The arrival of pregnancy often brings anticipation, hope, and, for many, a slew of strange new bodily sensations. One frequent visitor that quickly sparks anxiety: heartburn during pregnancy. Imagine a persistent burning creeping up behind your chest, just when you’d love to relax after a good meal, or a sour taste lingering in your mouth hours after dinner. Worrying about whether that plate of biryani or a small glass of orange juice will trigger it yet again can feel exhausting. Wondering how to regain comfort and what habits truly help? Get ready—science-backed explanations, daily strategies, and easy-to-follow tips await. What makes heartburn during pregnancy so relentless, and how can you step ahead of the burn without missing your favourite foods or much-needed sleep?
Understanding Heartburn During Pregnancy: The Medical Landscape
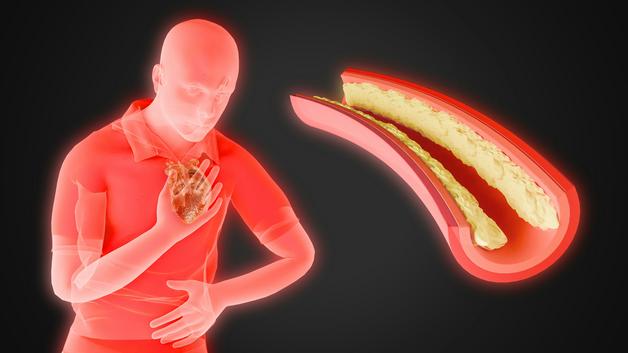
Pause for a moment. Are you experiencing a burning feeling after your meals, an odd bitterness in your throat, or frequent burping unlike what you ever had pre-pregnancy? During this phase, heartburn during pregnancy is nothing out of the ordinary—far from it. Hormonal patterns have shifted dramatically, with progesterone (often called the “pregnancy hormone”) acting not only to relax your uterus but also, unexpectedly, to relax the lower oesophageal sphincter (LES). Now, this LES is a one-way valve meant to keep stomach acids where they belong. When it goes slack, stomach acid can wander upward, resulting in that unmistakable burn. What you’re noticing is, in medical terms, “gastroesophageal reflux,” popularly called GERD.
Not every case looks the same:
- A sharp or burning sensation behind the breastbone (retrosternal pain).
- Bitterness or sour taste from acid reaching your mouth.
- Bloating, frequent belching, even occasional regurgitation
- A heavy chest or discomfort, often worsening lying down.
You may find yourself asking, “Why now?” Besides progesterone, the physical presence of a growing uterus pushes the stomach upward, leaving even less room for proper digestion. It’s a perfect storm for acid escape—particularly in the second and third trimesters, though some notice it earlier due to digestive sensitivity, rapid weight gain, or a genetically more “relaxed” digestive system.
Heartburn and Acid Reflux: Demystifying the Distinction
Are “heartburn” and “acid reflux” just two names for the same annoyance? Not exactly. Acid reflux describes the process—stomach acid journeying upwards. Heartburn is actually the symptom—the pain, the burning, the discomfort you feel. Both can happen any time but are especially common during pregnancy thanks to both hormone-driven slow-down of digestion and the literal squeeze put on your stomach by your growing baby.
You may notice symptoms worsen if you:
- Lie down after a heavy meal,
- Wear tight clothing around your waist,
- Bend over frequently,
- Indulge in foods known to relax the LES (think: chocolate, mint, or caffeine).
Understanding these subtle distinctions can help you describe your experience more precisely to your healthcare provider.
Foods, Habits, and Triggers That Intensify Heartburn During Pregnancy
Ever felt heartburn during pregnancy flare after eating spicy curry or greasy snacks? Certain foods have a knack for making symptoms worse:
- Oily, fried, or high-fat foods
- Heavily spiced dishes or those seasoned with strong condiments
- Tomatoes, citrus fruits, and their juices (acidic troublemakers)
- Chocolates, peppermint, coffee, tea, carbonated waters
Stretching the stomach by eating large meals, drinking much fluid with food, or eating late into the night all increase upward stomach pressure, setting the stage for acid reflux. Wear snug clothing, experience chronic stress, or adopt the habit of reclining post-lunch, and the risk rises higher. Some are just more sensitive—genetics, pre-pregnancy digestive concerns, or quick changes in body weight can each play a role.
Adapting Diet for Relief: Everyday Choices with Science at Heart
You might wonder: can simple tweaks to daily meals really subdue the burn? Parents find comfort in gentle, easy-to-digest foods, particularly when symptoms peak:
- Root vegetables (carrots, potatoes, pumpkin, and zucchini) plus, in moderation, non-citric fruits like banana or pear.
- Well-tolerated starches such as rice (especially whole grain), plain chapati, or idli.
- Cooked cheeses from goat or sheep milk (less acidic), and mild curd or yogurt—these can coat an irritated stomach lining, easing discomfort.
- Mineral water rich in bicarbonate, sipped slowly, may help neutralise excess acid.
Pay attention to cooking methods: grilling, steaming, or baking works much better than anything deep-fried. Try eating four to six smaller meals per day, chewing each bite thoroughly. Not only does this ease digestive load but it reduces pressure on the stomach. It’s best to drink water separately—between meals rather than with them—and maintain at least a gap of two hours before lying down after eating.
Posture, Habits, and Lifestyle Tweaks for Day and Night
Beyond food, day-to-day routines have tremendous impact. After a meal, stay upright—perhaps a gentle walk or simply leaning back instead of reclined seating. To reduce heartburn during pregnancy overnight, think about this: elevate the upper portion of your bed by 6 to 8 inches. A few extra pillows won’t always suffice, but repositioning the bed makes a significant difference. Opt for comfortable, loose clothing—no pressure bands at the waist.
Notice that stress amplifies discomfort? Mindful practices such as gentle prenatal yoga, breathwork, or simple guided relaxation often reduce not just heartburn but overall digestive unease. Establishing small, repeated routines—slow eating, journaling symptoms and food triggers, or brief post-meal strolls—can become valuable sources of relief.
Knowing When Medical Help Is a Must
Though mostly benign, persistent or severe heartburn during pregnancy should always be discussed with your maternity team. Warning signals include:
- Heartburn that lingers despite modifying food or posture,
- Sharp or radiating pain (not classic for straightforward acid reflux),
- Recurrent vomiting, aversion to food, or substantial weight loss,
- Fevers, intense headache, or any bleeding (vomiting blood, black stools),
- Difficulty swallowing.
Modern telemedicine platforms make connecting with doctors quite feasible if clinic visits are not easy. Trust your instincts; prompt professional input can avoid unnecessary discomfort.
Natural Approaches: Safe Soothing During Pregnancy
Curious about natural drinks or herbal options? Herbal teas, such as lemon balm, or a mild ginger infusion (small, grated amounts steeped in hot water), have been historically used to soothe the digestive tract, but always clearance is needed from your care provider first. Yogurt after meals, sipping room-temperature water rich in bicarbonate, or occasionally consuming aloe vera supplements can sometimes offer a calming effect—however, more isn’t always safer, and combining remedies without supervision is discouraged.
Remember, essential oils are not recommended during pregnancy. Keep to natural remedies in moderation and only after professional confirmation, especially if unfamiliar symptoms arise.
Medicines and Safe Pharmacological Relief
Have lifestyle and food modifications fallen short? Healthcare providers can recommend a safe plan. Local antacids containing sodium alginate or calcium carbonate (like chewable tablets) are commonly used for quick relief. Occasionally, magnesium-based preparations work as an alternative. In more persistent cases, doctors may prescribe proton pump inhibitors (such as omeprazole) or a class of medicines known as H2 blockers.
All medicines—even those available over-the-counter—should be started only after medical consultation, as unexpected interactions may affect you and your developing baby. Always communicate openly about any medications or supplements you consider using during pregnancy.
Could Heartburn Be Dangerous?
While deeply uncomfortable, heartburn during pregnancy itself rarely poses direct danger to your baby. Persistent, uncontrolled symptoms can indirectly affect nutrition if eating becomes a daily trial, but this is rare—and usually resolved with prompt adjustments and guidance from your provider.
Tips You Can Implement Today
- Create a food and symptom diary to track what works and what flares your heartburn during pregnancy.
- Space out meals—small, frequent portions are more digestible.
- Stay upright after eating, move gently, and avoid late-night heavy meals.
- Elevate the upper body during sleep for consistency.
- Rely on the support of family, healthcare teams, and parenting communities.
Myths and Facts: Sorting the Real From the Imagined
- Heartburn during pregnancy does not harm your baby.
- Individual tolerance for foods varies—testing gently is more effective than relying solely on food lists.
- All antacids are not the same; safety varies widely during pregnancy—consultation is necessary.
- For most, relief comes soon after birth; in rare cases, lingering symptoms resolve in the postnatal phase.
Key Takeaways
- Heartburn during pregnancy is widespread and usually manageable with tailored strategies—small meals, gentle foods, upright posture, and good hydration practices are the cornerstone.
- Symptoms commonly intensify in the later stages but rarely threaten mother or baby directly.
- Use only remedies—whether herbal or pharmacological—endorsed by your healthcare provider.
- Seek help early for persistent, disruptive pain or if new symptoms emerge.
- Reliable information, understanding support, and tested techniques are all within your reach—explore the Heloa application for trustworthy, personalised advice and free child health questionnaires at every stage of your parenting journey.
Questions Parents Ask
Can heartburn during pregnancy harm my baby?
Parents often worry about risks when that familiar burning takes hold, but rest assured: heartburn during pregnancy is mostly a nuisance for you, not your baby. Symptoms come from hormonal changes and the increasing pressure of your uterus. Actual harm is rare unless severe nausea or ongoing vomiting affects your nutrition—then, timely consultation is best.
When does heartburn start in pregnancy and how long does it last?
Heartburn can appear at any point—from very early weeks right through to the final trimester—though it usually peaks in the second and third trimesters as hormones rise and the baby grows. After birth, symptoms typically disappear or significantly reduce, with most experiencing only a short postpartum phase if heartburn lingers at all.
Are there any natural drinks that can help relieve heartburn during pregnancy?
Cool water—especially varieties high in bicarbonate—offers gentle, immediate relief for many. Light herbal teas like chamomile or lemon balm may help, but always with prior approval from your healthcare provider. Simple, non-acidic smoothies using bananas or oats are another soothing choice for some. A personalised approach is best—monitor your response and reach out to your care team for individual advice.
Further reading: