No parent expects their child’s laughter on a summer day to turn, suddenly, into a scene of urgent concern. Yet questions about heatstroke in children whirl through the minds of many families as the temperature climbs: “How do I spot the warning signs? What should I do if my child seems unwell in the heat? Is it really that risky to play outside, or nap in the stroller?” These are not just passing worries—they reflect real, pressing dilemmas. The good news? Proactive strategies and clear information can dramatically reduce the risks. Across these sections, discover how to recognize early symptoms, when to react, and why quick intervention matters, all while separating persistent myths from scientific facts. Behind every statistic, there’s a family, perhaps just like yours, whose summer could be safer with the confidence that comes from knowing what to do.
Understanding Heatstroke in Children: Why Are Kids So Vulnerable?
Heatstroke in children, sometimes called pediatric heat-related emergency, is more than “just” overheating. The physiology of young bodies tips the scales: children heat up three to five times faster than adults, partly due to their proportionally larger body surface area compared to weight and a still-developing ability to dissipate heat through evaporation (sweating). Their innate sense of thirst isn’t as reliable—meaning they rarely ask for water until they’re already dehydrated.
But not all forms are alike. Exertional heatstroke hits athletes or kids racing around the playground in peak heat. Classic heatstroke creeps in after exposure to a sweltering, poorly ventilated environment—think strollers shrouded in blankets, cars sealed in parking lots, or bedrooms with closed windows during a heatwave. Even a shaded tent can become an oven on the wrong day.
Caregivers may wonder, “What makes my child more at risk?” Age is key—infants and toddlers can’t remove themselves from harm, while their sweat glands haven’t matured enough for robust cooling. Chronic illnesses, fever, and certain medications (anticholinergics, diuretics, stimulants, beta blockers) increase susceptibility by hampering heat loss or fluid balance. Overdressing, restrictive covers, and a lack of hydration amplify the danger.
Recognizing the Signs: Symptoms to Watch Closely
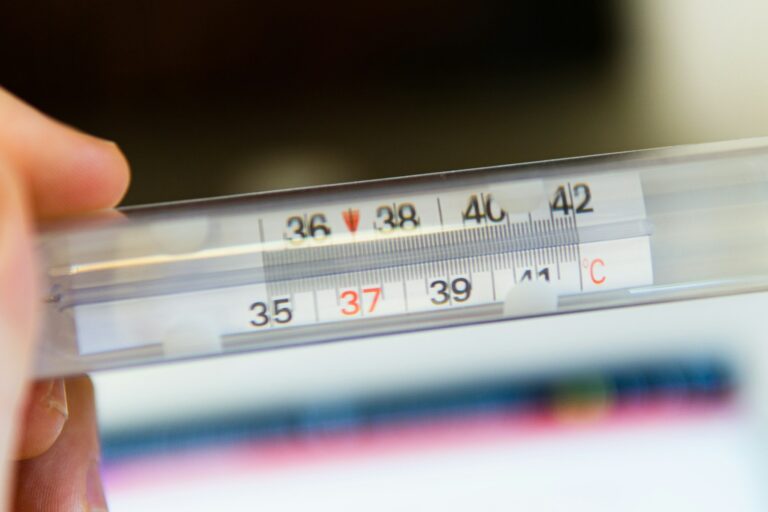
Vigilance saves lives, especially with heatstroke in children. Imagine a child whose cheeks are suddenly scarlet, whose skin feels dry and hot—or paradoxically, drenched in sweat but listless. Early manifestations often masquerade as mild illness: low-grade fever (above 100.4°F/38°C), nausea, irritability, tiredness bordering on lethargy, dizziness, muscular cramps, or a pounding headache. For infants, poor sucking, limpness, or persistent sleepiness may be the only warning.
As the core temperature surges past 104°F (40°C)—now a genuine medical emergency—the landscape shifts. Pallor may be replaced by a striking flush; consciousness might waver, replaced by confusion, slurred speech, or outright collapse. Seizures, shallow or rapid breathing, unresponsiveness: red flags demanding instant action. While some children still sweat during heatstroke, others will have hot, dry skin—a detail that can mislead unsuspecting adults.
Primary Triggers: Where and When Heatstroke Strikes
Why do so many stories about heatstroke in children begin with a parked car, a closed tent, or a playground under a merciless sun? The reason: confined, poorly ventilated spaces trap heat rapidly, turbocharging the rise in ambient temperature. In a sealed vehicle, cabin air can breach 120°F (49°C) within minutes—even if the outside temperature feels tolerably “warm.”
But not every risk lurks in the obvious places. Extended outdoor play, especially when accompanied by dehydration or heavy clothing, siphons away the body’s water reserve. Children participating in sports events or vigorous outdoor activities between 10 a.m. and 4 p.m.—the “danger zone” for solar intensity—face multiplied threats.
Medications that decrease sweat production or alter hydration, acute illnesses (gastroenteritis with vomiting or diarrhea), and neurological conditions can create a perfect storm. Even familiar situations—napping in a sunlit room, bundled in winter clothing indoors on an early spring day—harbor hidden risks.
Emergency Measures: What to Do When Seconds Matter
A child’s wellbeing can unravel with alarming speed during heatstroke in children. The question lingers: “What exactly should I do if I notice these symptoms?” Begin by seeking emergency help immediately. Every moment counts.
While awaiting medical support:
- Relocate your child to a shaded, cool, or air-conditioned area (if possible, an interior room or vehicle running AC).
- Strip off extra clothes, including socks, hats, and blankets.
- Initiate gentle but continuous cooling—apply lukewarm water (never ice-cold) with sponges or misting bottles, concentrating on high-blood-flow zones: the neck, armpits, groin.
- A fan will hasten cooling through evaporation but avoid overcooling; shivering can paradoxically raise body temperature.
- Offer sips of water only if your child is fully awake and able to swallow (never force fluid in a confused or drowsy child).
- Steer clear of fever medications like acetaminophen or ibuprofen—they won’t address the underlying thermal imbalance and could obscure the clinical picture.
Unconscious children require special caution. Place them on their side (the recovery position) to maintain an open airway and monitor their breathing carefully—breathing alteration or apnea requires immediate resuscitation techniques if you’re trained.
Regardless of interim improvement, the road never ends at home: every case of heatstroke in children requires systematic hospital assessment. Complications can develop later, and only medical teams can evaluate organ function or neurological risk with confidence.
Medical Assessment and Hospital Treatment
So what unfolds at the emergency department for heatstroke in children? Healthcare professionals prioritize rapid cooling—either with immersion in cool (not freezing) water, controlled misting, or applying cold packs to the neck, groin, and armpits. Intravenous fluids restore circulating blood volume and help correct electrolyte disturbances. Continuous monitoring of temperature, heart rate, neurological status, kidney and liver function, and urine output helps spot early signs of brain injury, muscle breakdown (rhabdomyolysis), or clotting abnormalities.
Blood tests can reveal elevated muscle or liver enzymes, abnormal sodium or potassium levels, or markers of infection or dehydration. Sometimes, advanced imaging or specialist input is needed. The recovery process is meticulously gradual—abrupt shifts could induce life-threatening complications.
Children recovering from severe heatstroke may need neurological evaluation, physical therapy, or even long-term follow-up. Memory, movement, and learning difficulties can arise after the event, so attentive observation in the weeks following discharge is recommended.
Prevention Starts at Home: Simple, Effective Strategies
Few threats are as predictably preventable as heatstroke in children. The arsenal of effective strategies is reassuring:
- Never leave a child in a parked vehicle, not even for a minute. The temperature inside can skyrocket faster than you’d ever imagine, even if the window is cracked.
- Hydration isn’t optional. Encourage routine drinks—water is best—before, during, and after outdoor activities. Children rarely recognize thirst before dehydration sets in.
- Dress with intention: loose, light-colored clothing; sun-protective hats; and regular sunscreen use.
- Seek out shade or create your own with umbrellas, canopies, or planning outings in the early morning or late afternoon.
- Maintain cool indoor environments—fans, closed blinds, air conditioning (when available), and cool baths can make a staggering difference.
- Avoid excessive bundling, especially for infants, who are poor regulators of their own body temperature.
- Always double-check car seats before locking the vehicle, and instruct every caregiver to do the same.
Teaching children to recognize and report early warning signals—headache, dizziness, fatigue, nausea—empowers even the youngest to play a vital role in their own protection. Keep lines of communication open with teachers, coaches, babysitters, and relatives. Consider checklists for outings or sports days.
Special Considerations: Infants, Toddlers, and Children with Medical Conditions
Some children need bespoke precautions. Infants—unable to shed layers or request water—should wear only light clothes and be shielded from sun at all times. Watch for subtle signs: quickened breathing, irritability, a lack of appetite or trouble arousing from sleep. Children with chronic illnesses, those using medications that impair sweating or hydration, and individuals with neurodevelopmental conditions demand heightened vigilance.
Maintain good room ventilation, avoid excessive bedding, and check hydration status repeatedly. Ask your healthcare provider if medications need adjustment. Make sure all caregivers are briefed about these enhanced needs—brief lapses in routine can unravel safety in vulnerable children.
Myths, Misconceptions, and Public Health Trends
The narrative persists: “It’s only risky if the child is forgotten in a car.” In reality, heatstroke in children can unfold anywhere—a sunlit living room, a poorly ventilated day-care, or fields during a sports tournament. Another widespread myth: sweating always vanishes in heatstroke. Not so—sweat production varies wildly. And fever medications? They offer no help in lowering a dangerously elevated core temperature due to heatstroke, and using them can divert attention from essential cooling techniques.
Public health data highlights that most cases arise in summer—during heatwaves, humidity spikes, school vacations. The age group most frequently affected? Children under five, whose independence hasn’t caught up to their curiosity. Boys and girls are equally at risk, and sports-related scenarios remain a particular concern. Prevention campaigns and community awareness offer immense benefit—they save lives.
Key Takeaways
- Heatstroke in children is a medical emergency requiring swift recognition and immediate action. Body temperature surpassing 104°F, altered consciousness, and dry, hot skin signal urgent danger.
- Children are prone to rapid overheating due to unique physiological vulnerabilities, underdeveloped sweating, and reduced thirst response. Infants, toddlers, and children with medical conditions warrant special vigilance.
- Symptoms range from subtle (lethargy, headache, pallor) to dramatic (seizure, collapse), and can progress rapidly.
- Prevention is both simple and powerful: frequent hydration, shaded play, cool clothing, sun protection, and avoiding closed vehicles save lives.
- Don’t hesitate to act—a prompt response makes all the difference. Even children who seem to recover at home should be examined by medical professionals to rule out complications.
- Professional and reliable sources—such as pediatricians, official health agencies, and community campaigns—are invaluable in keeping families informed and prepared.
Feeling uncertain or needing tailored advice for your child’s unique situation? Consider downloading the Heloa app for personalized tips and free child health questionnaires, supporting you every step of the way, every season.
Questions Parents Ask
Can heatstroke in children cause long-term complications?
Heatstroke may sometimes lead to long-term effects, especially if the child’s body temperature remained very high for an extended period before intervention. Some children can experience changes in concentration, memory, or physical strength during the weeks following the event. In rare situations, neurological, cognitive, or kidney-related issues can appear after recovery. Fortunately, most children who receive timely medical attention recover fully. If you notice your child having learning difficulties, frequent headaches, or changes in mood after an episode, do not hesitate to consult a healthcare professional. It is important to keep an open dialogue with your child’s doctor for reassurance and personalized guidance.
How quickly can heatstroke develop in a child?
Heatstroke can develop surprisingly fast in children, sometimes within minutes in hot, enclosed environments such as cars or tents. Even outdoor heat exposure during play or sports can lead to symptoms in less than an hour, especially if hydration is insufficient or if the child is dressed too warmly. Younger children are especially sensitive, as their bodies struggle to cool down efficiently. That’s why it is essential to monitor for warning signs when temperatures are high—quick action is often the best way to keep your child safe.
Are there activities that increase the risk of heatstroke in children?
Certain activities do make children more vulnerable to heatstroke. Vigorous outdoor sports, extended playtime in the sun, or any event happening during the warmest hours of the day increase risk, particularly if breaks are rare or access to shade and water is limited. Sleeping in a stroller or car seat, even for a short period, can become risky if the environment heats up. Remind children to pause for water and rest regularly, and plan active times for early mornings or later afternoons. With a few mindful adjustments, children can continue to enjoy outdoor activities safely.
Further reading: