You typed what does the umbilical cord do because you want straight, science backed answers without alarm. Here is the heartbeat of it, the cord is your baby’s supply line during pregnancy, a living bridge that brings oxygen and nutrients in, then carries waste out. You also want to know what does the umbilical cord do at birth, whether waiting to clamp changes anything, and how to care for the stump at home. All of that matters, and yes, you can make calm, well informed choices.
Big picture first, then details that help with real decisions. You will see how blood flow works, how scanning and monitoring guide care, what to do when something looks unusual, and how simple routines keep the stump healthy.
What does the umbilical cord do, quick answer for parents
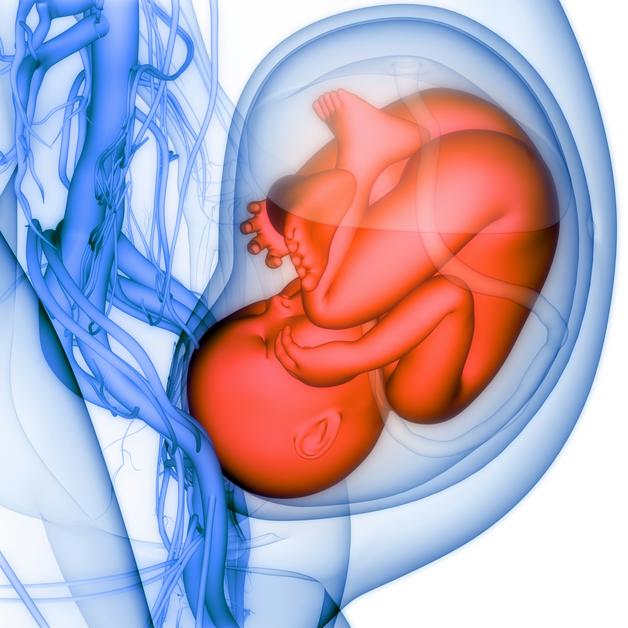
Think of the cord as a two way roadway with protective insulation. Oxygen rich blood travels in one large vessel, and used blood returns through two smaller vessels. More simply, what does the umbilical cord do, it delivers what helps a baby grow, it removes what a baby no longer needs.
- One vein brings oxygen and nutrients toward the baby, this is the Umbilical vein function in action.
- Two arteries return carbon dioxide and waste to the placenta, that is the Umbilical arteries function.
- The placenta also sends protective antibodies late in pregnancy, so the newborn starts life with early immune help.
You may wonder, if this is so efficient, does timing at birth matter. A short wait before clamping can top up your baby’s blood volume and iron stores. Sometimes, immediate care for the parent or baby comes first. Both paths can be safe and thoughtful.
Anatomy, what the umbilical cord is made of
Vessels, wharton’s jelly and membranes
At its core, the cord is three vessels cushioned in a springy gel and wrapped in a thin membrane. That gel, Wharton’s jelly, is rich in water binding molecules that keep the vessels open when the cord bends or gets squeezed. The outer layer, the amnion, smooths the surface and protects the inside from friction.
For quick reference, Umbilical cord anatomy looks like this in practice:
- A single vein, larger and softer walled, carries oxygenated blood toward the baby.
- Two arteries, muscular and more resistant, return deoxygenated blood to the placenta.
- The jelly resists kinking, so flow continues even during contractions.
Cord length, coiling and insertion patterns
Cords vary. Many measure about fifty to sixty centimeters. A very short cord can limit movement and tug during delivery. A very long cord can loop, knot, or drop beside the baby when the water breaks. Clinicians also notice twist patterns, some cords coil a lot, some very little, both extremes can be a sign to look closer.
Where the cord inserts on the placenta matters too.
- Central cord insertion and eccentric insertions are common and usually fine.
- Marginal cord insertion attaches near the placental edge, it may prompt extra observation.
- Velamentous cord insertion means vessels travel within membranes without the jelly, which leaves them unprotected if pressure or tearing occurs.
For parents tracking measurements and notes in reports, you might also see the phrase Umbilical cord length listed in centimeters. If numbers sit at either extreme, your team explains whether anything changes in care.
Innervation and sensation basics
The cord has no pain fibers. Cutting it is painless for the newborn, the real work in those first breaths is breathing and shifting circulation.
Physiology, how the cord supports fetal circulation and growth
Pathways for oxygen, nutrients and waste
Baby’s blood receives oxygen and nutrients at the placenta, then streams through the umbilical vein into the fetal circulation. Used blood circles back through the two umbilical arteries. In medical shorthand, think Placental exchange via the umbilical cord, with gases moving by diffusion and many nutrients moving by special transporters.
- The route for fresh blood is the Oxygenated blood path: umbilical vein to fetus.
- The returning route is the Deoxygenated blood path: fetal arteries to placenta.
You might ask, what does the umbilical cord do during a contraction. Thanks to the jelly and coiling, flow usually continues, although strong or repeated compression can temporarily dip delivery of oxygen.
Transport mechanisms and fetal hemoglobin
Glucose and amino acids cross via transport proteins, calcium and iron have their own channels, and antibodies cross through special receptors in late pregnancy. The fetus makes HbF, a form of hemoglobin that grabs oxygen more tightly than adult hemoglobin, which helps the baby capture oxygen efficiently from the placental side.
Hemodynamics, acid base and cord gases
Right after birth, a tiny sample from the cord can show how the baby tolerated labor. Clinicians often check Cord gas, an analysis of pH and carbon dioxide that offers a single timepoint snapshot. When needed, Umbilical cord blood gas analysis supports quick newborn care and guides follow up.
Embryology and development of the cord
The cord begins as a simple stalk in the earliest weeks, then gains vessels from the yolk sac and the allantois as the placenta matures. By the end of the first trimester, the classic pattern, two arteries and one vein, is set. Coiling increases as the baby moves, and as vessels lengthen and respond to flow. A balanced twist pattern helps prevent compression, so very high or very low coiling can be a clue to look at growth and well being more often.
You may be thinking, what does the umbilical cord do as it forms. It builds the highway before the traffic arrives, that way, by the time organs need fuel, the path is open.
Role during labor and delivery
Cord function during contractions and fetal monitoring
On the monitor, quick dips in the fetal heart rate that vary in timing often point to cord compression. Nuchal loops, called a Nuchal cord, are common and usually harmless. If the loop tightens, the heart tracing may change, your team adjusts positioning and fluids, and if needed, moves to delivery.
Cord clamping, cord milking and timing trade offs
Here is where choices meet physiology. Delayed cord clamping for about one to three minutes can increase newborn blood volume and build iron stores, which lowers early anemia. Immediate cord clamping may be used when maternal bleeding is heavy or when a baby needs help right away. Some studies suggest that cord milking can be helpful in certain scenarios, for very preterm babies there have been safety questions, so many teams prefer a short delay when possible. A small trade off with delayed clamping is a modest rise in jaundice that might need light therapy, see Cord clamping and newborn jaundice for details you may see in hospital leaflets.
So, what does the umbilical cord do during those first minutes after birth. It continues to pulse, sending a final transfusion of blood as the lungs inflate and the circulation shifts.
Cutting the cord and neonatal transition
As the baby breathes, vessels in the lungs open widely, the fetal shunts begin closing, and the cord’s flow naturally fades. The clamp goes on, the cut is painless, and the focus turns to warmth, breathing, and feeding.
Cord blood, cord tissue and post birth options
Cord blood composition and collection basics
Cord blood left in the placenta and cord is rich in Cord blood stem cells, cells that can rebuild blood and immune systems. Collection occurs after clamping and cutting, and delayed clamping reduces the remaining volume, so timing choices affect collection yield. Families planning storage or donation benefit from talking with the care team before labor to align timing and logistics.
Clinical uses and realistic expectations
Stored units can support transplants for blood cancers, marrow failure, and immune deficiencies. Many families ask whether storage should be private or public. Public cord blood banking contributes to registries that help many patients at no cost to the donating family, while Private cord blood banking reserves the unit for your family for a fee. Use in future personal scenarios is possible, though uncommon in the general population. Some parents also ask how this compares with marrow donation, resources often discuss Cord blood vs bone marrow transplant to explain differences in matching and availability.
Cord tissue and wharton’s jelly as cell sources
The cord’s connective tissue contains mesenchymal cells with promising laboratory properties. Clinical use outside trials is still limited. If you consider storage, balance cost with the current state of evidence.
You may be weighing what does the umbilical cord do after your baby is born. It can be a source for donation, for research, or simply a part of family rituals. All are valid choices when safety is kept front and center.
Common variations and cord complications
Nuchal cord, true knots and cord entanglement
Loops around the neck are common. Most are loose and do not change care. Cord knots that tighten are rare but can compress vessels. Ultrasound can sometimes suggest a knot or multiple loops, however, monitoring during labor remains the main tool to see how the baby is coping.
Velamentous insertion, vasa previa and marginal insertion
When vessels run through membranes without jelly, as in Velamentous cord insertion, they lose protection. Very rarely, vessels cross the cervix, called Vasa previa, which can bleed if membranes tear during labor. Prenatal diagnosis with targeted ultrasound often leads to planned birth before labor, usually by cesarean, to keep the baby safe. A Marginal cord insertion near the placental edge usually means closer watch of growth and Dopplers.
Single umbilical artery and congenital anomalies
Sometimes, there is one artery rather than two. This can associate with structural differences or growth issues. If seen on imaging, teams look carefully at the heart, kidneys, and growth, and may discuss genetic testing.
Short cord, long cord and abnormal coiling outcomes
Extremely short cords can tug, which may complicate the second stage. Extremely long cords can loop or prolapse. Very high or very low coiling has been linked with growth restriction in some studies, so it often prompts closer follow up.
You might still ask, what does the umbilical cord do when these variations are present. The same basic job, deliver and remove, though the margin for compression can be smaller, which is why surveillance becomes the safety net.
Diagnosis and monitoring of cord health
Prenatal ultrasound and visualization
Anatomy scans look for vessel number and insertion, and sometimes show loops or suspected knots. Not every issue shows up on a scan, so findings are paired with growth curves and heart rate patterns. If you have copies of reports, the phrases Ultrasound assessment of cord insertion and vessel count are standard entries.
Doppler velocimetry and flow assessment
Blood flow can be measured noninvasively. Doppler ultrasound of the umbilical cord yields indices that reflect placental resistance. When growth is slow, Umbilical artery Doppler in fetal growth restriction becomes especially informative. Absent or reversed flow during the resting part of the heartbeat is a red flag that usually leads to more frequent visits and discussions about timing of delivery.
If you are asking what does the umbilical cord do on an ultrasound, the answer is visual and numeric. It shows patterns of flow that correlate with how easily blood moves between baby and placenta.
Intrapartum monitoring and ctg patterns
During labor, variable decelerations suggest intermittent cord compression. Care teams reposition the parent, pause labor stimulating medicines, consider fluids or amnioinfusion, and move to delivery if the tracing does not improve.
Cord blood gases and placental pathology
Right after birth, cord samples can quantify pH and lactate. When results are abnormal, teams often increase newborn observation, and may request a placental exam to learn more and to plan for future pregnancies.
Management when the cord is compromised
Immediate intrapartum maneuvers
When tracings suggest compression, the first steps are simple, change position to relieve pressure, pause oxytocin, give fluids, provide oxygen, consider amnioinfusion if membranes are ruptured. For a visible loop at birth, a gentle reduction is attempted. In the case of cord prolapse, where the cord slips ahead of the baby, hands relieve pressure right away and birth is expedited.
Delivery planning for known cord abnormalities
Conditions like Vasa previa often lead to scheduled cesarean before labor. Others, such as marked velamentous insertion without previa, may call for individualized timing with frequent surveillance. Plans are shaped with obstetrics, anesthesia, and neonatology in the room or on call.
Neonatal resuscitation and follow up after compromise
If a baby shows low vigor at birth or if cord gases are very abnormal, the team focuses on breathing, warmth, and circulation. Some infants meet criteria for therapeutic hypothermia, a time sensitive therapy for significant hypoxic injury. Follow up can include developmental checks and early intervention if needed.
You may quietly ask, what does the umbilical cord do when things go sideways. It still tells a story, through tracings, Dopplers, and gases, that guides prompt, steady care.
Umbilical cord stump care after birth
Normal stump drying and separation timeline
The stump dries and darkens in the first days, then drops away, often near the end of the first week, sometimes up to three weeks. A small spot of blood on the diaper is common when the stump separates.
Signs of infection or abnormal healing
Call your care team for fever, redness that spreads, warmth, swelling, a foul smell or pus like discharge, or if the stump has not fallen by three weeks. The medical term for infection is Omphalitis, and while uncommon, it needs prompt attention.
Practical parent tips for stump care
Keep the area clean and dry. Fold the diaper below the stump so it is not irritated. Use sponge baths until it falls off. Gentle washing with water is enough unless your clinician advises otherwise. Never pull on it. For quick reference, see Cord stump care checklists provided by many hospitals and public health sites. Parents often ask about timing, the phrase Cord separation timing after birth is sometimes noted in discharge instructions.
You may also find yourself wondering what does the umbilical cord do once it is a stump. At that point, its job is done, and the small remnant is simply healing tissue.
Cultural, ethical and practical considerations
Some families keep a small piece of the dried cord, some plant the placenta with a tree, others prefer simple disposal. Discuss your wishes early so staff can help you do this safely and respectfully. On storage choices, Cord blood banking brings up cost, logistics, and personal values. Public cord blood banking helps many and does not reserve the unit, Private cord blood banking holds it for your family but with fees. There is no single right answer, your context and medical history shape the decision.
Hospitals also set policies, who can cut the cord, how donation is coordinated, what signatures are needed. If you plan delayed clamping and donation, raise this before labor, that way the collection team can prepare.
Key takeaways
- The cord is the baby’s lifeline during pregnancy, it delivers oxygen and nutrients, and removes carbon dioxide and waste. If someone asks what does the umbilical cord do, that is the simplest, most accurate answer.
- Structure protects function, vessels, coiling, and Wharton’s jelly keep flow going even with movement and contractions.
- Timing matters at birth, delayed clamping often boosts early blood volume and iron, immediate clamping still has a place when quick intervention is needed.
- Scans and Dopplers are practical tools, they show how blood moves through the cord and placenta, and they guide decisions about monitoring and delivery timing.
- Variations like nuchal loops, velamentous insertion, and Vasa previa are managed with tailored plans that center safety for parent and baby.
- Stump care is simple, keep it clean and dry, watch for redness, swelling, or foul discharge, and let it fall on its own.
If questions linger, especially around specialized findings or birth planning, talk with your clinician. For ongoing tips that fit your family’s context, you can download the application Heloa for personalized advice and free child health questionnaires.
Questions Parents Ask
Is the umbilical cord attached to the belly button?
Yes. The cord connects to the baby’s abdomen at the spot that becomes the belly button (navel). After birth the cord is clamped and cut; the small stump left on the abdomen dries and falls off over days to a few weeks, leaving the healed belly button. Rassurez‑vous — cutting is painless for the newborn and the navel is simply the scar of that connection. You can keep care gentle and watch for redness, pus, spreading warmth or fever, and contact your care team if any of those appear.
What happens to the umbilical vessels and cord tissue after birth?
Once the cord is clamped or circulation shifts when the baby breathes, blood flow through the vessels stops and they close down. The soft gel and vessels in the external stump dry and separate from the skin; internally the former vessels gradually fibrose and become ligament‑like structures (for example, the umbilical vein becomes the round ligament of the liver). In short: the cord stops working, the visible stump falls away, and the remaining tissues remodel into harmless internal remnants. If you’re curious about donation or storage, those steps are arranged before or right after birth since timing affects how much cord blood can be collected.

Further reading:
- Anatomy, Abdomen and Pelvis: Umbilical Cord – NCBI: https://www.ncbi.nlm.nih.gov/books/NBK557389/
- Umbilical cord care: Do’s and don’ts for parents: https://www.mayoclinic.org/healthy-lifestyle/infant-and-toddler-health/in-depth/umbilical-cord/art-20048250
- Blood Circulation in the Fetus and Newborn – UR Medicine: https://www.urmc.rochester.edu/encyclopedia/content?ContentTypeID=90&ContentID=P02362