A glass of milk at breakfast, a bowl of curd with lunch, an ice cream after school… and then the tummy starts acting up. Bloating, cramps, loud gurgling, loose motions, sometimes even tears after a bottle. It is natural to wonder: is this lactose intolerance in children or is it a milk allergy? And the next question follows quickly: should all dairy stop?
In most cases, lactose intolerance in children is a digestive issue linked to an enzyme (lactase). It is usually dose-dependent, meaning small amounts may be fine while larger portions trigger symptoms. With the right medical clarity and age-wise clues, many families can bring back calmer eating at home, in school tiffins, and when outside.
Lactose intolerance in children: what it is and why it happens
What lactose intolerance means (and how lactose is normally digested)
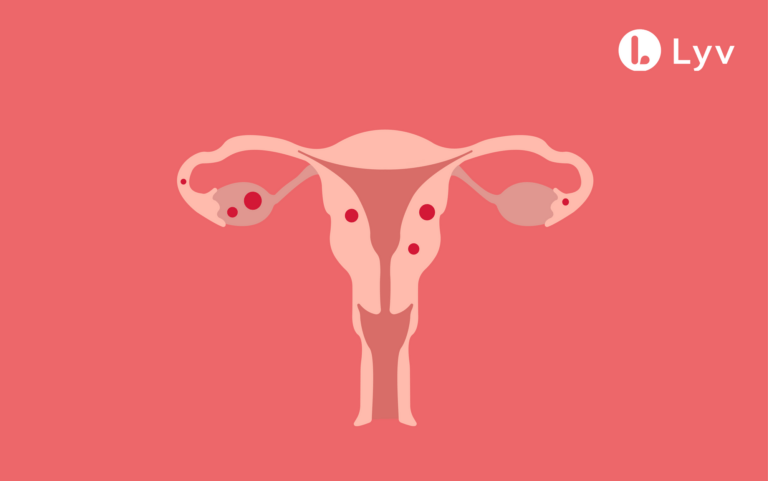
Lactose is the natural sugar found in milk (including breast milk) and most dairy foods. After your child drinks milk or has dairy, lactose usually travels to the small intestine, where it is split into two smaller sugars, glucose and galactose. These are then absorbed into the blood and used as energy.
If lactose is not broken down properly, it moves onward into the colon. There, gut bacteria ferment it. Fermentation creates gas, and lactose also pulls water into the bowel, leading to bloating, cramps, and watery stools.
The role of lactase and what “lactose malabsorption” means
Lactase is the enzyme that splits lactose. It sits on the brush border (the surface layer) of the small intestine.
When lactase activity is low, lactose is partly digested or not digested at all. Doctors call this lactose malabsorption (or maldigestion). Not every child with malabsorption has symptoms every time, because symptoms depend on:
- the lactose dose
- the child’s remaining lactase activity
- how fast food moves through the gut
- recent infection or irritation of the intestine
Two mechanisms explain most symptoms:
- Osmotic effect: undigested lactose draws water into the intestine, which can lead to loose, watery, sometimes acidic stools (can irritate the diaper area)
- Colonic fermentation: bacteria produce gas (hydrogen, sometimes methane), which can cause bloating, cramps, flatulence, and belly noises
Lactose intolerance vs “dairy sensitivity” vs milk allergy
Lactose intolerance in children is not an immune reaction. It is mainly digestive and often dose-related.
“Dairy sensitivity” is a loose term people use differently. It may refer to lactose intolerance, or sometimes to discomfort with milk proteins.
A cow’s milk protein allergy (to casein or whey) is immune-based. Skin symptoms (hives, eczema flares) or breathing symptoms (wheeze, tight chest) point away from lactose intolerance.
Types of lactose intolerance in children and common causes
Primary lactose intolerance (lactase non-persistence)
This is the most common type worldwide. Lactase levels are high in infancy, then gradually fall in many people as they grow.
In children, primary lactose intolerance in children is more often noticed later, school age or adolescence, when portions increase (milk, flavoured milk, dairy sweets, ice cream).
Secondary lactose intolerance (after infection or gut irritation)
Secondary lactose intolerance in children happens when the small intestine lining is irritated or injured and produces less lactase for some time.
Common triggers include:
- viral gastroenteritis (stomach infection)
- giardiasis (Giardia)
- celiac disease
- inflammatory bowel disease
This form is often reversible once the gut heals and the underlying issue improves.
Congenital lactase deficiency (very rare)
This is extremely uncommon. Symptoms start in the first days of life because the baby cannot digest lactose in breast milk or standard formula.
It can cause severe watery diarrhoea soon after feeds, with a real risk of dehydration and poor weight gain.
Temporary low lactase in premature babies
In preterm babies, the intestine may be immature and lactase production can be low for a while. As the gut matures, tolerance often improves.
Genetics, prevalence, and age of onset
LCT gene variants and lactase persistence
Whether lactase stays high beyond early childhood is strongly influenced by genetics (variants near the LCT gene). Genes influence risk, but day-to-day symptoms still depend on dose and gut health.
When lactose intolerance tends to start
- Infants: primary lactose intolerance is unusual. If symptoms occur, prematurity or secondary deficiency after illness is more likely.
- Toddlers: secondary intolerance after a stomach infection is common.
- School-age and teens: primary lactose intolerance in children becomes more likely.
Symptoms parents may notice
Typical symptoms
After lactose-containing foods/drinks:
- crampy tummy pain
- bloating and distension
- gas, gurgling sounds
- loose stools/diarrhoea (sometimes acidic)
- nausea (especially after larger amounts)
Vomiting can happen, particularly in older kids, but it is not the most typical sign.
Babies and young children
Symptoms may look less specific:
- irritability or crying after feeds
- gassy belly, distension
- frequent loose stools
- diaper rash worsened by acidic stools
Because several infant conditions overlap (reflux, infections, milk protein allergy), it helps to consider timing and growth.
School-age children and teens
Older children may notice symptoms after cereal with milk, chocolate milk at school, ice cream, or dairy desserts.
There may also be urgency to pass stools, embarrassment due to gas/bloating, or worry about school tiffins and outings.
How soon after dairy?
Often within 30 minutes to 2 hours, but it can be later depending on the dose and how fast food moves through the gut.
Dose-response: why one day is fine and the next is not
Many children tolerate small amounts of lactose, especially with meals. A realistic aim is to find the child’s personal threshold.
Lactose intolerance in children by age: what’s common and what’s rare
Infants
In full-term infants, persistent primary lactose intolerance in children is uncommon. More likely situations:
- prematurity-related low lactase
- temporary secondary lactase deficiency during/after gastroenteritis
Congenital lactase deficiency is rare but serious.
Toddlers
After gastroenteritis, milk and ice cream may trigger loose motions and cramps for a short period. This often improves as the gut lining recovers.
Older children and teens
Primary lactose intolerance in children becomes more plausible, often linked with routine habits like milk at breakfast or ice cream after play.
Lactose intolerance vs milk allergy: how to tell the difference
Digestive problem vs immune reaction
Lactose intolerance in children is enzyme-related and usually stays in the gastrointestinal system.
Milk protein allergy is immune-based (IgE or non-IgE) and may affect skin, breathing, and general wellbeing.
Signs that suggest milk allergy rather than lactose intolerance
These are not expected in lactose intolerance:
- hives, itching, swelling of lips/face
- eczema flare clearly linked with milk
- wheezing, breathing difficulty
- very rapid reactions after tiny amounts
Any suggestion of anaphylaxis (breathing trouble, collapse, severe swelling) needs emergency care.
Why management changes
“Lactose-free” does not mean “milk-protein-free”. Lactose-free dairy still has milk proteins, so it is fine for lactose intolerance but not for milk allergy.
For suspected milk protein allergy, clinicians may suggest extensively hydrolysed formulas, or sometimes amino-acid formulas.
When symptoms may point to something else (red flags)
Red flags to watch for
Simple lactose intolerance in children should not cause weight loss or poor growth by itself. Check in with a clinician if you notice:
- weight loss or poor weight gain
- dehydration signs (very few wet nappies, dry mouth, unusual sleepiness, in babies, sunken fontanelle)
- diarrhoea that persists or keeps returning
- prolonged food refusal
Blood in stool, fever, severe pain, repeated vomiting, night symptoms
These are not typical of lactose intolerance:
- blood in stools
- fever with ongoing gut symptoms
- severe/persistent vomiting
- significant abdominal pain
- pain waking the child at night
- worsening overall condition
How doctors diagnose lactose intolerance in children
Symptom patterns and a short diary
Doctors often start with the story:
- trigger foods (milk, flavoured milk, cream, ice cream, dairy sweets, processed foods with milk powder)
- timing and dose
- recent infection, antibiotics, stress
- growth and energy levels
A food-and-symptom diary for a few days to 1-2 weeks can help.
Elimination and re-challenge
A common approach:
1) reduce/avoid lactose for about 2 weeks
2) reintroduce gradually
If symptoms settle and then return with reintroduction (often dose-related), it supports lactose intolerance in children.
Hydrogen breath test (H2)
Procedure usually involves fasting, a baseline breath sample, a lactose drink, then breath samples every 30 minutes for 2-3 hours.
A rise in breath hydrogen suggests lactose reached the colon undigested and was fermented.
Stool tests in infants
Sometimes stool tests help detect carbohydrate malabsorption:
- stool acidity (low pH)
- reducing substances
When to look for secondary causes
If symptoms persist despite a properly done lactose reduction, clinicians may look for:
- celiac disease
- inflammatory bowel disease
- giardiasis or other infections
Treatment and day-to-day management
Lactose reduction vs lactose-free: avoid over-restriction
Many children do well with reduction, not complete avoidance. The aim is comfort plus steady nutrition.
Some families find it simple to keep lactose-free milk at home for daily use, and test small portions of regular dairy when it is convenient.
Portion-size strategies
- choose one dairy item to test
- start with a small portion with a proper meal
- increase slowly if symptoms stay calm
- if symptoms return, step back to the last tolerated portion
Lactase enzyme supplements
Lactase tablets/chewables can be used by older children right before dairy meals. Lactase drops may be used in some infant situations with medical guidance.
This can be useful for birthday parties, weddings, restaurants, and school trips.
Managing flares: hydration and comfort
If diarrhoea is significant, focus on fluids:
- small, frequent sips of oral rehydration solution
- continue breast milk or formula for infants
- temporarily switch to lactose-free/low-lactose choices until stools settle
Avoid anti-diarrhoeal medicines in young children unless advised.
Foods to limit and foods often tolerated
Higher-lactose foods
- regular milk and milk drinks
- cream-based desserts
- ice cream
- fresh cheeses
- foods with added milk solids/milk powder
Lower-lactose foods many children tolerate
- curd/yoghurt (cultures partially break down lactose)
- kefir
- hard/aged cheeses (usually very low lactose)
Tolerance varies.
Lactose-free dairy products
Lactose-free milk and lactose-reduced dairy help many children maintain protein and calcium intake while reducing symptoms.
Reading labels and avoiding hidden lactose
Ingredients that may signal lactose
Look for:
- lactose
- milk sugar
- dry milk solids
- non-fat dry milk powder
- whey
Processed foods with “surprise” lactose
Lactose can appear in:
- breads/buns
- breakfast cereals
- instant soups
- salad dressings
- bakery mixes
Medicines and supplements
Some medicines use lactose as a filler. If symptoms seem out of proportion, a pharmacist can check ingredients.
Best milk and curd alternatives for kids
Lactose-free cow’s milk
Often the easiest swap: similar protein and calcium, but lactose already broken down.
Plant-based drinks
They are lactose-free, but not nutritionally identical.
- soy drink often matches protein needs better
- almond/coconut drinks are usually low in protein
Choose fortified options (calcium, vitamin D) and unsweetened versions when possible.
Nutrition and growth: keeping bones and energy on track
The trio to watch: calcium, vitamin D, protein
If dairy is reduced widely, the bigger risk is nutritional during growth. Keep an eye on:
- calcium
- vitamin D
- protein
Also consider iodine and vitamin B12 depending on the overall diet.
After secondary lactose intolerance: reintroduce slowly
After gastroenteritis, lactase activity can recover. Many children improve in 1-2 weeks, sometimes longer.
When stools are stable:
- start with small amounts with meals
- increase slowly over 1-2 weeks
- begin with yoghurt/curd or hard cheese
Infants: breastfeeding and formula
Breastfed babies
In a healthy full-term breastfed baby, primary lactose intolerance in children is rare. Lactose in breast milk does not reduce just because the mother stops dairy.
Formula changes
Changing formula without guidance can delay the correct diagnosis. Depending on the situation, a clinician may suggest a brief lactose-free formula trial or a hypoallergenic formula for suspected milk protein allergy.
To remember
- Lactose intolerance in children is linked to low lactase activity, symptoms are mainly digestive and often dose-dependent.
- Primary lactose intolerance in children is uncommon in infants, secondary intolerance after gastroenteritis is common and often temporary.
- Red flags (blood in stools, dehydration, severe pain, weight loss, night-time pain) need medical assessment.
- Diagnosis may involve symptom patterns, a short elimination-and-rechallenge, and sometimes a hydrogen breath test.
- Many children can keep some dairy using lactose-free staples, smaller portions, yoghurt/curd, and lactase enzyme when useful.
- Support is available. Health professionals can guide testing, nutrition, and safe reintroduction. You can also download the Heloa app for personalised follow-up and free child health questionnaires.

Further reading: