Pregnancy launches the body into a whirlwind of transformation—sometimes subtle, sometimes seismic. For many parents, uncertainty abounds. Why does fatigue set in with a vengeance, or why does a sense of euphoria suddenly give way to tears? The answer often lies with pregnancy hormones. These chemical messengers shape your experience from the moment fertilization occurs, guiding development, well-being, and adaptation. Nausea, mood swings, glowing skin, and even those mysterious food cravings all find their root in this intricate hormonal ballet. This exploration will clarify why these hormonal surges happen, what their physical and emotional impacts are, and how their ebb and flow supports both you and your baby. If you’re seeking insight, reassurance, or simply a scientific explanation for the rollercoaster ride, you’re in the right place. Here’s a tour through the fascinating world of pregnancy hormones—bursting with practical advice, fresh perspectives, and science-backed details to help parents feel informed, resilient, and empowered.
The Symphonic Surge: An Overview of Pregnancy Hormones
Pregnancy hormones ignite an astonishing cascade of changes from the first days after conception. The process is anything but monotonous. Human chorionic gonadotropin (hCG) takes the stage first, secreted by the developing placenta to signal pregnancy. Progesterone soon follows, calming uterine muscles and creating a nurturing environment for the embryo. Estrogen, rising in concert, amplifies blood supply and prepares tissues for growth. And—almost backstage—human placental lactogen (hPL) alters maternal metabolism to favor the baby’s needs.
What governs these hormonal spikes and dips? A network of organs: the ovaries, the evolving placenta, the pituitary gland—the latter unleashing prolactin to foster milk production and synchronize with oxytocin, the conductor of labor and postpartum bonding. Even the fetal adrenal glands contribute, supplying precursors vital for ongoing pregnancy.
Each hormone acts as both soloist and member of an ensemble, driving physical changes (think: breast sensitivity, fatigue, altered digestion) and emotional fluctuations. Wonder why a simple scent suddenly triggers nausea? The answer often returns to this unpredictable, yet beautifully orchestrated, hormonal interplay.
From Period to Pregnancy: The Hormonal Prelude
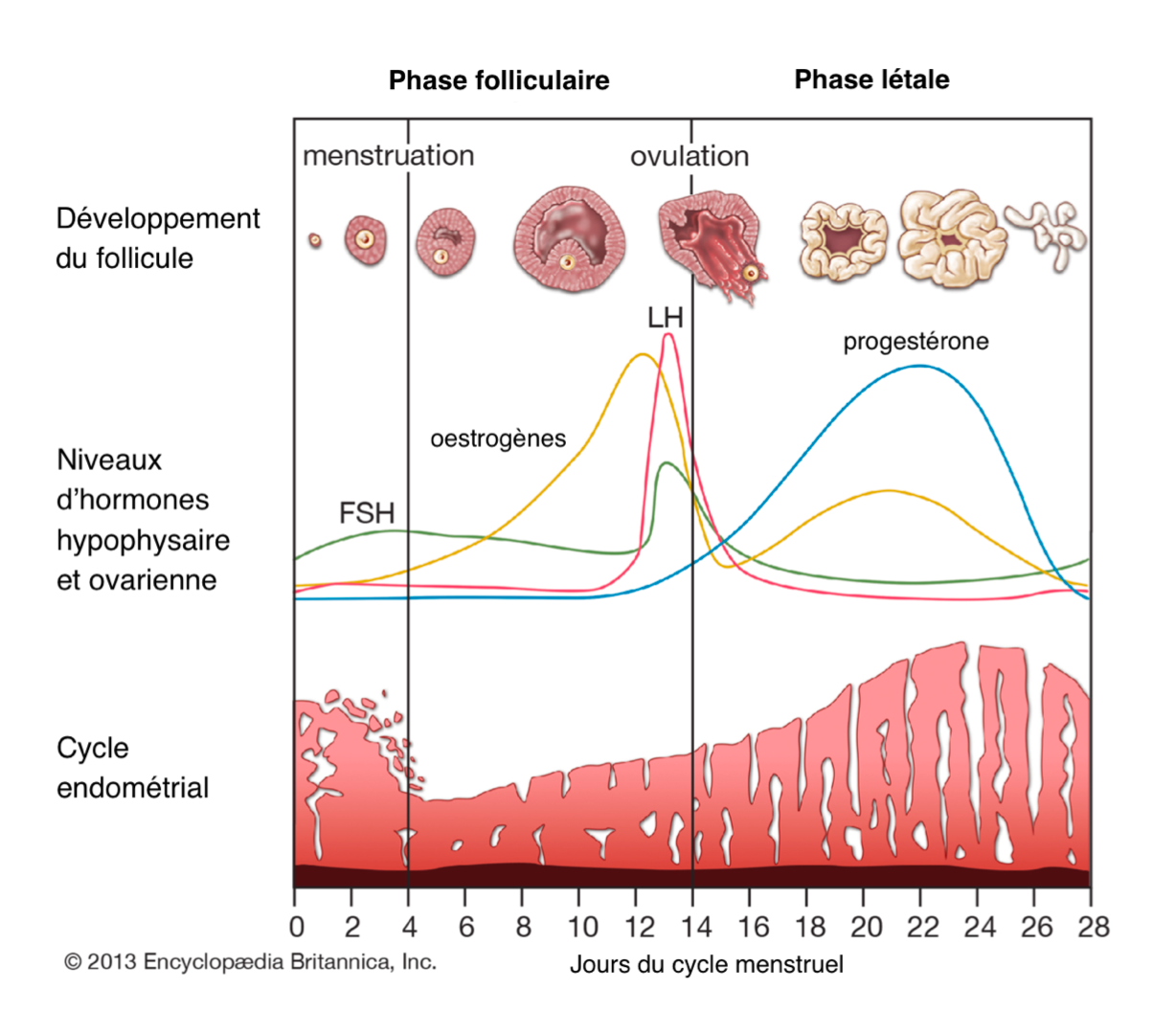
Before pregnancy hormones dominate the scene, ovulation and the menstrual cycle set the context. The pituitary gland’s follicle-stimulating hormone (FSH) directs ovarian follicles to mature, while estrogen orchestrates the uterine lining’s preparation. Estrogen’s peak incites a surge in luteinizing hormone (LH), triggering ovulation. If fertilization happens, the corpus luteum (what remains of the follicle) churns out progesterone. This shift prevents menstruation and ensures optimal support for early gestation.
Curious about timing? Each cycle typically spans about 28 days, but real life often strays from textbook predictability. A sudden alteration or missed period can stir anxiety—often the very first hint that pregnancy hormones are rewriting the script.
Key Pregnancy Hormones and Their Functions
Human Chorionic Gonadotropin (hCG)
Often recognized as the earliest signal of pregnancy, hCG is secreted by the trophoblast (outer layer of the embryo) within days of implantation. Its job? To ensure the corpus luteum keeps producing progesterone, warding off uterine contractions and securing the freshly implanted embryo. This surge is why over-the-counter pregnancy tests work—but it’s also what’s behind the classic wave of morning sickness many parents experience. Persistently abnormal hCG levels may alert medical professionals to complications, prompting timely intervention—a potent demonstration of the hormone’s significance.
Progesterone
Without progesterone, pregnancy would falter. Secreted initially by the corpus luteum and later by the placenta, this hormone steadfastly supports the uterine lining, relaxes uterine muscles, and ramps up immune protection to shelter the embryo. Its far-reaching effects ripple throughout your system: interrupted digestion (often causing constipation), breast changes, pervasive tiredness, and, yes, those unpredictable mood swings. Progesterone’s dominance even suspends menstruation until the end of pregnancy.
Estrogens (Estradiol, Estriol, Estrone)
Estrogen is not a single entity but a collection—estradiol, estriol, estrone—originating first from the ovaries and then mainly from the placenta. Their roles are extensive: stimulating uterine growth, boosting circulatory volume, coordinating tissue adaptation for the future demands of birth and lactation. Closer to labor, rising estrogen sensitizes the uterus to oxytocin, orchestrating the onset of regular contractions. A fascinating twist: estrogen also affects skin tone and elasticity (hello, “pregnancy glow” and linea nigra).
Human Placental Lactogen (hPL)
As pregnancy advances, the human placental lactogen steadily increases, preparing breast tissues for lactation and shifting maternal metabolism to prioritize fetal energy needs. By ramping up insulin resistance, hPL ensures a larger share of circulating glucose reaches the developing fetus. However, this can sometimes tip the scales toward gestational diabetes—one reason for tailored glucose screening during pregnancy.
Relaxin, Oxytocin, and Prolactin
- Relaxin unleashes flexibility—both helpful and occasionally inconvenient. By softening pelvic ligaments and the cervix, it paves the way for birth but may also explain joint instability or balance wobbliness as pregnancy progresses.
- Oxytocin, though relatively inconspicuous for months, leaps into action near labor’s start, fueling strong uterine contractions, facilitating milk ejection, and bolstering maternal-infant bonding.
- Prolactin steadily rises, promoting glandular growth in the breasts and setting the stage for milk production after birth. As a bonus, prolactin often suppresses ovulation, lengthening the gap before menstrual periods resume—especially if breastfeeding.
Beyond the Basics: Other Hormones of Interest
- Corticotropin-releasing hormone (CRH): A key player in labor timing and fetal readiness.
- Thyroid hormones (T3, T4): Support metabolic demands and neurological maturation.
- Androgens: Minor, but pivotal for specific fetal tissues.
- Beta-endorphins: Nature’s pain relief as labor nears.
- ACTH and Cortisol: Fine-tune stress responses and aid lung maturation.
- Placental growth factor (PlGF): Nurtures robust placental blood vessels for ideal nutrient exchange.
Hormones on the Move: Change Over Pregnancy’s Course
First Trimester
The story opens with a leap in hCG, marking the establishment of pregnancy. Progesterone and estrogen, mainly from the corpus luteum, dominate—ushering in early fatigue, noticeable breast changes, queasiness, and sometimes tearful moments at surprising triggers.
Second Trimester
Here, the hormonal tempo shifts. hCG levels stabilize, but progesterone, estrogen, and hPL ascend steadily, sustaining fetal growth, supercharging the supply of nutrients, and accounting for renewed energy and complexion changes that parents may notice around mid-pregnancy.
Third Trimester
The final act is dynamic—surges of estrogen, progesterone, prolactin, relaxin, and oxytocin orchestrate readiness for birth. CRH and cortisol synchronize fetal organ maturation, and Braxton Hicks contractions may introduce early “practice” for labor. Near term, an intriguing pivot: progesterone tapers, estrogen peaks—priming the uterus for coordinated, effective contractions.
Physical, Emotional, and Fetal Impact
Bodily Changes and Physical Symptoms
It’s impossible to ignore the physical effects of shifting pregnancy hormones. Some parents report persistent nausea, pronounced breast swelling, or fresh skin pigmentation. Others notice changes in hair texture, fluid retention, or even mild joint aches linked to relaxin. Digestive complaints—constipation, heartburn—are frequent visitors, explained by both direct hormonal action and pressure from the growing uterus.
Emotional and Psychological Dimensions
Mood swings during pregnancy are not merely anecdotal. Scientific analysis attributes much of this lability to the interplay of progesterone and estrogen, shifting neurotransmitter balance in the brain. Fluctuating between joy, frustration, and tears—all without obvious warning—can feel bewildering, yet it’s a direct result of biological adaptation. Opening up about these shifts, whether with a partner, friend, or clinician, can make a world of difference.
Supporting Your Baby’s Development
Hormones such as estrogen and placental growth factor curate the fetal environment, supporting everything from brain formation to oxygen delivery. Their effects reach well beyond pregnancy: for instance, optimal thyroid hormone levels are integral for cognitive development, while cortisol assists in maturing the lungs for that critical first breath.
Monitoring and Managing Pregnancy Hormones: Practical Approaches
How and Why Hormones Are Measured
A medical practitioner may recommend various blood or urine tests to gauge pregnancy hormone levels. hCG is routinely checked in early pregnancy (especially with bleeding or uncertain dates), while estriol and placental growth factor are sometimes measured to assess placental health. For some, hormone monitoring can unmask risks such as preeclampsia or growth restriction. If laboratory values fall outside expectations, additional guidance or interventions may be offered to help preserve the well-being of both parent and baby.
Hormone-Related Complications
- Low progesterone can predispose to early pregnancy loss or preterm birth.
- Excess hPL may disrupt glucose control, ushering in gestational diabetes.
- Thyroid imbalance and altered androgen levels can leave subtle—but important—effects on both parent and baby.
Unusual findings usually prompt additional, targeted care; reassurance and action go hand in hand here.
Nurturing Hormonal and Emotional Health
Nutrition, Lifestyle, and Self-Care
Looking to support a balanced surge of pregnancy hormones? A diet abundant in fresh vegetables, whole grains, high-quality proteins, healthy fats, and plenty of water supplies the essential building blocks for fetal and hormonal well-being. Moderate exercise—pausing for symptoms, of course—helps regulate blood sugar, energy, and mood fluctuations. Sleep, stress-relief practices, and gentle physical routines are equally valuable (think: prenatal yoga, peaceful walks, mindful breathing).
Responding to Change with Compassion
Each parent’s journey is unique, punctuated by both easy days and challenging moments. Setting boundaries, asking for help where needed, and making room for rest or reflection are worthy priorities. If periods of sadness, anxiety, or disconnection emerge and persist, do not hesitate to reach out—a listening professional can offer both support and potential solutions without judgment.
The Postpartum Hormonal Shift
Once your baby is born, estrogen and progesterone tumble rapidly. Prolactin and oxytocin, meanwhile, surge to facilitate breastfeeding and foster emotional connection. This sudden transition often triggers the “baby blues”—a short-lived window of mood fluctuation. Simple routines, rest, hydration, and emotional support accelerate recovery. For those who don’t breastfeed, menstruation may resume after four to six weeks; breastfeeding can delay its return.
Medical Advances and Monitoring: Spotlight on Interventions
When Extra Hormonal Support Is Considered
Some pregnancies benefit from additional hormone support—progestins can shore up early gestational stability, while thyroid supplementation addresses metabolic or developmental concerns. Continued hormone measurement can swiftly highlight concerns like gestational diabetes, preeclampsia, or growth restriction—enabling proactive, rather than reactive, management.
More Than Discomfort: Managing Hormonal Symptoms
While a certain degree of discomfort is to be expected, parents are not powerless. Small, practical adjustments—eating smaller, frequent meals for nausea, gentle movement for mood, prioritizing rest, and leaning on loved ones for help—allow room for adaptation and comfort. Attention to self-care and mindfulness builds resilience, both before and after birth.
Key Takeaways
- Pregnancy hormones serve as the unseen architects of gestation, orchestrating adjustments in every organ system and supporting baby’s development at every turn.
- Every physical, emotional, and metabolic change has a hormonal foundation—understanding this dynamic can transform worry into empowerment.
- From hCG to progesterone, estrogen to hPL, these messengers act in symphony—each phase of pregnancy offers new rhythms, possibilities, and challenges.
- Monitoring hormone levels informs individualized care for parent and baby, allowing minor issues to be addressed before they escalate.
- Evidence-based self-care—nutritious diet, gentle activity, consistent hydration, and timely support—can soften discomfort and nurture emotional health.
- For parents seeking guidance or customized resources, consider accessing support through your healthcare provider, and download the Heloa app for personalized tips and free child health questionnaires.
Pregnancy hormones: they shape, test, and surprise—yet underpin one of life’s most extraordinary journeys. Every parent’s path is different, but with information and the right support, navigating these changes becomes a little clearer.
Questions Parents Ask
Can pregnancy hormones affect sleep patterns?
It’s very common for changes in hormone levels during pregnancy—especially progesterone and estrogen—to impact sleep. Many parents feel unusually tired in the first trimester, and later, difficulty falling or staying asleep may appear. Nighttime awakenings, vivid dreams, or even restlessness can all be linked to hormonal shifts. These changes are natural and reflect the body’s adaptation to pregnancy. You can try relaxation techniques, gentle movement, and a soothing bedtime routine to improve comfort. If you’re having persistent trouble sleeping, don’t hesitate to talk to a healthcare professional—support is always possible.
How soon after conception do pregnancy hormones start to rise?
Human chorionic gonadotropin (hCG) begins to increase just days after fertilization, even before a missed period. This early rise in hCG allows pregnancy tests to detect a possible pregnancy typically one to two weeks after conception. Progesterone and estrogen also climb quickly to create an optimal environment for the developing embryo. For many, the first signs—like tiredness or breast sensitivity—appear soon after these hormone levels increase. Every parent is different, so onset and degree of symptoms can vary.
Can pregnancy hormones cause headaches?
Yes, changes in estrogen and progesterone levels can sometimes lead to headaches in pregnancy, especially in the first trimester. These headaches are a normal response to the rapid hormonal changes and increased blood flow occurring in the body. Try to rest, stay hydrated, and seek out calm, low-light environments when needed. If headaches become intense or ongoing, it is wise to consult with your healthcare provider for personalized advice and reassurance.
Further reading:









