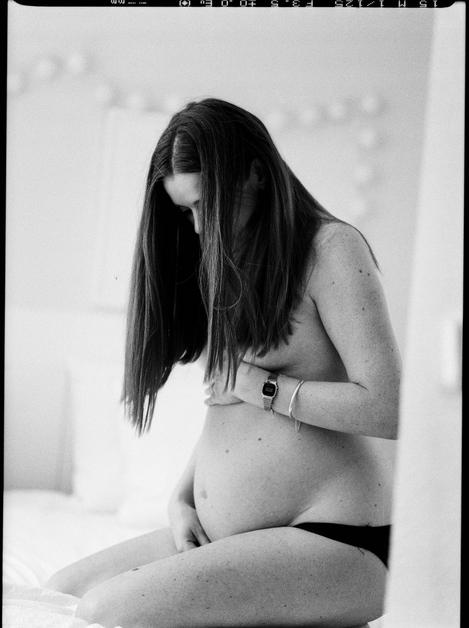
Picture this—one moment, fatigue and nausea hold court, the next, a surge of energy returns. The second trimester of pregnancy (weeks 14 to 27), often dubbed the “honeymoon period”, unravels a unique mixture of relief, anticipation and rapid transformation. For many, this phase is sprinkled with palpable changes—your belly now gently curves outward, once-elusive flutters are suddenly felt, and an ultrasound brings you face-to-face with a profile you’ve mostly imagined. Yet, lingering questions persist: What’s normal? How much movement is enough? Is this pain just ligaments stretching, or something more?
Expect a deep dive into the milestones of fetal development, maternal symptoms (the delightful, the expected, the occasionally baffling), routine clinical exams, nutrition, activity, common discomforts, and practical strategies to stay comfortable and confident. Health screening, safe medication practice, and special situations like twin pregnancies or health disorders—nothing is swept under the carpet. The goal is simple: empower, inform, and reassure, so you walk through this unique window of pregnancy with clarity and calm.
Weeks 14–16: Early changes, budding connections
Peek at the growing life within—a harmonious expansion. Limbs lengthen with surprising speed, fingers and toes, now accentuated by delicate nails, stretch gracefully. The facial features—imagine the nose, lips, and tiny eyelids—become more defined, setting the stage for late-night “who does baby resemble?” debates. Internally, key organs such as the heart (pumping with a regular four-chambered beat), kidneys (now making urine), and primitive respiratory muscles are hard at work, even if they’re not quite breathing yet.
Early on, sonography evolves from “crown–rump length” to concrete biometric metrics: biparietal diameter (BPD), head circumference (HC), femur length (FL), and abdominal circumference (AC). Your clinician interprets these not in isolation but as part of a dynamic chart, so one odd value? Not a cause for alarm.
What about how you feel? For many, nausea finally bows out, energy rebounds, and a gentle bump arises as the uterus escapes the pelvis. Breasts continue their transformation—fullness and perhaps a hint of colostrum. Some may notice nasal stuffiness, tender gums, or occasional heartburn; simple remedies like smaller meals and saline rinses can ease the way.
Weeks 17–20: Quickening – first kicks and mighty milestones
Curiosity peaks right here. You might catch a gentle flutter—a “quickening”—often described as bubbles, a faint flicker, or butterfly wings, typically between 18 and 20 weeks. Is it really the baby? Quite likely! Movement perception varies wildly, but most parents start tuning in during this window.
Inside, the brain’s cortical landscape is bustling; neurons connect, sensory circuits form, and the inner ear shapes up so your voice or a loud clap might already reach curious little ears. Lanugo (that fine baby fuzz) appears, along with vernix caseosa—a creamy protective coat.
The “bump” grows bolder as the uterus crests above the pubic bone. Hunger might spike—time to honour those rising calorie needs with balanced meals: think whole grains, colourful vegetables, legumes, and dairy. Discomforts like ligament pain might come and go, especially after brisk walks or increased activity—pelvic support belts and stretching can be a relief.
Ultrasound time: this is when the detailed fetal anatomy scan occurs, scrutinising everything from the spine to the stomach, cardiac chambers and that oft-anticipated question—boy or girl? If the angle’s right, you’ll know. Size analogies now? Imagine your baby as a pomegranate or a banana, all for illustrative fun though, as every pregnancy writes its own growth story.
Weeks 21–24: Patterns bloom, preparations begin
Your baby grows at warp speed now. Brain folds multiply, giving rise to more intricate sleep-wake cycles, while lungs build new pathways—though you’ll hear, “True breathing, not quite yet.”
The kicks feel less like whispers, more like gentle nudges or sometimes a solid thump. Regular patterns begin to form—bursts of activity followed by restful pauses. Clinicians pay attention to these movements; once perception is routine, it becomes a reassuring ritual to monitor wellbeing.
Your silhouette changes further—centre of gravity shifts, gentle backaches or mild pelvic ache may occur. Think supportive shoes, and perhaps a pregnancy pillow. Appetite, not surprisingly, climbs again. Should growth seem off-track, fundal height checks and, if needed, ultrasound assessments step in for reassurance.
Weeks 25–27: Strengthening, gearing up for birth
Remarkable changes unfold during the closing weeks of the “honeymoon phase”. Rapid brain growth, more subcutaneous fat, enhanced energy stores—the skin smooths, cheeks become rounder, and “kicks” often grow strong enough that even partners can feel the drama.
Survival outside the womb, though still medically challenging, improves by the end of week 27. The lungs, steadily maturing, begin to produce surfactant (a slippery substance critical for breathing at birth), while thermoregulation and feeding coordination await their third-trimester refinement.
Lab work intensifies: screening for gestational diabetes between weeks 24 and 28, repeat bloodwork as indicated (e.g., hemoglobin for anemia, Rh status confirmation), and, in some places, immunity checks for infections. The conversation around birth preferences starts heating up—what are your wishes for pain relief, help with breastfeeding, or who should be present in the delivery room? Jot it down now, while energy is high.
Fetal development: The scientific intricacies
Beneath the growing bump, fetal development surges—synaptogenesis and neural wiring accelerate, reflexes blossom, and sensory functions emerge. Cardiovascular sophistication grows; routine Doppler or ultrasound checks keep tabs on beat and rhythm.
Bones ossify (harden), muscles grow bolder, and every well-timed kick or roll is a testament to your baby’s rising strength. Sensory organs—taste, touch, and especially hearing—add new dimensions to baby’s environment as flavours filter through amniotic fluid and familiar sounds (your laugh, music, traffic symphonies) echo through the uterine walls.
Understanding your symptoms: What’s typical, what calls for care?
Tired of heartburn, surprise cramps or swelling? Each has a physiologic backstory. Round ligament pain—the result of uterine “support ropes” stretching—and backaches emerge as body alignment shifts. Simple tricks—gentle movement, posture checks, hydration, or specialist physiotherapy—often go a long way. For muscle cramps (often in calves or feet at night), consider magnesium-rich foods or supplements as discussed with your provider.
Digestive issues like constipation or hemorrhoids? A fibre-rich diet, hydration, regular movement, and, if necessary, stool softeners work wonders. For heartburn, swap big meals for smaller ones, and tilt the bed’s head a few centimetres.
Braxton Hicks contractions—painless, irregular “practice tightenings”—can surprise you. Regular, painful or accompanied by bleeding warrants a quick call to your care team.
But when does something move from “discomfort” to “concerning”? Heavy vaginal bleeding, significant pain, continuous fluid leaking, severe headache, sudden facial or hand swelling, fever, or notable drop in fetal movement—each signals it’s time to reach out, sometimes urgently.
Medical visits, screenings, and vaccinations: What, when, and why?
Expect a four-week rhythm for appointments if pregnancy is low-risk. Check-ins include not just fetal growth (measured by fundal height and heart tones) but also your weight, blood pressure, urine screens, and mental well-being. For certain pregnancies—multiples or chronic illnesses—additional monitoring and cervical checks add extra caution.
Screenings spike—quadruple biomarker screening for chromosomal or neural tube risks, anatomy ultrasound scans, and the all-important gestational diabetes test are routine by now. Hemoglobin assessments, Rh status, and retesting for certain infections fill out the list, tailored to individual risks.
Vaccinations—seasonal flu, COVID-19, and (later, in the third trimester) Tdap—are part of safeguarding both you and baby, priming routines for optimal protection right from birth.
Dental care? Absolutely. Treat cavities and gum concerns; inform your dentist you are pregnant for safety adaptations.
Nutrition, hydration, and supplements: Nurturing with intention
Weight gain—gradual and steady, often about 0.4–0.6 kg per week for those beginning at a typical BMI—is a sign of healthy growth, though always best adjusted via your provider’s personal recommendation.
Focus on nutrient-dense eating: proteins (dhal, paneer, lean meats), whole grains (brown rice, millets), leafy green vegetables, fresh fruits, fibre, and low-mercury fish like salmon or sardines for those who include seafood. Essential micronutrients? Iron (for blood), folate (cell growth and neural tube protection), calcium and vitamin D (bone health), iodine and choline (brain formation), and omega-3s (DHA especially) all take centre stage. Prenatal vitamins round off the list—skip extra vitamin A (retinol), as excessive amounts can be unsafe.
Avoid high-risk foods: unpasteurised milk, raw or undercooked animal proteins, deli meats unless reheated, and high-mercury fish (shark, king mackerel). No alcohol, and keep caffeine modest—generally under 200 mg per day.
For digestive ease: increase fibre gradually, pair with water, and lean on physical activity. If constipation or heartburn persist, your provider can recommend pregnancy-safe options.
Physical activity, pelvic floor, and posture: Keeping body and mind aligned
Gentle movement is medicine. Walking, swimming, prenatal yoga and Pilates, or stationary cycling keep muscles supple, boost mood, and prepare the body for labour. Intensity? You should be able to chat comfortably while moving. Pause if overheated, short of breath, in pain, or noticing contractions.
Why pelvic floor and core? Kegel exercises fortify muscles crucial for childbirth and postpartum recovery, easing symptoms like urinary frequency. Modify traditional ab work—avoid direct crunches or intense supine exercises after mid-pregnancy; focus on movements guided by a specialist when possible.
Skip contact sports, anything with high fall risk, scuba diving, and extreme heat exposure. If you experience bleeding, regular contractions, chest pain, or dizziness during activity, stop and reach out to your care team.
Safety: Travel, work, and everyday living
Travel feels easier in this trimester—energy returns, discomforts subside for most. Airlines may require a doctor’s note; on longer journeys, move every hour, stretch calves, remain well-hydrated, and consider compression stockings to offset DVT risk.
Seat belt tips? Never skip them—lap belt stays under your bump, shoulder belt crosses your chest.
Workplace: schedule frequent breaks, use supportive chairs, avoid lifting heavy objects. Timing of sharing your pregnancy with your employer? That’s a personal balance—consider workplace structure and support.
Everyday safety includes avoiding hot tubs or saunas, limiting exposure to paint fumes or chemicals, and passing the litter box duty to someone else (toxoplasmosis risk). Check every medicine with your provider—many over-the-counter or herbal remedies lack proven safety in pregnancy.
On skincare: skip oral or topical retinoids, use broad-spectrum sunscreen, opt for pregnancy-friendly treatments under advice.
Sex, bonding, and emotional wellbeing
Is intimacy safe in the second trimester of pregnancy? For most, yes—unless the doctor advises otherwise due to placenta previa, active bleeding, or preterm-labour risk. Comfort first: experiment with positions that avoid abdominal pressure.
Bonding strengthens—kick counts, talking, reading, and music all create pathways for connection, and yes, the baby can often recognize voices by the end of this trimester.
Partners play a pivotal role. Attending check-ups, helping with preparation, or simply providing emotional support all add a layer of reassurance and shared experience—an invaluable asset during these changing times.
Special cases: High-risk pregnancies & common complications
Those carrying multiples, of advanced maternal age, or living with chronic conditions such as hypertension, diabetes or thyroid disorders may require tailored surveillance, more frequent visits, and sometimes, specific dietary or lifestyle adjustments.
Watchful eyes remain trained for signs of preterm labour (regular intense contractions, pelvic pressure, or leaking fluid), placental issues (e.g., low-lying placenta, abruption), and gestational diabetes or high blood pressure. Sudden severe itching could hint at a rare liver complication—cholestasis—so never ignore persistent symptoms.
Infections—urinary tract (UTI), viral exposures—are treated promptly. Reporting early is always encouraged; interventions can make a significant difference.
Looking ahead: Planning for birth and postpartum
The second trimester of pregnancy is prime time to gather information: research and select your birth facility, finalise preferred healthcare providers, tour hospitals, consider birth classes and breastfeeding workshops, and begin tangible preparations—nursery, baby register, car seat choice and installation (do this well ahead of time), exploring suitable paediatricians, and understanding parental leave policies.
Thinking about postpartum support here sets the stage for smoother recovery. Line up resources—lactation consultants, family help, budgets, and insurance checks. Reading about breastfeeding or newborn cues now pays dividends later.
Second trimester checklist and step-by-step window
- Weeks 14–16: Confirm all screenings, update your medicine list with the provider, kick-off a safe exercise routine, book a dental check.
- Weeks 17–20: Attend the anatomy scan, discuss findings, note first flutters, start your baby registry, shortlist birthing and feeding classes.
- Weeks 21–24: Track daily baby movement, optimise sleep with supportive pillows, compare pediatricians, clarify leave details at work.
- Weeks 25–27: Complete gestational diabetes and repeat labs, finalise postpartum help, clarify birth and vaccine plans, prepare for shorter appointment gaps as the third trimester approaches.
Key Takeaways
- The second trimester of pregnancy ushers in welcome relief for many—energy lifts, nausea retreats, while the first kicks create an unbreakable bond.
- Watch for tests—anatomy ultrasounds, maternal serum screening, diabetes checks, anemia and Rh factor screens—each weaves into the safety net for you and baby.
- Prioritise nutrition, listen to hunger cues, focus on iron, folate, calcium, and omega-3s; daily prenatal vitamins fill tiny but important gaps.
- Gentle activity, pelvic-floor care, and posture adjustments can ease aches while prepping body and mind for birth.
- Familiarise yourself with red flags—bleeding, pain, fever, swelling, reduced movement—and contact your care team without hesitation if these occur.
- Resources exist at every step; for tailored guidance and free health questionnaires for your child, try application Heloa.
Questions Parents Ask
How big is my baby during the second trimester of pregnancy?
Throughout the second trimester of pregnancy, growth is surprisingly rapid. Imagine—from a length of around 12–16 cm (roughly head-to-rump or head-to-heel, depending on protocol) and a few hundred grams by weeks 16–20, your little one quickly stretches to 25–37 cm and weighs between 500–900 g by the end of 27 weeks. But every baby is writing their own timeline. Your ultrasound reports and ongoing clinical measurements give the clearest view; never hesitate to ask for clarification—they are there for you.
Can I take ibuprofen or other over-the-counter painkillers?
Seeking safe relief is natural. Generally, non-steroidal anti-inflammatory drugs like ibuprofen, naproxen, or aspirin (especially at higher doses) are avoided during second trimester of pregnancy, as prolonged use can alter kidney function in the fetus or impact their circulation. Paracetamol (acetaminophen) is often preferred for occasional discomfort but always at the lowest possible dose and only when needed. For those prescribed low-dose aspirin (for preeclampsia prevention, for instance), continue only if your clinician directs. Persistent pain or any need for regular medicine should always prompt a personalised discussion with your healthcare provider.
Is it safe to have caffeine in the second trimester of pregnancy?
The consensus? Caffeine, in moderation, is usually fine. Most experts recommend limiting intake to about 200 mg per day (about what you’ll find in a regular cup of coffee—the strength varies). Remember, tea, chocolate, and some sodas or energy drinks count toward the daily amount. Struggling to cut back? Try switching to decaffeinated or milder alternatives. If you have any complications or unique circumstances, your doctor can offer you personalised advice.
Remember, the second trimester of pregnancy is a journey of adaptation and anticipation. Each symptom, milestone, or emotion is part of this dynamic phase—there is no single right path. If in doubt, your care team is just a call away, and resources like application Heloa offer guidance tailored for your family’s health and happiness.
Further reading:
- 2nd trimester pregnancy: What to expect — https://www.mayoclinic.org/healthy-lifestyle/pregnancy-week-by-week/in-depth/pregnancy/art-20047732
- 13 weeks pregnant guide – Best Start in Life — https://www.nhs.uk/best-start-in-life/pregnancy/week-by-week-guide-to-pregnancy/2nd-trimester/week-13/
- The Second Trimester — https://www.hopkinsmedicine.org/health/wellness-and-prevention/the-second-trimester









