing, rolling, meals, urination, sex), duration, and whether rest helped.
Upper abdomen and right-sided rib/upper belly pain
Upper abdominal discomfort can be reflux or gas. Rib soreness can also happen later in pregnancy as posture changes and the uterus rises, baby’s kicks under the ribs can be sharp.
But persistent right upper quadrant pain should be discussed promptly, especially with nausea/vomiting, fever, severe headache, visual changes, or sudden swelling. Gallbladder disease is also more common in pregnancy.
Sex-related pain in pregnancy
Why it happens
Some people notice stinging with penetration, pelvic tightening, lower belly cramps, or pain after orgasm. Often linked to increased pelvic blood flow, lubrication changes, pelvic joint shifts, and pelvic floor tension.
If pain changes with position, depth, or pace, it often points to a mechanical factor you can adjust.
Safety basics
In many uncomplicated pregnancies, sex is usually possible. Still, pain during pregnancy is not something to push through. Slow down, change positions, use a water-based lubricant if dryness is present, or stop.
If your maternity team has advised restrictions (placenta previa, bleeding, threatened preterm labour, suspected rupture of membranes), follow that guidance.
Cramps after orgasm
Orgasm can trigger uterine contractions, often Braxton Hicks-type: irregular and settling with rest, hydration, and position change.
Before 37 weeks, tightening that becomes regular, painful, or does not settle after drinking and resting should prompt medical contact.
Causes to discuss with your clinician
Vaginal infections and urinary infections
Pregnancy can change vaginal balance and make infections more likely.
Consider assessment for:
- yeast infection: itching, burning, thick white discharge
- bacterial vaginosis: increased discharge, sometimes unusual odour
- urinary infection: burning urination, frequent urge, suprapubic pain, sometimes fever
Testing (urine test and/or vaginal swab) guides treatment.
Pelvic floor tension and pubic symphysis irritation
Pubic pain, pain when turning in bed, and difficulty walking can fit pelvic girdle pain. A tense pelvic floor can make the vaginal entrance painful.
A referral to pelvic health physiotherapy can make a real difference.
Red flags: when pain during pregnancy needs urgent care
Contact your maternity unit or seek urgent care if you have:
- vaginal bleeding with pain, or heavy bleeding
- fluid leakage (a gush or continuous trickle)
- fever or chills
- fainting, severe dizziness, or feeling clammy and unwell
- severe, persistent one-sided abdominal or pelvic pain
- regular painful contractions, especially before 37 weeks
- noticeably reduced fetal movement (especially after 28 weeks)
Also seek prompt evaluation for severe headache with vision changes, chest pain or breathlessness, or one leg that is swollen, warm, red, and painful (possible DVT).
Gentle pain relief options that are often used in pregnancy
Non-drug tools
For mild pain during pregnancy without red flags:
- rest and frequent position changes
- warm bath or heat pack on low for short periods (avoid overheating)
- cold pack for local inflammation
- gentle stretching and approved movement
- supportive shoes, lumbar cushion, pelvic/maternity belt if advised
- side-lying sleep with pillows between knees and under the belly
Medication considerations
Discuss medicines with your clinician. Paracetamol is commonly used when needed, at the lowest effective dose.
NSAIDs like ibuprofen or naproxen are generally avoided unless specifically advised.
Targeted self-care for common pregnancy pains
Leg cramps
- sip fluids through the day (especially in hot weather)
- calf stretch before bed (20–30 seconds, 2–3 repetitions)
- ankle circles/pumps in the evening
- calcium- and magnesium-rich foods, ask before supplementing
Back, pelvic, and round ligament pain
- stand tall, avoid locking knees
- log-roll in bed (shoulders and hips together)
- pillow between knees, another under belly
- reduce one-leg loading if pelvic pain flares
- consider physiotherapy for persistent pelvic or back pain
Pain during pregnancy vs labour pain
Braxton Hicks vs true labour
Braxton Hicks: irregular tightening that may ease with hydration, rest, or a position change.
True labour: contractions become regular, closer together, longer, stronger—and do not stop with rest.
If unsure, time them for an hour and call your maternity unit.
Preterm labour signs before 37 weeks
Before 37 weeks, contact your maternity unit promptly for regular contractions, pelvic pressure with recurring backache, or contractions with bleeding/fluid leakage.
Key takeaways
- Pain during pregnancy is often linked to hormones, ligament laxity, posture changes, increased pelvic blood flow, and expanded blood volume.
- Common patterns include abdominal stretching discomfort, back pain, leg cramps, pelvic girdle pain, and sex-related sensitivity.
- Severe, persistent, or worsening pain during pregnancy, or pain with bleeding, fluid leakage, fever, fainting, chest symptoms, a painful swollen leg, or reduced fetal movement needs urgent medical advice.
- Gentle measures—rest, warmth, stretching, supportive positioning, lubrication adjustments, and physiotherapy—can ease many everyday aches.
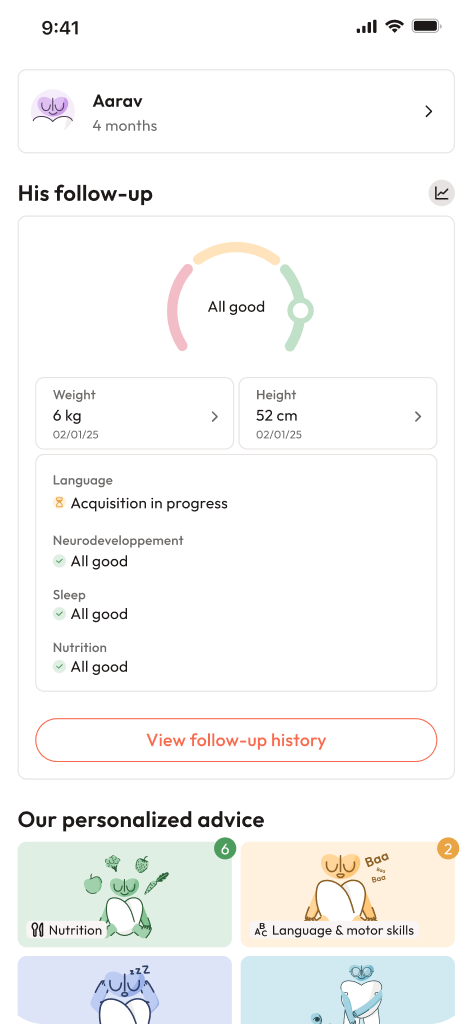
- If you need support, your obstetrician, midwife, and physiotherapist can guide you, you can also download the Heloa app for personalised advice and free child health questionnaires.

Further reading: