Heartburn during pregnancy—a phrase that sparks recognition, perhaps even a twinge of frustration, for many expecting parents. The sensation can strike suddenly, a burning ache creeping behind the breastbone after a meal, or a persistent discomfort that lingers and disrupts precious sleep. Given the excitement and anxiety that often accompany pregnancy, few parents anticipate just how dramatically their digestive comfort might shift. Is every meal destined to end in discomfort? Will a simple orange juice or late-night treat be forever banished from the menu? Heartburn during pregnancy is not only widespread, but also shaped by unique physiological changes. Unpacking the medical science behind it brings clarity, relief, and empowers families to reclaim comfort with concrete, research-based strategies.
What Really Happens: The Science of Heartburn During Pregnancy
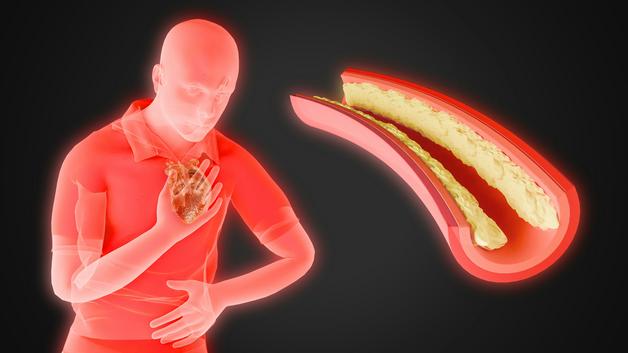
If you’re curious—why now?—the answer lies in the extraordinary hormonal choreography of pregnancy. High levels of progesterone (sometimes called the “relaxing hormone”) soften smooth muscle tissue throughout your body. While this supports a growing uterus, it also relaxes the lower esophageal sphincter, that one-way valve separating the stomach from the esophagus. The result? Acidic content from the stomach can move upward—what’s called acid reflux—causing heartburn during pregnancy.
This is not just a matter of mild warmth. The passage of acid triggers a cascade of symptoms: a fiery sensation in the middle of your chest, regurgitation of sour fluid, and frequent burping or bloating after meals. Some experience a bitter taste at the back of the throat, others describe difficulty falling asleep because of the persistent burning. It’s important to distinguish heartburn from simple indigestion (which is more about heaviness and bloating) and from morning sickness, which usually involves queasiness without the acid burn.
The growing uterus contributes a physical layer to this discomfort. As your pregnancy advances into the second and third trimesters, the expanding uterus presses upward against the stomach, increasing the risk of acid movement into the esophagus. If you have a sensitive digestive tract or experience rapid weight gain, symptoms can be even more pronounced.
Heartburn and Acid Reflux: Are They the Same?
The two terms often swirl together—but technically, acid reflux is the process, and heartburn during pregnancy is the symptom that announces it. Acid reflux refers to the movement of gastric acid into the esophagus, while heartburn describes that burning, sometimes searing, sensation it produces. During pregnancy, these intertwined phenomena can feel like an uninvited double act, amplified by hormonal and anatomical shifts.
Notice patterns: the discomfort may heighten when lying down, after eating, or during physical movements like bending. Regurgitation—where actual acid rises into the mouth—adds to the distress, further distinguishing heartburn from routine indigestion.
What Makes Heartburn Worse? Dietary and Lifestyle Triggers
You may wonder if there’s a conspiracy against your favorite foods. Certain triggers loom large for heartburn during pregnancy:
- Fried, fatty, and greasy foods
- Spicy dishes or pungent condiments
- Citrus fruits, tomatoes, and other acidic foods
- Chocolate and mint (both can further relax the esophageal valve)
- Caffeinated beverages, sodas, and carbonated drinks
Large meals, late-night snacking, and drinking copious fluids during meals—all of these behaviors stretch the stomach, boosting pressure on that delicate esophageal barrier. Wearing tight waistbands or reclining too soon after eating? Both risk tipping the scales further. It’s not only about food: some individuals with gastric hypersensitivity are simply more vulnerable, especially if they experience rapid weight changes during the pregnancy journey.
Dietary Adaptations: Building a Soothing Eating Plan
Nutrition doesn’t need to become a battleground. With thoughtful adaptation, parents can ease heartburn during pregnancy and reclaim mealtime comfort.
- Prioritize gentle, non-acidic vegetables such as carrots, zucchini, or pumpkin. Choose well-tolerated starches—potatoes, for instance, or wholegrain rice.
- Enjoy fruits with low acidity: bananas and pears top the list.
- Favor milder, cooked cheese from goat or sheep’s milk to minimize irritation.
- A yogurt (non-sweetened and rich in probiotics) can help line the stomach and promote calm digestion.
- Opt for natural, bicarbonate-rich mineral water—this may help neutralize excess acid.
Cooking methods shape outcomes: avoid frying and instead try steaming, gentle roasting, or baking. Adopt a schedule of smaller, more frequent meals—four to six per day is a reasonable target. Chew thoroughly and take your time; this helps limit abrupt pressure surges in the stomach and eases the work your digestive system must do.
Try to hydrate between meals, not during. And if you’re tempted to lie down after dinner, try waiting two hours or more—gravity is often your ally against heartburn during pregnancy. Plan an early, light dinner if possible to set yourself up for more restful nights.
Posture, Routine, and Everyday Habits for Comfort
Here’s where practical tweaks yield real rewards. Small daily shifts accumulate to help minimize the sting of heartburn during pregnancy:
- Remain upright after meals. Whether it’s a gentle walk or simply sitting up, avoiding reclining gives gravity a chance to help keep acid where it belongs.
- For sleep, consider elevating the head of your bed by 6–8 inches. A wedge pillow or sturdy blocks beneath bed legs can angle your body so acid is less likely to travel upward.
- Loose, comfortable clothing—particularly around the waistline—avoids compressing the stomach and reduces episodes of reflux.
- Introduce calming rituals: prenatal yoga, breathing, or focused relaxation can soothe both mind and digestive tract. High stress is linked to increased reflux episodes, while mindful stress management shows tangible relief.
Build healthy rhythms—a short walk after meals, slow eating, dividing food into several portions throughout the day—each step supports better digestion and fewer relapses of heartburn during pregnancy.
When Is It Time to Talk to a Healthcare Provider?
While heartburn during pregnancy is most often a temporary inconvenience, there are important warning signs. Contact a healthcare professional if you notice:
- Persistent or intensifying heartburn despite attempts to adapt diet and habits
- Sharp pain radiating toward the back or arms, or chest pain that doesn’t resolve
- Recurrent vomiting, marked appetite reduction, or unexplained weight loss
- Fever, severe headaches, or gastrointestinal bleeding (such as vomiting blood or passing black stools)
- Difficulty swallowing or frequent nighttime awakening due to heartburn
Prompt attention to these signs can ensure effective and safe relief while ruling out other rare, but more serious, medical conditions.
Natural Remedies: Safe Soothing Measures
Natural comfort holds strong appeal, especially when pregnancy heightens concern for medications. Several gentle strategies for heartburn during pregnancy have research backing:
- Certain herbal teas, such as those with lemon balm, can calm digestion, but always confirm safety with a healthcare provider.
- Marshmallow root and licorice root, in forms approved for pregnancy, may offer a protective lining for the esophagus.
- Fresh ginger, sliced or grated and steeped in hot water, can calm both nausea and mild reflux if used in moderation.
- Avoid essential oils (concentrated plant extracts) in pregnancy; their safety has not been confirmed.
- Low-fat yogurt and water naturally rich in bicarbonate are safe options for most parents.
Some consider aloe vera (labeled as a food supplement), but this requires professional oversight due to potential risks. Never combine multiple remedies or herbal supplements without guidance—a cautious, informed approach is always safest for both parent and growing baby.
Medications: What’s Safe When Natural Solutions Aren’t Enough?
If lifestyle adaptation and natural remedies fall short, some pharmaceutical options are deemed safe for heartburn during pregnancy:
- Local antacids containing sodium alginate or bicarbonate
- Formulations containing calcium carbonate (commonly found in chewable tablets like Tums) or certain magnesium-based antacids
- In specified situations, a healthcare provider may prescribe a proton pump inhibitor (PPI) such as omeprazole, which offers powerful acid suppression and is generally considered safe for use during pregnancy
Never self-medicate or add any over-the-counter product without expert advice. Drug interactions and rare side effects can arise—professional guidance ensures both optimal safety and symptom control.
Heartburn During Pregnancy: Risks and Myths
Reassurance counts: heartburn during pregnancy itself does not threaten your baby’s direct well-being. Discomfort can certainly impede sleep or affect appetite, and in rare, severe cases, persistent vomiting might impact nutrient intake. Still, these situations are the exception, not the rule.
Some persistent myths deserve dispelling: food sensitivities differ between individuals—what causes distress for one mother need not be problematic for another. Adaptation, not blanket avoidance, proves most helpful. Recognize that most heartburn resolves shortly after birth, though a few may experience lingering sensitivity for a short time postpartum.
Key Takeaways
- Heartburn during pregnancy is common, intensely shaped by hormonal and anatomical changes—both acid reflux (movement) and heartburn (symptom) matter.
- Smart dietary choices (gentle vegetables, non-acidic fruits, smaller meals) and practical strategies (upright posture, bed elevation, calm routines) reduce discomfort in most cases.
- Evidence-based natural remedies or appropriate medications may prove useful; always consult a healthcare provider before starting anything new.
- Seek medical assessment for severe, persistent, or unusual symptoms—timely expertise ensures comfort and guards against rare complications.
- Reliable resources and real-world support are always at hand. To access personalized advice, meal tracking, and child health questionnaires, parents can download the Heloa application, an accessible and science-informed companion to navigate pregnancy and early parenting—because with expert information and supportive strategies, comfort and peace of mind are truly within reach.
Questions Parents Ask
Can heartburn during pregnancy harm my baby?
Feeling heartburn during pregnancy is understandably worrying, but rest assured: heartburn itself does not pose a direct risk to your baby. This symptom results mainly from hormonal changes and the pressure of the growing uterus, not from anything dangerous to your developing child. In rare cases, if severe indigestion leads to ongoing vomiting or significant difficulty eating, it’s important to reach out to a health professional for advice and support to ensure you are both well-supported. In most situations, heartburn is simply part of the body’s adaptation to pregnancy.
When does heartburn start in pregnancy and how long does it last?
Heartburn can begin at any stage of pregnancy, but many parents notice it becoming more frequent or intense during the second and third trimesters. This increase is often linked to rising hormone levels and the uterus putting added pressure on the stomach. For many, the discomfort eases shortly after the baby is born as the body’s natural balance returns. While it can be uncomfortable during pregnancy, it’s generally temporary and manageable with gentle adjustments to daily routine or diet.
Are there any natural drinks that can help relieve heartburn during pregnancy?
Yes, some natural drinks may provide comfort if you’re experiencing heartburn during pregnancy. Many parents find that sipping cool water, especially water rich in natural bicarbonates, can neutralize acid and bring gentle relief. Herbal teas such as those made from chamomile or lemon balm are also commonly used, but it’s always best to check with your healthcare provider before trying new herbal options during pregnancy. Mild, non-acidic smoothies—using ingredients like banana or oats—can sometimes help soothe the stomach as well. Each body reacts differently, so listen closely to your own comfort and feel free to consult your care professional for tailored guidance.
Further reading: