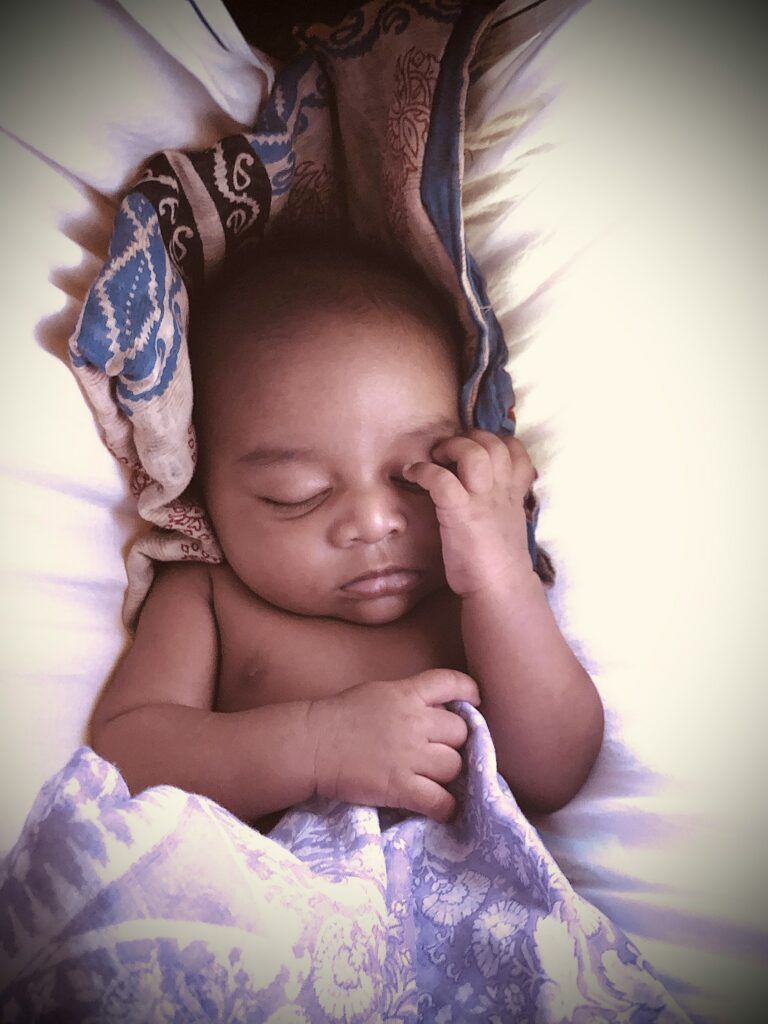
The world of a preterm baby is a place of contrasts—tiny, vulnerable, and yet, in so many ways, resilient beyond words. For new parents, the shock of early arrival collides with an intense surge of responsibility. Questions arise in a rush: How do you support those delicate lungs? What about feeding rhythms when the clock seems irrelevant? Does every cough spell danger? Exploring every corner of care—breathing, nutrition, infection protection, warmth, growth—instantly becomes second nature. Here, medical advances and parental instinct walk hand in hand, guiding fragile beginnings towards healthy tomorrows. Let’s untangle the worries, discover the strategies that bring confidence, and shine a light on how fragile can indeed become formidable.
Preterm baby: key facts and first actions for families
A preterm baby—born before 37 weeks of gestation—ushers in a new set of priorities. Globally, nearly 1 in 10 babies experience such an early debut, each with their own combination of medical and emotional needs. The spectrum is vast: extremely preterm (below 28 weeks), very preterm (28–32 weeks), moderately preterm (32–34 weeks), or late preterm (34–36 weeks). Arrangement in a Neonatal Intensive Care Unit (NICU) soon becomes routine for many, where constant monitoring, special warmth, and respiratory support create a new normal.
Facing respiratory distress, feeding on narrow time frames, temperature swings, and the ever-looming risk of infection—these are not just clinical terms, but daily realities unfolding before anxious parents’ eyes. Fortunately, the modern NICU empowers families to offer skin-to-skin touch, foster kangaroo care, and become real participants in baby’s care. Early breast milk (sometimes fortified), careful handling, and expert guidance all converge on one goal: supporting growth and independence so that the jump to home care comes with readiness, not just relief.
Preparing for homecoming: creating a safe and calm space
The transition home often feels monumental. For a preterm baby, leaving the hospital’s cocoon can be both liberating and intimidating. Before discharge, close coordination with a medical team is essential—sometimes including a paediatric nurse who can help set up support at home or answer emerging questions. Freedom from hospital beeps and wires does not mean sudden freedom from caution; some babies may still require oxygen therapy or have feeding tubes in place, making home visits and professional assistance invaluable.
Change can unsettle newborns—especially those never exposed to household sounds, familiar voices, or the gentle, unprogrammed rhythms of home life. If your baby seems unsettled, cries frequently, or struggles to adjust, gentle affection and patience work wonders. Reclaiming connection after days—or weeks—spent apart sometimes takes as much courage as the hospital stay itself.
Continue generous skin-to-skin contact to reassure your baby and encourage biological stability. Even after being deemed “medically stable,” preterm babies remain more susceptible to everyday infections—both gastrointestinal and respiratory. Meticulous hand washing, strict smoke-free environments, and reducing exposure to crowds are not just precautions, but lifelines at this stage.
Sleep, feeding, and daily routines for preterm babies at home
Promoting healthy sleep patterns
For a preterm baby, sleep isn’t just rest—it’s deep physiological work. Guidance is clear: let your baby sleep beside you (not in your bed) up to six months, on a firm, flat, uncluttered cot or bassinet. Swaddling, mimicking the NICU’s cocooning method, can soothe those recently adapted to enclosed security—be sure to check safe techniques with your nurse. Overdressing and excessive bedding are avoidable hazards. Consider a gentle nightlight or soft lullabies if complete silence and darkness create distress after the noisy, bright NICU environment.
Ventilate sleeping spaces when not in use, and maintain a room temperature around 19°C (66°F)—conditions that stabilise sleep and regulate little bodies still learning their own rhythms. Some preterm babies may need weeks, sometimes longer, to catch up to the daily cycles of full-term infants.
Feeding: nutrition tailored for the tiny and strong
Breastfeeding a preterm baby can mean regular pumping and strategic feeds, sometimes continuing the NICU practice at home. Special preterm formula provides essential nutrients and calories if breast milk is not available or needs supplementation, often until the baby reaches a weight of about 3 kg. With much smaller, sensitive stomachs, preterm babies thrive on more frequent, smaller meals. Trust those hunger cues: a hand to the mouth, rooting reflex, or agitated movement speaks louder than a clock.
Digestive hurdles—regurgitation or constipation—are not rare. Prolonged feeding, need for tube assistance, or muscular fatigue might demand regular check-ins with a paediatrician or nutritionist. A tailored feeding plan, responsive to changes and monitored for progress, ensures that weight gain and development remain on track.
Protecting your preterm baby: hygiene and infection prevention
Preterm babies, with their still-maturing immune defenses, face elevated risks. Thorough hand washing before feeding or changing, steering clear of crowded venues, and face masks for caregivers with coughs or sniffles help erect a sturdy shield. A preterm baby’s home is a fortress: fresh air, yes; tobacco smoke, an absolute no.
Outdoor time, even brief, can uplift mood and regulate sleep, provided the environment is quiet and clean. Localized respiratory virus outbreaks—chickenpox, flu, RSV—make timing and location especially important for outings.
Recognising challenges and understanding medical needs
At first sight, a preterm baby may seem almost ethereal—translucent skin, little body fat, and a vulnerability that belies the robust will to survive. Underdeveloped lungs can lead to respiratory distress syndrome or irregular breathing (apnea). Feeding complicates matters further—weak sucking or swallowing can necessitate tube feeds and dietary fortification.
The struggle for temperature regulation, thanks to minimal subcutaneous fat, makes warm clothing and, sometimes, skin-to-skin or kangaroo care non-negotiable. Medical teams vigilantly watch out for potential hurdles: brain bleeds, developmental delays, jaundice, anemia, and dangerous gut conditions like necrotizing enterocolitis. Every sign—pale skin, lethargy, reduced movement—becomes a clue to address problems early and ensure optimal outcomes.
The NICU journey: immediate care and family involvement
From the moment of birth, urgent interventions revolve around stabilization. Baby placed under a heat lamp or in a temperature-controlled incubator, miniature monitors attached—a choreography of technology and human care. Respiratory support arrives as gentle CPAP, oxygen, or more advanced mechanical ventilation when lungs hesitate to do their job. Medications, like surfactant to mature breathing sacs, and infusions to sustain hydration and energy, are common.
Kangaroo care steps in to stabilise temperature, foster emotional connection, and even support immunity. Progress is not measured only by machines, but also by your baby’s ability to feed by mouth, gain steady weight, and move independently away from wires and tubes. Before leaving the NICU, special instruction sessions teach you quick responses, safe handling, and warning signs to watch for—building confidence for the coming challenges at home.
Treatments and innovative advances for preterm babies
NICUs unite traditional approaches and cutting-edge technology, blending antenatal corticosteroids for mothers at risk of delivering early (improving fetal lung maturity) with interventions such as surfactant administration, specialized ventilators, and tube feeding if needed. Infections require prompt antibiotics; fluid management may call for diuretics.
Kangaroo care now stands as a renowned therapy, not just a feel-good practice—proven to improve neurodevelopment and reduce infection rates. Newer ideas, like stem cell therapies for lung injury and advanced screenings for early detection, continue to expand the medical playbook. Eye care for retinopathy and developmental therapies offered right from NICU stay predict better outcomes, especially with regular parental involvement.
Tracking growth and development
Measuring a preterm baby’s development goes beyond the standard charts—specific references like Fenton or Intergrowth curves allow professionals to chart progress using daily weight, weekly length, and head circumference. The concept of ‘corrected age’—your baby’s actual weeks minus those missed in the womb—guides evaluation of milestones, often until the toddler years.
Regular checks for movement, language, and learning, relying on established tools like the Bayley Scales, intervene early at any sign of delay. Protein supplements, multivitamins, and careful feeding plans (adapted for tolerance and digestive power) help bridge those precious early months. Referrals for physiotherapy, occupational therapy, or speech therapy can make a pivotal difference—each small step towards walking, talking, and self-discovery brings new celebrations.
Long-term health and ongoing support
A preterm baby’s health story stretches beyond NICU walls. Risks of learning difficulties, speech delays, chronic lung problems like asthma, and even behavioural challenges may exist, influenced by how early the baby arrived and any complications that arose. Some children need support in school, require tailored diets, or benefit from speech or physical therapy. Regular eye and ear screenings, ongoing nutritional monitoring, and quick responses to infections are part of the extended care network.
Emotional resilience is built day by day—parent groups, educational workshops, and attentive professionals offer strength and insight. Harnessing hospital experiences, home routines, community resources, and family support allows your child, and you, to steadily flourish. The journey through early adversity often builds a foundation of tenacity that will serve a preterm baby and their family throughout life.
Everyday routines and nurturing emotional connection
Day-to-day life can sometimes feel like a dance—feedings often longer and more frequent, small diapers prompting double-checks about hydration, and sleep routines tailored for maximum serenity. Quiet, cozy, and consistent environments calm jangled nerves for both baby and parent. Play, even if simple—gentle talking, music, soft toys—feeds cognitive growth and emotional bonds.
Stay vigilant: regular appointments for vision, hearing, and developmental tracking are invaluable early. And never discount the power of small, mindful moments—holding, singing, or just gazing at each other. Balancing these routines with your own rest deserves priority too. Every parent’s intuition, sharpened by learning and experience, becomes the secret sauce in a preterm baby’s comeback.
Causes, signs, and risk factors behind preterm birth
Why does preterm birth happen? Sometimes answers elude even the best doctors. Still, certain patterns emerge: spontaneous early labour, pregnancy complications like high blood pressure or preeclampsia, or multiple gestations all raise the chance. Medical factors—maternal diabetes, kidney disorders, thyroid imbalances—can contribute. Environmental and lifestyle factors, from exposure to smoke to unmanaged stress or poor prenatal care, add layers of complexity.
Classic signs suggesting early labour—regular contractions, lower back pain, watery or bloody discharge—demand immediate attention. Maternal age (under 17 or over 35), previous preterm delivery, or infections during pregnancy raise risk. Quick recognition and prompt support offer a real shot at delaying birth and aligning the best-possible care.
Preventing preterm birth: progress and hope
Science races to stay ahead, with advances in the early detection of risk—novel biomarkers, precision ultrasound, even smart wearable devices that monitor uterine activity. Supplementing with progesterone, surgical options for cervical weakness, nutritional optimization, and robust prenatal programmes shape everyday prevention strategies.
Reducing smoking, targeting infections, and providing timely medical intervention continue to improve outcomes. Personalised medicine, a growing field, tailors these advances to individual pregnancies, reducing rates of preterm birth and improving short- and long-term wellbeing.
The future: progress, partnerships, and global lessons
The face of neonatal medicine is changing—gentler ventilation, precise brain and lung therapies, dedicated research into preterm nutrition, and the rise of Kangaroo Mother Care supported by international health bodies. Community programmes empower families, bring mothers and babies closer to care, and chip away at survival gaps between regions.
Global focus on maternal wellbeing, research funding, and education take on the challenge of making every preterm beginning a story of hope. The journey is complex; the rewards immense.
Key Takeaways
- A preterm baby brings distinct challenges and remarkable possibilities—modern treatments, vigilant monitoring, and nurturing routines offer a solid foundation for growth.
- Early recognition of complications or warning signs empowers families to seek the right help sooner, averting bigger issues.
- Practices such as kangaroo care, breast milk fortification, and strict infection prevention—start in NICU, continue at home, and become lifelong habits.
- Developmental milestones may follow a different pace, with ‘corrected age’ guiding parents and professionals.
- Long-term tracking and early interventions maximise every child’s potential, whatever their starting line.
- Medical innovations and parental engagement keep improving prospects every year—added support is never out of reach.
- For tailored advice, developmental questionnaires, and ongoing support, explore the application Heloa—a valuable digital companion for your parenting journey.
Questions Parents Ask
How can I improve my preterm baby’s weight gain?
Supporting the weight gain of a preterm baby can feel like a delicate balancing act. Delay is common, but practical steps abound. Breast milk, frequently fortified, delivers key calories and natural immune protection—sometimes donor milk or special formula is suggested if the mother’s supply is low. Collaboration with your healthcare team keeps feeds tailored to your baby’s tolerance, often increasing in small increments and sometimes blending oral and tube feedings. If digestion problems or reflux seem to cause setbacks, it’s perfectly reasonable to ask for a neonatal dietitian’s or lactation consultant’s help—they’ll adjust the feeding plan, ensuring the best possible start.
Can preterm babies go outside?
Yes, many preterm babies enjoy fresh air—thoughtful planning is the only prerequisite. Check with your paediatrician before that first outdoor trip, considering your baby’s age, overall condition, and local weather. Quiet, smoke-free environments are best, with outings brief and away from crowds, particularly during respiratory virus seasons. Dress your baby in light, comfortable layers and watch closely for early signs of fatigue or chill. This way, you help your little one enjoy the world safely, step by step.
Is it possible for a preterm baby to have normal development?
A preterm baby often surprises even doctors by reaching milestones close to their peers, especially when the family and medical teams provide early support. Some motor or language delays may appear, but energetic intervention and consistent check-ups can narrow the gap. Activities—gentle play, reading aloud, responsive caregiving—add up. While each journey unfolds in unique ways, timely therapies, encouragement, and observation help your preterm baby develop, connect, and thrive in their own time.
Further reading: