For many parents, sleep quickly shifts from a taken-for-granted necessity to a daily pursuit—a complex journey peppered with questions, longing, and, sometimes, a quiet sense of desperation. When does baby sleep through the night? It’s a question whispered in the dark, mulled over during midnight feeds, and debated across countless parenting forums. The search for uninterrupted sleep embodies not just fatigue, but hopes for tiny victories—longer sleep stretches, a predictable rhythm, a sense that comfort is, finally, within reach. Rest assured, understanding the science beneath infant sleep, the interplay of biology and environment, and recognizing individual pacing can be powerful tools. Here, you’ll find the answers to common questions, evidence-based strategies, and explanations of how and why when does baby sleep through the night is not the same for every child.
What “sleeping through the night” means—for parents and babies
When parents ask, “When does baby sleep through the night?”, the desire is clear: uninterrupted rest, for both adult and child. Medically, this typically refers to a period of 6-8 hours of continuous sleep. Some may envision a full 10-12 hours, but few infants oblige so early. Sleeping through the night doesn’t mean absence of waking—adults themselves cycle between light and deep sleep, often shifting position, briefly awakening before drifting off again. Likewise, babies may rouse between sleep cycles but only stir their parents if unable to settle themselves back.
For families returning to work or seeking to restore some sense of normalcy, aligning the baby’s sleep intervals with the adults’ nighttime can transform daily life. This intersection—where infant biology, parental needs, and household dynamics meet—marks one of early parenthood’s main turning points.
How baby sleep really works: understanding rhythms and cycles
Infant sleep cycles: striking contrasts with adult sleep
Newborns experience short, ultradian sleep cycles—about 50 minutes each—where half of this time is spent in rapid eye movement (REM) sleep, that active, light stage often associated with dreams and physiological brain development. Compare this to adults, whose cycles extend to 90–120 minutes, with more consistent transitions between deep and shallow sleep. This difference, explained by neurodevelopmental immaturity, means infants will wake more frequently, day and night.
As the circadian system (the biological clock that responds to light and dark) begins to mature, sleep consolidates—babies gradually start to distinguish night from day, and the hope grows stronger: When does baby sleep through the night may finally have an answer.
Developmental milestones: timelines for sleeping through the night
Newborns (0–3 months): fragmented sleep and frequent feeds
For a newborn, sleep dominates—16-18 hours spread over 24 hours—but true rest for parents remains elusive. Small stomachs, intense metabolic needs, and an immature circadian system dictate short bouts, 2–4 hours at a time. During this phase, it is virtually unheard of for an infant to sleep longer than 5 hours. When does baby sleep through the night feels out of reach, and that’s entirely normal—biology insists on frequent waking for survival and growth.
3–6 months: Sleep extension and shifting patterns
Between 3 and 6 months, an important transition begins. Melatonin, a hormone that signals darkness and tranquility, starts following more regular cycles as the pineal gland matures. Cortisol, which boosts wakefulness and energy, finds its rhythm as well. Result? Sleep blocks stretch—sometimes up to 5–6 hours. However, just as relief approaches, the 4-month sleep regression enters the scene: evolving neural pathways temporarily disrupt the fragile structure, and when does baby sleep through the night remains a moving target. Still, many infants at this stage can offer one stretch that resembles a “night,” often from a late evening feed to early morning. Be prepared for variation—this window is fluid and highly individual.
6–12 months: longer stretches, but new challenges
Most babies are now capable—if development, feeding, and environment align—of sleeping 6–12 hours. Why the range? Teething pain, mastering bold new motor skills (crawling, standing), minor illnesses, or anxiety about separation may provoke unexpected wakings. Night feeds often decrease, replaced by needs for reassurance and comfort. The elusive phrase, when does baby sleep through the night, is now within grasp for many, yet still not guaranteed for all.
Toddlers and beyond: consolidation, with bumps in the road
After 12 months, sleep usually becomes more consistent, though periods of disruption—caused by separation anxiety, rapid physical and emotional growth, or transitions in routine—should be anticipated. Temporary regressions do not erase progress; rather, they reflect natural adaptation in a developing child.
Individual variation: why sleep is unique to every baby
Just as adults may be natural “night owls” or “early birds,” infants possess distinct sleep temperaments. Some may achieve 8–10 hour uninterrupted stretches as young as one month, while others continue to wake at night past their first birthday. Family genetics, feeding practices, temperament, and environmental cues all shape the answer to when does baby sleep through the night.
Between two and four months, sleep typically begins to organize into longer night intervals. Many parents consider their baby to be “sleeping through” when the first morning feed comes after 6 a.m. following a late-night feed. However, some children need a slower timetable, and such diversity is both expected and healthy.
Why do babies wake during the night?
Beyond basic hunger, post-4 months, night waking is more likely tied to emotional and sensory needs—desire for reassurance, discomfort with noise or temperature, or minor physical irritation (teething, congestion, an itchy onesie). Light, room temperature, and ambient sound all impact sleep continuity. Parents often wonder when does baby sleep through the night because every small disruption—creaking floors, barking dogs, late-night discussions—may echo louder in the delicate world of infant sleep architecture.
Influences on night sleep: what really matters
Feeding and nutrition: milk matters, but not forever
Breastfed infants typically digest food faster than formula-fed peers, potentially requiring more frequent feeds and waking accordingly. Over time, adjustment of daytime intake and a gradual stretch in night intervals can help. Key is respecting each child’s nutritional requirements—growth will stall, not accelerate, if calories are sacrificed for convenience. A safe, responsive transition is paramount; abrupt weaning or schedule shifts can create its own sleep turbulence.
Sleep environment: where biology meets comfort
A scientific approach highlights several essentials:
- Cool temperatures (68–72°F / 20–22°C)
- Minimal light, preferably using blackout curtains
- White noise (steady, non-distracting background sound)
- Firm crib mattress, no pillows or loose objects
These modifications may seem minor but, collectively, dramatically impact whether when does baby sleep through the night becomes a reality.
Routine and self-soothing: the building blocks of independence
Building a consistent bedtime sequence signals—at a biological and psychological level—that sleep is imminent. Research supports routines incorporating baths, lullabies, gentle rocking, or massage. Babies who are placed “drowsy but awake” in their beds have shown, through multiple studies, a greater capacity to self-soothe: falling asleep unassisted, then resettling themselves during normal partial arousals. Gradual reduction in parental intervention isn’t always easy, but it lays the foundation for longer, peaceful nights.
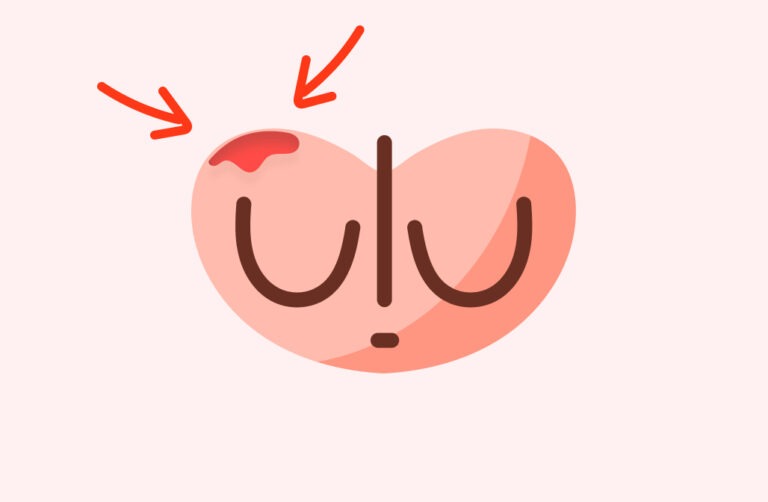
Health and development: the wild cards
Growth spurts, teething, or temporary illnesses, including eczema or even mild gastroesophageal reflux (a common cause of sleep disruption), can interrupt established patterns. Pediatric review is warranted if underlying health issues are suspected. Adjust sleep routines when a child is unwell, then gently return to baseline as recovery occurs.
Family patterns and temperament: genetics in action
Some infants crave prolonged parental proximity to fall and stay asleep, while others thrive with gentle separation. Studies in pediatric sleep medicine confirm the intersection of genetic sleep traits, family routines, and caregiver responses. Acceptance of each family’s unique dynamic, rather than comparison or rigid schedules, fosters realistic expectations—a key to emotional wellbeing for both parent and child.
Signs your baby may be ready to sleep through the night
Recognizing readiness involves more than counting months on a calendar.
- Decreased night feedings: If feeds drop and daytime nutrition is robust (steady weight gain, visible satisfaction after feeds), longer stretches may emerge.
- Self-soothing skills: Observing your baby drift off with thumb sucking, soft breathing, or the gentle clutch of a safe sleep object suggests a capacity to self-regulate.
- Improved wakefulness during the day: More sociable, active, and alert infants often exhibit stronger circadian rhythms, helping differentiate night from day.
Strategies for supporting night sleep: actionable steps
Respecting “wake windows”: matching rest needs to age
- Newborns: awake periods of 45–60 minutes
- 3–6 months: 1.5–2 hours
- 6–12 months: 2–3.5 hours
Exceeding these times regularly triggers overtiredness—a paradoxical increase in night wakings powered by surges of cortisol, the stress hormone. Early cues like yawning or eye rubbing signal a need for prompt sleep.
Consistent bedtime routine: creating signals for sleep
A soothing sequence—dim lights, soft sounds, gentle touch—reinforces the biological drive for sleep. For young infants, swaddles and rocking mimic the womb, while older babies may benefit from baths, rhythmic stories, and calm music.
Safe sleep setting: essentials for rest and security
Keep the crib free of objects, maintain an optimal temperature, and deploy white noise machines to buffer environmental flares. Sleep sacks over blankets continue to be recommended by pediatric sleep experts as a means to prevent accidental suffocation and provide comfort.
Fostering independent sleep skills: gentle approaches to autonomy
Transferring your baby when “drowsy but not fully asleep” lays the groundwork for self-regulation. Parents drawn to sleep training—from gradual withdrawal to “check and console” routines—should consider readiness around 4–6 months, taking cues from their infant’s temperament and feeding schedule.
Navigating setbacks: resilience through consistency
Sleep regressions, especially at 4 and 8 months, are well-documented. Coping strategies include maintaining routines, offering comfort without overhauling established sleep habits, and remembering that these phases, while exhausting, are fleeting.
Addressing common nighttime challenges
Sleep regressions
Developmental leaps—whether physical (rolling over, crawling) or emotional (new separation awareness)—often result in temporary disruptions even for babies with previously stable nights. A return to predictability is inevitable with gentle persistence.
Illness, teething, and routine changes
Pain, nasal congestion, or travel-induced time zone shifts may all unravel sleep for brief periods. The priority is to address the underlying need—pain relief for teething, optimized sleep environments for illness—before a swift return to comforting rituals.
Separation anxiety and late night wakings
From around 9 months onward, infants may express new fears or seek additional reassurance as they understand separation. Comforting check-ins, presence without excessive stimulation, and the introduction of age-appropriate “lovies” (safety-tested comfort objects) can soothe anxieties.
When to seek further support
Symptoms that merit professional attention
- Multiple, persistent night wakings in babies older than 6 months, with clear difficulty resettling
- Signs of discomfort—gastroesophageal reflux, eczema, breathing disturbances
- Stagnant or declining growth, persistent feeding trouble
Paediatricians, sleep specialists, and other healthcare providers can screen for medical issues and offer individualized approaches when when does baby sleep through the night is more than just a waiting game.
Comprehensive solutions for persistent difficulties
When sleep deprivation or chronic disruption becomes overwhelming, outside assistance brings relief and insight. Targeted advice—rooted in paediatrics and sleep science—empowers families to reclaim rest.
Understanding sleep patterns: tracking and cues
Documenting wake and sleep cycles, naps, and nighttime intervals—whether in a notebook or using a dedicated app—provides invaluable data for recognizing patterns and planning interventions. Reading subtle signals (yawning, fussing, staring off) often enables preempting overtiredness, setting the stage for easier sleep transitions.
Shaping realistic expectations and prioritizing self-care
Improvement rarely occurs in a straight line; babies—and families—ebb and flow through routines that mix progress and setbacks. Alternating night duties, accepting help, and maximizing rest during daytime naps supports parental resilience and energy, key to managing the unpredictable territory of when does baby sleep through the night.
Key Takeaways
- The age at whichwhen does baby sleep through the night becomes reality varies widely; anywhere between 3–12 months is typical.
- Maturation of circadian rhythms, improved feeding, environmental tweaks, and self-soothing skills all foster progress, though temporary regressions are common and expected.
- Breastfeeding, formula feeding, room environment, and health issues—each shapes sleep in unique ways.
- Gentle, evidence-based routines and safe sleep setups are essential.
- Every baby—and family—is unique; there is no single answer to when does baby sleep through the night. Observe, adapt, and if concerns arise, consult healthcare professionals.
- Professional resources and pediatric expertise are available for families needing extra guidance. For tailored advice and free health questionnaires for children, download the Heloa app—support is always within reach, whenever when does baby sleep through the night still feels just out of reach.
Questions Parents Ask
How can I help my baby differentiate between night and day?
Supporting your baby to distinguish day from night can make nighttime sleep smoother. During the day, allow plenty of natural light in the house and engage in playful interactions. At night, keep the environment quiet, the lights dim, and make nighttime feeds calm and brief. This routine gradually teaches your baby that nights are for rest, helping their internal clock to adjust.
Is it normal for my baby to sometimes sleep through the night and then revert to frequent waking?
Absolutely, this is quite common. Babies’ sleep can fluctuate due to growth spurts, new milestones, teething, or even minor colds. Temporary regressions, even after a period of solid sleep, are part of normal development. Rassurez-vous, these phases usually pass, especially with supportive routines and gentle reassurance.
Should I wake my baby to feed during the night?
If your baby is healthy, gaining weight well, and your pediatrician has no concerns, you usually don’t need to wake your baby for night feeds after the first weeks. However, for newborns or babies with specific medical or growth needs, it is important to follow your healthcare professional’s advice. As always, adaptation to each baby’s unique rhythm is key.
Further reading: