When your child coughs through the night or a seemingly minor rash sparks a world of worries, suddenly calm becomes elusive. Questions, big or small, multiply fast: Is it serious? Should you see a pediatrician urgently? Can you handle it at home, or is there cause for greater concern? For many parents, the world of children’s health feels like an intricate map—full of unknowns, unexpected detours, and sometimes, the weight of needing to make the “right” decision at every twist and turn. The pediatrician stands as a reliable companion in these moments, someone to not only decode symptoms and treat illnesses, but to anticipate needs, support developmental stages, and offer reassurance when uncertainty runs high. From newborn check-ups to guidance on vaccination, nutrition, and behavioral shifts, the pediatrician offers more than answers; they offer partnership. So, what truly sets these specialists apart? Why do they matter in an era where information seems only a click away?
Understanding the Pediatrician’s Role: Science, Care, and Reassurance
The term pediatrician might call to mind stethoscopes and routine checkups, but the expertise runs much deeper. Trained exclusively in the care of infants, children, and adolescents, a pediatrician embodies a blend of advanced clinical knowledge and a remarkable ability to connect with families under stress. Unlike a family doctor, whose skills cover all age groups, a pediatrician is uniquely equipped to spot infant respiratory distress, assess developmental milestones such as speech acquisition, and recognize subtle differences in disease presentation—think of how appendicitis typically appears in a toddler compared to an adult. When a child’s growth chart veers off track or a milestone stalls, a pediatrician brings an eye for patterns and red flags.
But have you ever wondered why the visit takes so long even during “simple” follow-ups? It’s not just about measuring weight or checking head circumference: each interaction weaves together physical, emotional, and social observations. Do you notice hesitancy with certain foods? Is sleep interrupted by nightly awakenings or allergies? The pediatrician builds a profile over time, tracking everything from vaccination status to environmental influences (childcare settings, siblings). This depth prevents missteps and allows tailored advice—no child is “average,” and no recommendation is given lightly.
Specific Skills and Qualities: Blending Science With Sensitivity
Precision matters. The pediatrician’s knowledge encompasses everything from growth monitoring to the nuances of infant immune systems. Yet, technical skill alone isn’t enough. What distinguishes outstanding care is listening: the ability to translate parental concern into appropriate action. Is your toddler’s refusal to eat vegetables a phase or a sign of sensory aversion? Should persistent stomach aches prompt a discussion about anxiety as well as digestion? Families rely on their pediatrician’s judgment when worries arise late at night or symptoms shift rapidly. Active listening, empathetic advice, and clear explanations are not just helpful; they are essential for building trust and securing positive outcomes.
Prevention forms the backbone of pediatric practice—not only detecting illness, but pinpointing risk factors before they surface. Expect conversations about nutritional guidance, safe sleep, accident prevention (from stair gates to poison safety), and screen time. Healthy habits start early, and the pediatrician acts to empower, not dictate.
Training and Expertise: A Long Path to Mastery
What does it take to become a pediatrician? Far more than a white coat and compassion. After rigorous undergraduate and medical training, future pediatricians embark on exhaustive years of specialty rotations: learning not just how to recognize rashes or order tests, but how a child’s body reacts uniquely to disease, trauma, and medication. Many extend their training (several more years) to master fields like neonatology (care of fragile newborns), pediatric endocrinology (hormonal issues like diabetes), or pediatric neurology for complex neurological conditions.
The landscape is evolving, too. The majority of pediatricians are now women—a shift that’s changed everything from appointment structure to consultation style. Modern practitioners juggle hospital rounds, community health visits, and even video consultations—adapting to family needs and the unpredictability of childhood illness.
Where Pediatricians Practice: Settings and Accessibility
Children’s care doesn’t stop at one office. Pediatricians work in clinics for standard follow-up, hospitals for acute issues (like seizures, severe asthma attacks), maternity wards for newborn assessment, and community health centers focused on outreach and prevention—think vision screenings, immunization drives, or managing conditions like anemia in underserved populations. Telemedicine has further expanded reach—consultations by video allow regular check-ins, fine-tuning of chronic care (asthma, eczema), and rapid reassurance for concerns that might not need an in-person exam.
Coordinating across settings, pediatricians create a safety net—ensuring detailed information is shared, every measurement is logged (often in a parent-held health book), and that transitions (from maternity ward to home, from family practice to specialist) happen without miss-steps. This network is invisible to most parents but proves essential when quick, multidisciplinary action is needed.
Regular Check-Ups: What to Expect and Why They Matter
Visits follow a rhythm. Immediately after birth, a baby meets their pediatrician for a full-body review: checking tap reflexes, heart sounds, and hip stability. Over the first year, appointments are regular—monthly to start, then gradually spreading out—as growth trends, feeding patterns, and vaccine schedules are monitored closely. Each age brings new screening points: Do they fix and follow with their eyes? Are first words emerging at expected times? Can they manage small finger foods without choking?
The growth curve—tracking height, weight, and head circumference—serves as a blueprint for wellbeing or potential trouble. If deviations occur, further assessments, such as hearing checks or development screens, come into play. This careful surveillance enables early intervention, supporting everything from speech delays to chronic diseases.
Advice for Everyday Challenges: Food, Sleep, Hygiene
Parenting doesn’t come with an instruction manual, and many encounters with the pediatrician revolve around everyday puzzles. How do you encourage a picky eater? What’s normal sleep for a six-month-old? Is a fever after a vaccine a sign of immunity or worry? Answers rarely fit a single template. Some children thrive on routine; others need a more flexible approach. The pediatrician offers evidence-backed guidance: when to push, when to wait, and when to seek more specialized support. Hygiene, too, gets serious treatment: from handwashing techniques to strategies for head lice outbreaks or diaper rash remedies.
Managing Illness: Acute, Chronic, and Emergency Scenarios
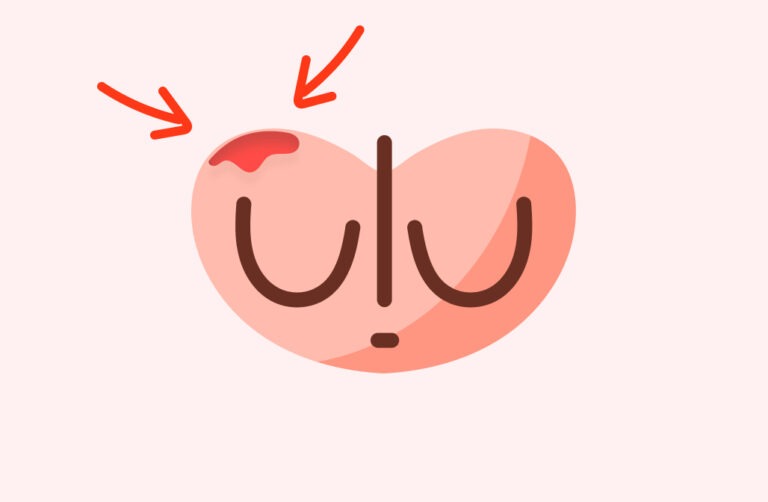
When illness strikes, the pediatrician’s approach is swift and systematic. Whether you’re dealing with bronchiolitis in winter or a sudden asthma exacerbation, diagnostic clarity and action can make all the difference. For long-term issues like eczema or Type 1 diabetes, care is multidisciplinary—bridging pediatric nurses, dieticians, and, when needed, other subspecialists. The pediatrician acts as care coordinator, maintaining continuity, clear communication, and in-depth documentation, especially during transitions or flare-ups.
When to Consult: Signs Not to Ignore
Sometimes it’s obvious—a convulsion, prolonged fever, unexpected injury. Other moments are cloudier: a cough that lingers, a change in play behavior, excess thirst and urination. Are these worrisome—or just typical childhood tweaks? While many issues can be monitored at home, the pediatrician encourages questioning (no concern is too minor) and prompt visits when red flags arise: persistent vomiting, unexplained weight loss, or delays in motor skills like walking.
Choosing a pediatrician is personal. Many families look for proximity, a flexible communication style, capacity for teleconsultation, and proven rapport with children. The ideal is a lasting, respectful relationship—one built on trust and open dialogue.
Fee Structure and Health System Support
Costs vary widely: from private clinics to community centers, where preventive services may be free or low cost, especially for those facing financial strain. Public insurance or health systems often cover most routine check-ups (including vaccines), while additional therapies or specialty care may require supplemental coverage. Increasingly, telemedicine and community care networks are closing gaps—providing accessible, timely expertise wherever families live.
Building Trust: Transparent Communication and Medical Records
Trust is nurtured by unwavering attention to parental worries—even if the question seems basic. No issue is too small to address; every doubt is respected. Keeping a comprehensive health book—with detailed records of vaccines, measurements, and medical events—facilitates seamless, safe, and continuous care, no matter which setting the child is seen in next.
Open communication with schools, therapists, and other health professionals ensures that children with special needs receive cohesive, well-coordinated support—nothing is left to chance.
Medical Subspecialties and Pediatric Innovation
The spectrum within pediatrics is vast. Neonatology covers premature or at-risk newborns, pediatric cardiology addresses heart conditions, and pediatric neurology supports children with epilepsy, cerebral palsy, or behavioral differences. A pediatrician might also collaborate with specialists in gastroenterology, rheumatology (autoimmune conditions), or immunology (allergies, immune deficiencies).
Mental health and emotional resilience are key, too. Anxiety, school refusal, developmental challenges—all receive the pediatrician’s attention, with additional input from psychologists or psychiatrists when warranted.
Innovation is ever-present: digital tools, telehealth services, and evolving therapies continually update the care landscape. While methods advance, the basics remain: attentive examination, careful listening, and respect for the parent’s role—each one a safeguard for quality and safe care.
Emerging concerns—rising obesity, complex allergies, increasing developmental diagnoses, and workforce constraints—present new tests for the entire profession, but the pediatrician adapts, advocates, and leads research to close gaps.
Collaboration With Obstetricians, Educators, and Families
From birth, the pediatrician works side by side with mothers and obstetricians, ensuring smooth transition of care and sharing all relevant health records. Outreach involves regular communication with schools, therapists, and specialized teams to support individualized care plans.
Medication safety, too, is a family affair: the pediatrician prioritizes education about dosing, toxicity risks, and the peculiar ways in which a child’s metabolism can amplify side effects. Using the correct medication form and following dosing instructions to the letter is emphasized, protecting growing bodies from avoidable risks.
Encouraging Autonomy: Empowerment for Families
Education is ongoing. With every visit, the pediatrician encourages both parents and children to understand their health, gradually building skills and confidence for self-care. Transparent feedback, opportunities for questions, and shared decision-making lay the groundwork for a future where children grow into informed, empowered adults.
Key Takeaways
- The pediatrician stands as a science-backed partner for your child’s health, supporting every stage from the newborn period to adolescence—with deep expertise in growth, immunization, prevention, illness management, and family education.
- Regular growth monitoring, detailed medical evaluation, and vaccination guidance give peace of mind and help to catch issues early.
- Advice covers the practical and the emotional: nutrition, sleep, behavioral questions, hygiene, and accident prevention.
- When sickness strikes—be it a cough, a fever, or a chronic condition—timely intervention, clear communication, and tailored management minimize worry and optimize wellbeing.
- Pediatricians connect across clinics, hospitals, and telemedicine platforms, working alongside schools and specialists to ensure seamless, coordinated care.
- Open dialogue and a comprehensive health book strengthen trust and support continuity.
- As pediatric medicine evolves—with new therapies, digital tools, and rising healthcare challenges—the focus remains clear: individualized, proactive support for every family.
Families never have to feel isolated in facing children’s health questions. Support and trusted resources are at your fingertips—download the Heloa app for free personalized advice, health questionnaires, and tools tailor-made for families navigating every step of childhood.
Questions Parents Ask
What is the difference between a pediatrician and a general practitioner?
A pediatrician focuses exclusively on the medical needs of children—from newborns to teens—while a general practitioner cares for patients of all ages. Pediatricians receive specific training to understand childhood development, recognize unique signs of illness in kids, and address conditions more common in young patients. Their expertise includes supporting milestones, vaccination schedules, and offering advice suited to growing bodies and minds.
Can my child see a pediatrician after the age of 18?
Most pediatricians care for patients from birth through adolescence, often up to 18 years of age. Some may continue to see young adults into their early twenties, especially when a condition requires ongoing specialized care. If your family is comfortable and your child has particular health needs, you can discuss with your pediatrician about the best moment to transition to an adult healthcare provider. There’s no rush—what matters most is a smooth, supportive handover whenever the time feels right for your child.
Why should I choose a pediatrician instead of a family doctor for my child?
Choosing a pediatrician means your child benefits from care tailored to the specific needs of growing bodies and minds. Pediatricians have deep knowledge of childhood illnesses, age-appropriate development, and preventive care. They can detect subtle changes in health or behavior and guide you through every phase—offering reassurance, expert advice, and individualized attention for your child’s unique journey. Whatever the age or concern, you can count on their commitment to your family’s wellbeing.

Further reading: