Welcoming a new baby through a cesarean delivery brings both immense joy and a cascade of questions. How long will it take to feel strong again? Should discomfort around the incision be this persistent? Is it normal to feel overwhelmed—both physically and emotionally—when caring for a tiny newborn while also healing from surgery? Postpartum rehabilitation after cesarean is a unique journey, with each parent weaving together rest, gentle activity, and emotional adaptation at their own pace. Many discover that the pathway to recovery is not linear but marked by small triumphs and unexpected challenges. Addressing pain, restoring mobility, eating well, and building confidence in daily care: these are the stepping stones for a smoother transition. Science offers clarity—rehabilitation isn’t just about wound care, but a symphony of body, mind, and connection. Let’s explore how parents can structure recovery, minimize risks, and embrace autonomy, with medical expertise lighting the way.
Understanding the Cesarean Delivery Experience
A cesarean section—sometimes decided before labor begins, other times determined after challenges arise—transforms the anticipated birth plan into a surgical moment. Regional anesthesia keeps most mothers awake, feeling gentle pressure but not pain. The reasons? Sometimes it’s fetal distress, an obstructed labor, previous surgical scars, or the position of the baby. Hospital stays, normally ranging from one to three days, focus on close monitoring: checking blood pressure, monitoring the incision, and ensuring stable postpartum recovery. No two stories are alike; some parents feel immediate relief, others a sense of loss or frustration. Scientific studies reveal that medicalizing birth through surgery layers additional factors on hormonal recovery and postnatal mental health, making family and professional support even more impactful.
The Phases of Physical and Emotional Recovery
Early Days: Navigating Pain, Fatigue, and Healing
Immediately after cesarean delivery, the body rallies its resources. Incision pain, swelling in legs or feet, sometimes even stubborn constipation—these are just the outward signs of deep healing underway. Movement may feel daunting; yet, even sitting up or taking a few steps (with help) encourages healthy circulation and lowers clot risk. Pain relief, typically acetaminophen or ibuprofen, may be supplemented with other medications, individualized for each situation. A pressurized abdominal binder can provide a sense of security for those first hesitant walks. While physical hurdles are real, emotional responses often surprise: relief, joy, anxiety, even tearful moments are common as hormones like oxytocin and estrogen shift dramatically in the days following surgery.
Weeks One to Six: Gradual Return of Strength and Routine
Pain usually subsides incrementally, but some discomfort may linger on exertion. Light activities—feeding, gentle walks, or short forays outside—help restore stamina without overtaxing healing tissue. Scar tissue management becomes relevant once the incision seals, as gentle massage and observation limit excessive adhesions. Simple daily habits matter enormously—think routine handwashing and incision checks for redness or pus, preventing the risk of infection. Pelvic floor and gentle abdominal exercises, initiated with medical guidance, can safely reawaken muscle tone and support the lower back.
Months Six and Beyond: Regaining Core Strength, Confidence, and Mobility
By six weeks or later, many resume low-impact exercise. Yet, thresholds for safe activity fluctuate—each parent’s timeline is unique, influenced by sleep, nutrition, and the demands of baby care. Postpartum rehabilitation after cesarean becomes particularly targeted now: specialized physiotherapy for abdominal muscle separation (diastasis recti), deep core engagement, and pelvic floor resilience. Ignoring muscle recovery can set the stage for persistent pain, postural issues, or even pelvic organ prolapse. Scientific literature consistently underscores the benefits of rehabilitation: improved mobility, faster scar healing, and enhanced emotional adaptation.
The Science and Practice of Rehabilitation: Perineal and Abdominal Focus
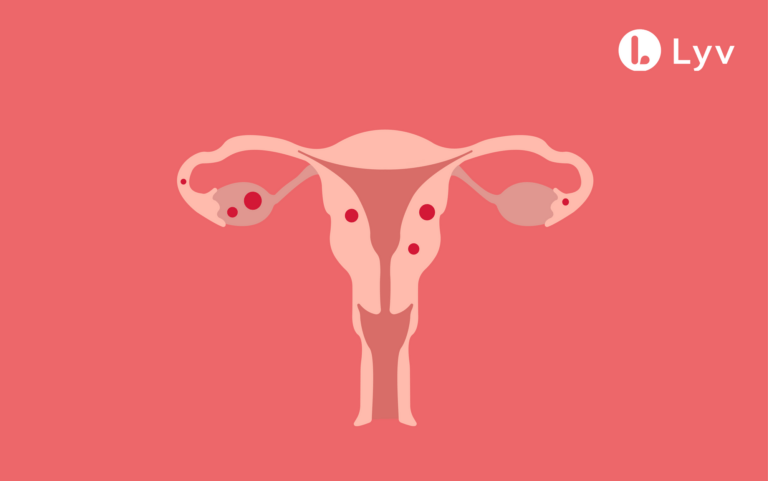
Why Pelvic Floor Recovery Matters—even After Cesarean
It’s a misconception that only vaginal births strain the pelvic floor. The act of pregnancy itself—the pressure of the growing uterus and hormonal softening of ligaments—challenges the perineal muscles. Even absent a vaginal delivery, contractions, or hours spent pushing, can stress pelvic support structures. Pelvic floor dysfunction, often manifesting as incontinence, discomfort during intimacy, or a sensation of heaviness, may quietly persist unless addressed. Delicate and precise exercises (think Kegel exercises, pelvic tilts) restore muscle tone and improve bladder and bowel control. In some scenarios, technology-enhanced options like electrical stimulation or biofeedback offer tailored support, informed by emerging clinical evidence.
Abdominal Rehabilitation: More Than Cosmetic Recovery
Visible changes—softness around the belly, discomfort when rising—reflect more than just lingering pregnancy weight. The abdominal wall, stretched for months, sometimes remains separated at the midline (diastasis recti). Here, poorly structured exercise or premature high-intensity workouts can deepen the gap or induce back pain. Instead, focused core exercises (guided by pelvic health specialists or physiotherapists) steadily rebuild integrity. Postpartum rehabilitation after cesarean leverages both physical therapy and self-monitored routines to safeguard posture, prevent hernias, and promote functional strength needed for lifting and carrying a growing infant.
Gentle Exercise and Movement: Practical Approaches
How much activity is enough? Walking remains a foundational recommendation—short, regular strolls help avoid blood clots, raise energy, and support psychological well-being. Simple breathing exercises, pelvic tilts, and Cat-Cow stretches facilitate mobility without overwhelming vulnerable tissues. Attempting strenuous workouts—jogging, weightlifting, high-impact sports—before six weeks (or provider clearance) can jeopardize wound healing and amplify pain. Even returning to driving or sexual activity is best delayed until movement feels steady and pain-free. Here, listening to your body proves indispensable: increased pain, odd swelling, or fever demand timely evaluation.
Wound Care, Scar Management, and Comfort Strategies
Daily incision care involves washing gently with mild soap, patting dry (never rubbing), and observing for changes—redness, drainage, excessive swelling, or an odor warrant prompt attention. Once healed, scar massage (using a simple oil or gentle cream) in small circular motions may help minimize adhesions—tight bands of tissue that can limit movement or cause lasting discomfort. Supportive clothing—loose garments or postpartum binders—offers relief and bolsters mobility. For ongoing pain, simple strategies like holding a pillow against the abdomen during coughing or laughing, and avoiding lifting heavy objects, go a long way in protecting healing tissues.
Fueling Recovery: The Power of Nutrition and Hydration
What lands on your plate matters just as much as rest and gentle movement. Protein-rich foods (chicken, eggs, legumes), abundant fruits, and leafy greens deliver the micronutrients—vitamin A, vitamin C, zinc—that accelerate tissue repair and bolster immunity. Fibre battles constipation, an unwelcome but common postoperative guest. Hydration needs rise, especially during breastfeeding, supporting milk supply and metabolic healing. Structured, balanced meals also stabilize blood sugar, reducing mood fluctuations and energy slumps.
Emotional Adaptation: Mood, Autonomy, and Professional Support
Hormonal turbulence—oxytocin, prolactin, progesterone—shapes postpartum emotions as surely as physical symptoms. Natural mood swings often appear, sometimes compounding feelings of anxiety or exhaustion in the face of disrupted sleep and relentless baby care. Distinguishing between the “baby blues” and more persistent sadness or withdrawal is essential: if low mood lingers beyond two weeks, or if caring for yourself or your baby feels overwhelming, reaching out for professional support can transform the landscape. Psychological research emphasizes that partnership—whether through support groups, peer sharing, or counseling—builds resilience during postpartum transitions.
Breastfeeding After Cesarean: Comfort, Support, and Safe Medications
Finding a sustainable, pain-free breastfeeding position can be challenging when an incision protests. The football hold and side-lying position are favorites, keeping pressure off the abdomen. Support cushions, frequent feeding, and careful latching techniques reduce common issues like engorgement or sore nipples. While most pain medications (acetaminophen, ibuprofen) are considered safe during breastfeeding, always double-check with a provider, especially before using less common remedies.
Complex Recoveries, Multiple Births, and High-risk Conditions
Some cesarean experiences come layered with complexity: prolonged labor, multiple births, or underlying health conditions. Here, postpartum rehabilitation after cesarean takes on an extra dimension—a phased approach to exercise, specialized wound monitoring, and enhanced nutritional support become priorities. Mothers of twins or those navigating chronic medical issues often benefit from structured input from dietitians, physiotherapists, and social support systems, with research demonstrating amplified benefits in physical recovery and emotional well-being.
Everyday Life After Cesarean: Lifting, Caring, and Social Integration
Household responsibilities don’t pause when a new baby arrives—a truth every parent recognizes quickly. The directive is simple: avoid lifting objects heavier than your infant. Engaging leg muscles rather than the back when rising, requesting help from family, and resting whenever possible preserves both abdominal and back health. Intimacy, whether emotional or sexual, resumes best when both partners feel ready, typically after six weeks and with provider approval. Gentle communication, patience, and sometimes lubricant ease the return.
Gradual social reintegration—venturing outside, seeing loved ones, returning to work—follows an individual rhythm. Rushing, comparing, or striving to “bounce back” quickly often does more harm than good. Trust the pace your body and mind sets.
Key Takeaways
- Postpartum rehabilitation after cesarean is a multifaceted process: physical, emotional, and social dimensions intertwine uniquely for each parent.
- Targeted pelvic floor and abdominal exercises form the core of recovery, supported by wound care measures, gentle activity, and nutrition tailored to healing.
- Early mobilization, monitored pain management, and professional guidance help minimize risks like infection, adhesions, or pelvic dysfunction.
- Emotional adaptation is as significant as physical healing: brief baby blues are common, but persistent sadness deserves medical attention.
- Parents benefit from incremental resumption of daily activities, with caution applied to lifting, sex, and strenuous exercise.
- Professional resources abound—consultations, digital tools, peer support—to guide recovery and boost parental confidence.
For tailored advice, daily tips, and access to free health questionnaires for your child, download the Heloa app. Professional input and peer insights are just a click away, empowering families on every step of the postpartum journey.
Questions Parents Ask
When can I start bending and moving more freely after a cesarean?
Many parents wonder when it’s safe to bend or move without discomfort after a cesarean. After surgery, your body needs several weeks to heal, especially around the incision and the internal stitches. It’s generally possible to make gentle movements, such as sitting up or slowly getting out of bed, within the first days post-surgery. As the weeks progress and discomfort lessens, you might find bending a bit easier. There’s no universal timeline—some parents feel ready after a couple of weeks, others need more time. Listen carefully to your body, move slowly, and don’t hesitate to ask for help with daily tasks. If you feel any pulling, sharp pain, or are unsure, it’s always wise to check with your healthcare professional.
How soon can I take a shower after a cesarean birth?
It’s common to feel hesitant about showering after a cesarean birth. Most often, a gentle shower is possible 24 to 48 hours after surgery, following your care team’s instructions. The key is to avoid scrubbing the incision—simply let water run over it without using harsh soaps. Pat the area dry with a clean towel. Baths, swimming pools, and soaking in water should wait until your provider gives you the all-clear, usually after the incision has completely healed. Taking time to care for this area can help prevent infection and support smoother healing.
What foods support healing after a cesarean?
Supporting your body after a cesarean involves focusing on foods that encourage recovery and energy. Protein-rich foods like eggs, beans, chicken, and fish help repair tissues, while a variety of fruits and vegetables provide essential vitamins and minerals. Whole grains offer sustained energy, and foods high in fiber—such as leafy greens and lentils—can ease common issues like constipation. Staying well hydrated is also helpful, particularly if you’re breastfeeding. Eating nourishing meals, even small ones throughout the day, can make a noticeable difference in how strong and supported you feel as you recover.
Further reading: