Awaiting the birth of a child often brings a blend of excitement, hope, and the fluttering of tiny feet deep within. But just as you begin to memorise the rhythm of those heartbeats on the scan, a term like “placenta previa” can enter the picture—surprising, puzzling, and perhaps a little frightening. Parents may find themselves wrestling with urgent questions: Why is the placenta so low? Will the baby be safe? Can this mean bed rest, sudden hospital stays, or even an unexpected operation? Rather than searching in panic, let’s break down what matters most: how placenta previa is spotted, what it means for you and your baby, and how expert care can help you prepare, adapt, and stay mentally strong through every stage.
Understanding Placenta Previa: What’s Happening and Why?
Placenta Placement and What Makes Previa Different
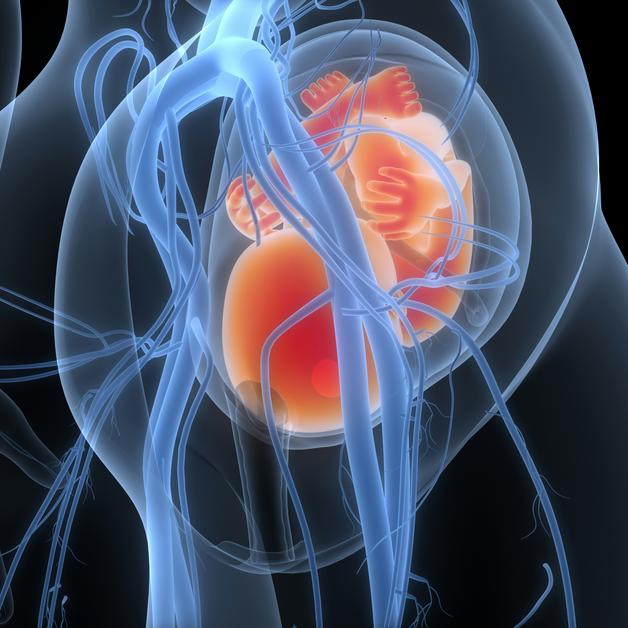
A healthy, developing pregnancy usually means the placenta (that all-important, life-sustaining organ linking baby to mother) settles high in the uterus, well away from the cervix. In placenta previa, however, the placenta anchors itself lower down, sometimes so close to or even covering the cervix—the very passage your baby would usually exit during natural birth. Sometimes it completely covers the opening (complete previa), sometimes just a portion (partial), and sometimes just edges close to it (marginal). There is also the “low-lying” variant, where the placenta sits within 2 to 3.5 centimetres of the cervical opening but doesn’t touch or cover it.
You might wonder—did I do something to cause this? Could it have been prevented? The answer, most often, is no. Factors like previous caesarean section, history of uterine surgery, advanced maternal age, carrying twins or more, use of fertility treatments, uterine fibroids, or even genetics can gently tip the odds toward placenta previa—but it’s rarely within anyone’s control.
And here’s a small relief: in many cases, what’s labelled as “low-lying” early in the second trimester moves safely upward as the uterus grows—thanks to the remarkable elasticity of maternal tissues. Regular ultrasound scans (the gold standard for diagnosis and follow-up) quietly track these changes, ensuring decisions are always based on precise information.
Causes, Risk Factors, and “Placental Migration”
Having a good understanding of what increases the odds helps in planning, not blaming. Key risk factors for placenta previa include:
- Multiple previous pregnancies—each adding to little changes in the uterine lining.
- Previous C-sections or any surgery that leaves a scar on the uterus.
- Being above the age of thirty-five at the time of pregnancy.
- Short gaps between pregnancies.
- Smoking or exposure to harmful substances.
- Conception via assisted reproductive techniques (like IVF).
Again, even if none of these applies, placenta previa can still happen. You may also read the phrase “placental migration.” This simply means that as your womb expands, the placenta (which is firmly rooted but the surrounding muscle stretches enormously) often ends up further from the cervix all by itself, especially by the third trimester.
Recognising Symptoms: When Should Alarm Bells Ring?
Classic Presentation: Painless Vaginal Bleeding
One of the hallmark signs of placenta previa is sudden, bright red painless vaginal bleeding—usually after the midway point of pregnancy, often surprising in its absence of discomfort. Maybe there’s a bit of mild pressure or feeling of tiredness, but contractions are rarely severe. Sometimes, after intercourse or an internal examination, light spotting can occur—a sign to be extra gentle and cautious.
However, up to one third of cases may be detected silently, through routine scans before any bleeding has shown up. Always take any bleeding after the 20th week as a reason to consult without delay—minutes matter more than courage here.
Diagnostics: Precision With Ultrasound
Reliable and safe, ultrasound is the foundation for diagnosing placenta previa. The initial scan is usually abdominal, but a transvaginal scan offers the clearest view of the placenta’s relationship to the cervix—guiding doctors in mapping out the degree of covering and the exact distance. If vaginal bleeding is significant, blood tests will be done to check haemoglobin, blood group (important for possible transfusion), and clotting function.
A vital point: avoid any internal vaginal examination unless previa has been ruled out, as even gentle touch can trigger serious bleeding. Diagnosis sometimes also requires ruling out other causes, such as placental abruption (where the placenta peels away) or, rarely, uterine rupture.
Types and Delivery Planning: What If Placenta Previa Persists?
Classification and What It Means for Birth
Diving deeper, placenta previa has several shades:
- Complete previa: Full cervical covering; only a planned caesarean is possible.
- Partial previa: Partial coverage; caesarean is still recommended.
- Marginal previa or low-lying placenta: The edge nears but doesn’t cover the opening. Here, repeated scans and clinical judgement sometimes make a trial of natural birth possible, but only under the strictest supervision and with safety nets in place for quick intervention.
Delivery plans are crafted individually, but generally a scheduled caesarean is advised around 36 to 37 weeks, before labour starts naturally. If there’s late bleeding, urgent decisions may be made in hospital.
Complications: Thinking Ahead Without Panic
Maternal Complications
The single greatest risk in placenta previa is heavy bleeding (haemorrhage), which can escalate in late pregnancy or just after delivery. Timely medical care, though, makes a huge difference. Sometimes life-saving measures like blood transfusion or—rarely—removal of the uterus (hysterectomy) might be needed. There’s also a risk of infection and, if the placenta invades unusually deep into the muscle (placenta accreta spectrum), complex surgery could become necessary.
Fetal Risks
For babies, biggest concerns include being born preterm (if early delivery is required), having low birth weight, and needing support in the neonatal unit. If the placenta is very low, the baby might be lying sideways (transverse), making vaginal delivery impossible. Rarely, blood vessels from the placenta can overlie the cervix (vasa previa)—an urgent medical situation. That’s why ongoing scans and careful planning offer such a safety net.
Daily Life, Monitoring, and Emotional Wellbeing
Dealing With Bleeding and Adjustments to Routine
If you experience significant bleeding, doctors often advise hospital admission for observation, at least at first. Bed rest, pausing normal activities, refraining from sexual intercourse, and continuous monitoring are all common recommendations. Occasionally, corticosteroid injections might be given—for baby’s lungs if risk of early delivery appears. Tocolytics (medications to delay labour) could also be needed if contractions attempt to start.
Milder or stabilised cases might be managed at home, with precise instructions about when to seek urgent help. “Listen to your body, but ring your doctor if anything feels off”—that’s the golden rule.
Route of Delivery: Caesarean or Natural?
The preferred method is a scheduled caesarean if the placenta even partially covers the cervix. Natural birth remains an option only when repeated scans confirm the placenta is safely away and both mother and baby’s condition are reassuring. In true emergencies—profuse bleeding, maternal or fetal distress—the team moves quickly to ensure the best outcome.
Empathy, continuous reassurance, and open dialogue matter every bit as much as clinical skill. There’s no shame in worry—speaking up, asking for support, or seeking counselling can make all the difference.
Prevention, Life After Birth, and Parental Wellbeing
Early Detection, Practical Strategies, and Family Support
Early and regular prenatal ultrasounds remain your best friend—spotting placenta previa early, tracking changes, and planning safely. Let your doctor know about previous C-sections, surgeries, or fertility treatments at your very first visit. Quitting tobacco and arranging practical support for physical rest at home are simple but effective ways to reduce risk and cope better if diagnosed.
After birth, attention shifts to preventing excess bleeding, ensuring smooth uterine recovery, and rebuilding your energy—iron-rich foods, staying hydrated, and supplements if needed often make a real difference. Never hesitate to talk about anxiety or stress—professional help, honest conversation with loved ones, and focusing on recovery, both physical and emotional, is always encouraged.
Key Takeaways
- When the placenta previa is diagnosed, remember it means the placenta has settled low in the uterus, sometimes covering the cervix.
- Classic warning signs: bright red, painless vaginal bleeding after 20 weeks—always report this immediately.
- Obstetric risk factors include prior C-section, uterine surgery, multiple pregnancies, maternal age over 35, smoking, and fertility treatments.
- Most cases receive clear guidance with regular ultrasound monitoring and personalising birth plans to limit risk; usually, a caesarean is advised, though rare low-lying placentas might make vaginal birth possible.
- The major risks are excessive bleeding for the mother and premature delivery for the baby. Individualised, attentive care significantly reduces these dangers.
- Emotional support, clear communication with healthcare professionals, and not blaming oneself are all key. Parenting under these conditions can be challenging, but it is also manageable with preparation and help.
- Explore practical, reliable resources; tools like Heloa provide personalised medical advice and free health checklists for children—reliable daily support, right at your fingertips.
Questions Parents Ask
Can placenta previa go away by itself during pregnancy?
Absolutely, in many pregnancies where a low-lying placenta is noticed midway, it lifts further up the uterine wall as your womb expands—a process often called “placental migration.” As weeks go by, repeat ultrasounds can show a reassuring distance developing between the placenta and the cervix. Nonetheless, attending every scheduled check-up and sticking to the obstetrician’s advice ensures the best outcome for you and your baby.
Is normal delivery possible with placenta previa?
It depends entirely on how far the placenta is from the cervix by late pregnancy. If it’s fully or even partly covering the opening, caesarean is almost always the safer choice; no room for risks here. But if the placenta is low-lying and, over time, moves well up and away—with all other signs healthy—a carefully supervised natural delivery may be discussed. Always clarify your situation directly with your specialists.
What should be avoided if diagnosed with placenta previa?
Doctors often recommend cutting back on anything that could stir up trouble—vigorous exercise, heavy lifting, and sexual intercourse, particularly as pregnancy advances. Self-examinations, especially of the vagina, are to be strictly avoided unless a doctor prescribes or supervises it. The idea is to avoid provoking unnecessary bleeding, keeping the focus on gentle routines and careful supervision as your baby grows.
If in doubt, rapid consultation saves precious time and sets up the best odds for a happy, healthy birth.
Further reading: