Every parent grapples with questions about the best ways to nurture their baby, especially amid the whirlwind of new responsibilities and relentless advice. Should you breastfeed? How long is recommended? Is combination feeding acceptable? It’s easy to feel overwhelmed, particularly when facing sleep deprivation, shifting routines, and the pressure of doing “the right thing.” Understanding the true nature and benefits of breastfeeding can illuminate this journey—whether you’re aiming for exclusive nursing, mix-feeding, or simply seeking clarity and reassurance. Let’s untangle the medical, emotional, and practical realities, demystifying both the proven science and the lived experience behind infant feeding. Consider this an invitation to explore, question, and take heart: informed choices are always empowered choices.
Why the Benefits of Breastfeeding Matter: A Look Beyond Nutrition
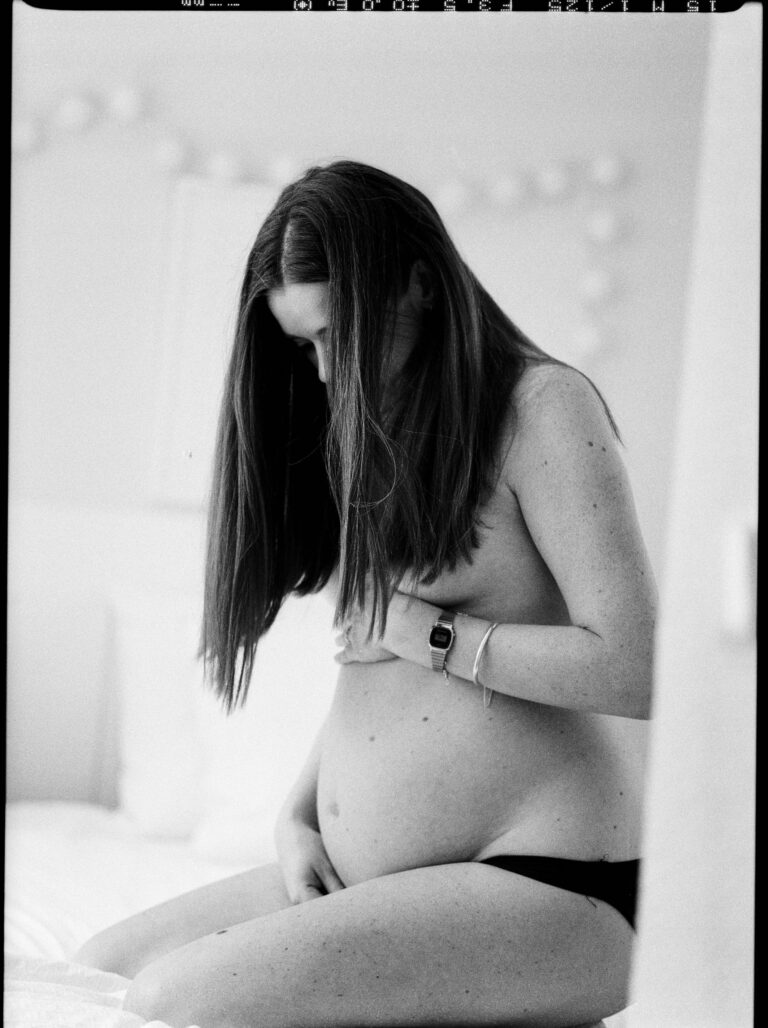
Breastfeeding is not merely a means of providing sustenance. Rather, it is a fusion of physiological processes, family relationships, and personal values. Some parents cherish the skin-to-skin contact and the surge of confidence that comes from witnessing their body nourish new life. Others experience frustration or discomfort, wondering if their reality aligns with what’s often described as natural or effortless. The truth? The benefits of breastfeeding reach far beyond initial perceptions:
- It shapes the immune system with a cascade of live antibodies and essential nutrients.
- It facilitates a unique emotional bond between parent and child, steered by hormones like oxytocin—think of it as a biologically mediated trust-building mechanism.
- It supports recovery for mothers, all while promoting self-assurance as caregiving patterns establish themselves.
But what if returning to work feels like an insurmountable barrier? What if cultural attitudes or family opinions add pressure? These realities are shared by many, and the journey is never one-size-fits-all. Nonetheless, the benefits of breastfeeding—spanning nutrition, emotional support, and autonomy—can offer powerful tools for well-being.
Breastfeeding Recommendations: What Do the Authorities Say?
International organizations unanimously underscore the benefits of breastfeeding. The World Health Organization (WHO) and UNICEF recommend exclusive breastfeeding for the first six months, followed by continued nursing with the addition of solid foods up to two years or longer. In many European countries, including national authorities in France, breastfeeding for at least two years is presented as advantageous for both children and mothers.
Yet numbers tell a more nuanced story. Fewer than one in four infants in high-income regions are exclusively breastfed at six months, a pattern shaped by factors such as parental leave limitations, societal attitudes, and advertising. For many parents, reconciling professional life with the recommendations from pediatric experts feels incongruent. Here’s a detail you might find surprising: workplace accommodations and social support networks are among the strongest predictors of breastfeeding success and satisfaction. Therefore, exploring solutions at the intersection of health policy, family needs, and individual preferences becomes essential.
Health Benefits of Breastfeeding for Mothers: Physiology and Beyond
Medical Advantages and Recovery
Why does the act of nursing quicken postpartum healing? Testosterone and other labor-related hormones recede post-birth, but a surge in oxytocin—sometimes called the “love hormone”—triggers uterine contractions. This phenomenon accelerates uterine involution (the shrinking back to pre-pregnancy size), reduces postpartum bleeding, and limits the risk of anemia due to lowered iron loss.
This isn’t simply a side effect—studies show mothers burn an extra 300–500 calories each day while producing milk. Some experience more rapid postpartum weight loss as energy is redirected toward milk synthesis. In addition, research over the last several decades links breastfeeding with a lower lifetime risk of breast, ovarian, and endometrial cancers; reductions in type 2 diabetes and cardiovascular events; and even a decreased risk of osteoporosis and rheumatoid arthritis. The benefits of breastfeeding for maternal health are, in a word, profound.
And how about sleep? Counter to the myth that breastfeeding disturbs rest, many women report deeper sleep cycles, possibly due to the interplay of prolactin and reductions in cortisol (the “stress hormone”).
Psychological Factors and Empowerment
Repeated releases of oxytocin and prolactin don’t just polish biological processes—they reinforce positive emotions, diminish anxiety, and can repair the bond after challenging or traumatic births. Parents often report a renewed sense of competence and satisfaction—a feeling of having navigated barriers and developed new strengths. Such gains in self-esteem and psychological wellbeing are integral to overall family health.
Health Benefits of Breastfeeding for Infants: Protective, Adaptive, Exceptional
Adaptive Nutrition and Immunology
One of the most celebrated benefits of breastfeeding is its astonishing adaptability. Colostrum, the golden fluid secreted right after birth, is dense with antibodies like secretory immunoglobulin A (sIgA) and cells that guard fragile newborn systems against infections. As days pass, this transition to mature milk converts it into a living, evolving substance that shapes itself to an infant’s needs—delivering altered quantities of essential fatty acids, carbohydrates, and water during fevers or hot weather.
- Did you know breast milk can increase water content if your child shows early signs of dehydration?
- Or that it becomes richer in protective elements during periods of illness, offering extra ammunition to a vulnerable immune system?
Gut microbiota—the trillions of microscopic organisms inhabiting your child’s digestive tract—are also tuned and nurtured by special sugars called human milk oligosaccharides. These pave the way for healthy digestion and optimal nutrient absorption, creating a fortified barrier against harmful pathogens.
Defense Against Infections and Chronic Diseases
Babies nurtured by breast milk enjoy measurable declines in:
- Gastrointestinal infections (e.g., diarrhea and vomiting)
- Respiratory tract illnesses (such as bronchitis and pneumonia)
- Otitis media (ear infections)
- Hospital admissions for infections
The presence of omega-3 and other long-chain polyunsaturated fatty acids within breast milk supports cognitive development, laying the groundwork for advantageous language, focus, and social skills throughout childhood. Studies also suggest a lower incidence of sudden infant death syndrome (SIDS), allergies, and pediatric obesity in exclusively breastfed infants.
Communication and Connection
Feeding at the breast encourages parents to decode early cues—little fists rooting at cheeks or fussy cries—helping to build mutual trust. The dance of demand and supply can be freeing: no measuring, no clocks, no need for external validation; just attentive, instinctive parenting.
Emotional, Psychological, and Social Dimensions
The Power of Skin-to-Skin and Responsive Parenting
The tangible benefits of breastfeeding include a deeply rooted sense of connection. Oxytocin and prolactin prompt a soothing calm—this is more than a poetic metaphor; it’s a series of observable cardiac and neurological effects. Families often cite a feeling of safety, tranquility, and joy during feeding times.
Family Dynamics and Societal Perspectives
Yet, not all parents experience universal support. Family, friends, even strangers can voice opinions (sometimes constructive, often unsolicited). Well-meaning partners and relatives may assist with chores, emotional support, or nighttime wakings. Community acceptance—think parent support groups, peer counselors, and public spaces designed for nursing—positively shapes experiences. Conversely, social stigma can introduce stress or self-doubt, making acknowledgment and normalization of breastfeeding practices so important for long-term satisfaction.
Maternal Wellbeing and Self-Image
Overcoming breastfeeding challenges can kindle pride and a new perspective on body image—a celebration of function rather than appearance. For many, feeding sessions soon become moments of peace and intimacy amid chaos, fostering resilience and adaptation through each developmental leap.
Societal, Economic, and Environmental Perspectives
Public Health Advantages
Higher rates of breastfeeding correspond with lower healthcare costs—not just because of fewer hospital stays, but due to lasting reductions in chronic diseases like diabetes and hypertension. In populations where breastfeeding is normalized, some data indicates improved outcomes in infant mortality rates and community wellness.
Financial Considerations
A sometimes-overlooked benefit of breastfeeding involves simple economics. Parents may circumvent expenses on formula, sterilizing equipment, and bottles. Over time, these savings accumulate—fewer sick days from work, reduced doctor visits, minimized pharmacy expenditures.
Sustainability and Ecology
Unlike formula, breastfeeding generates no packaging waste, demands no industrial production, and produces only what the child needs (minimizing food loss). With every feeding, ecological costs plummet—a subtle yet powerful contribution to environmental stewardship.
Addressing Misconceptions and Surmounting Challenges
Practical Realities
Does breastfeeding look like sleepy smiles and perfect latch every time? Hardly. Many experience sore nipples, occasional mastitis (breast inflammation), doubts about milk supply, and the logistical tangle of expressing milk during work hours. Social myths—think “formula is just as good” or “breastfeeding and career don’t mix”—further blur confidence.
Yet, actionable steps can pave the way:
- Consulting a lactation consultant for hands-on support (especially with latching and supply issues)
- Joining support groups for practical tips and shared encouragement
- Advocating for workplace solutions: private lactation rooms, flexible breaks for pumping, and transparent HR discussions
- Engaging partners and loved ones in supportive roles, from meal prep to emotional encouragement
Reliable, science-based information relayed by healthcare professionals helps dismantle persistent myths. Each family’s solution may look different—and that’s entirely valid.
Key Takeaways
- The benefits of breastfeeding for infants stretch from superior nutrition and powerful immune protection to boosted brain development and reduced risk of chronic diseases.
- Mothers gain both immediate and enduring health rewards—faster recovery, lower risks of cancer and metabolic disorders, and greater emotional wellbeing.
- Psychological and social advantages can enhance self-esteem, foster relational bonds, and provide a sturdy foundation for family life.
- Official organizations like WHO advocate for six months of exclusive breastfeeding, followed by continued nursing alongside complementary foods up to two years or beyond.
- Family, workplace, and community support are vital for overcoming practical and emotional hurdles, boosting satisfaction and perseverance.
- Choosing breastfeeding can yield substantial environmental and financial advantages—benefiting individual families and the wider world.
- Facing challenges doesn’t mean missing out on all the benefits of breastfeeding; instead, tailored solutions and professional guidance allow every parent to pursue what feels best for their child and themselves.
If you’re searching for customized advice or wish to track your child’s health and milestones, consider downloading the Heloa app for evidence-based guidance and free health questionnaires—because every parenting path deserves expert support and respect.
Questions Parents Ask
Does breastfeeding reduce the risk of allergies and asthma in babies?
Many parents wonder whether breastfeeding can help prevent allergies or asthma in their child. Studies suggest that exclusive breastfeeding during the first months of life can lower the likelihood of developing allergies and asthma, especially in families with a history of these conditions. This protective effect is linked to the antibodies and unique immune factors found in breast milk, which support the baby’s developing immune system. Every situation is unique, but know that breastfeeding may offer this additional layer of defense—even though no single method guarantees complete prevention. If you have concerns about allergies or family medical history, discussing them with your pediatrician can help you find the best approach for your child.
Is breastfeeding beneficial for the environment compared to formula feeding?
Absolutely—breastfeeding is recognized as a more environmentally friendly option. It produces no packaging waste, does not require industrial manufacturing, and uses no additional resources for transportation or storage. In contrast, infant formula production consumes significant amounts of water, raw materials, and energy, and generates waste through packaging and distribution. By breastfeeding, parents contribute to reducing their ecological footprint, which is a positive and meaningful action for the planet—however small it may seem on a daily basis.
Can breastfeeding lower the risk of certain cancers for mothers?
Yes, research indicates that mothers who breastfeed may have a lower risk of developing certain types of cancers, such as breast and ovarian cancer. This protective benefit is associated with the hormonal changes that occur during lactation, influencing breast and ovarian tissue over the long term. While breastfeeding is just one factor among many that influence cancer risk, it’s reassuring to know that it brings an added advantage for maternal health. As always, if you have questions about your own health risks, your healthcare provider is there to support and guide you.
Further reading: