Parents often confront a flurry of worries when faced with changes in their baby’s mouth—white patches, fussiness at feedings, or a sudden refusal to nurse can quickly raise alarm bells. Questions swirl: Is it just a bit of milk residue? Why does my baby seem uncomfortable, and is this an emergency? Oral thrush in infants is not only widespread but layered in its presentation, leading many to feel uncertain about what’s normal and what needs expert attention. Understanding this condition means delving into the complex interplay of biology—Candida albicans, infant immunity, frequent antibiotics, and the everyday reality of bottle nipples and pacifiers all become main characters in this story. For parents navigating the challenges of feeding and infant hygiene, clarity and empathy are more necessary than ever. Explore how to recognize the signs, untangle causes, prevent recurrence, and support your baby—while also discovering science-based reassurance for your parenting journey.
What is oral thrush in infants? Understanding the basics
Imagine a microscopic world in your baby’s mouth—delicate, complex, and constantly changing. “Oral thrush in infants” refers to a fungal infection dominated by Candida albicans, a yeast that is typically harmless but, under certain circumstances, becomes an uninvited disruptor. The immune system of neonates is, by nature, under construction—a construction site that, at times, struggles to control the blossoming of this yeast.
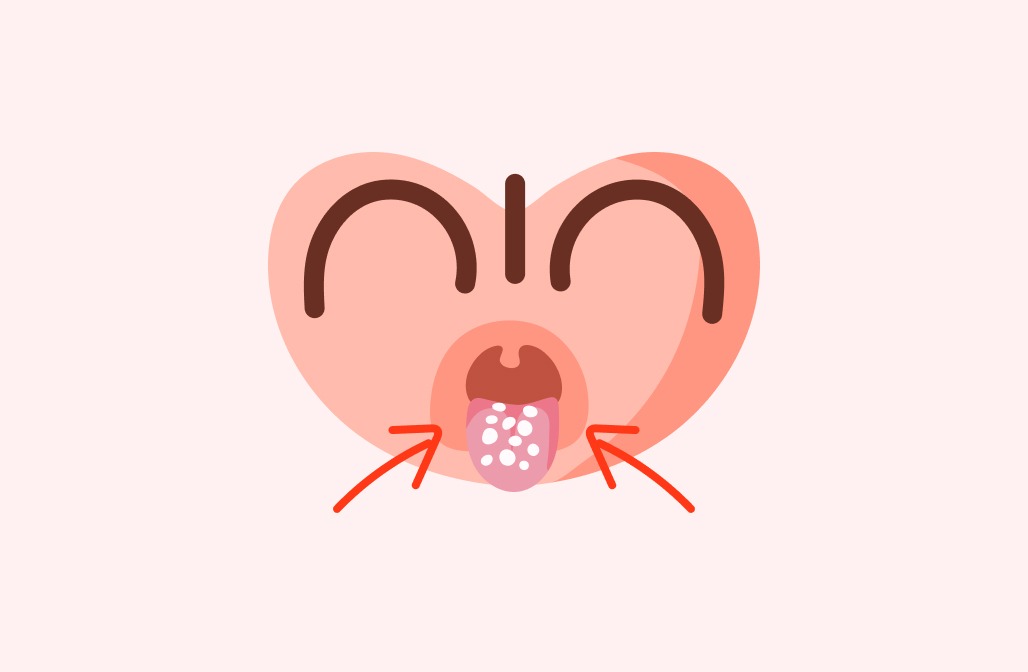
What does this look like to the naked eye? Picture patches of white, sometimes likened to cottage cheese, dotting the tongue, the roof of the mouth, gums, or cheeks. These are not fleeting milk stains; instead, they adhere stubbornly, sometimes revealing a reddened and sore surface beneath when wiped. While some infants breeze through with few symptoms, others display unmistakable distress at feeding times.
But what sets thrush apart from simple milk residue? Milk wipes away easily, while thrush clings tenaciously, marking its territory on mucosal surfaces—sometimes creating visible oral lesions that parents may confuse with other conditions.
Prevalence and risk: Why does oral thrush in infants occur?
About the “how common” question—you might be surprised how frequently pediatricians encounter oral thrush in infants. It’s especially prevalent in newborns during the first three months of life. Several factors conspire to make infants particularly vulnerable:
- Premature birth: Preemies have even less mature immune defenses.
- Recent antibiotic use: Both for the infant or a breastfeeding mother, antibiotics unintentionally sweep away beneficial bacteria, leaving Candida unopposed.
- Vaginal delivery: If the mother carries Candida albicans in her vaginal flora, passing the microbe is nearly seamless.
- Environmental influences: Crowded living conditions, humidity, and inadequate cleaning of pacifiers or bottle nipples serve as additional risk amplifiers.
Is it any wonder that parents sometimes feel guilt or anxiety? Yet, recognizing how pervasive and, in many cases, unavoidable these factors are can ease some of the stress.
The science and spread of Candida: Beyond the basics
To grasp the mechanism, imagine the oral cavity as a balanced ecosystem. Candida albicans—while a natural part of this landscape—can grow unchecked when the body’s defenses are momentarily depleted, or the bacterial landscape shifts (such as after a course of broad-spectrum antibiotics).
Babies are exposed to this yeast during birth, breast milk, or contact with contaminated hands and feeding tools. If there’s a disturbed microbiota, opportunistic infections like oral thrush in infants flourish. In rare cases, the infection can even extend to the diaper area, manifesting as a Candida diaper rash.
Recognizing oral thrush in infants: Clear signs for parents
Wondering if what you see is just the remnants of a recent feed or something more persistent? The “wipe test” often brings clarity: gently run a piece of damp gauze over the white spots. If the patches remain, or if the spot left behind is raw and inflamed, oral thrush in infants is likely. Alongside these oral signs, watch for:
- Reluctance to feed or irritability during nursing
- Increased drooling or mild discomfort
- Redness or tiny cracks at the corners of the mouth
- Occasional association with diaper rash, especially one that is stubborn or resistant to standard treatments
Feeding difficulties and persistent oral lesions should prompt a dialogue with your healthcare provider—the stakes rise if hydration or growth seem impacted.
Diagnosis: From parental observations to professional assessment
Pediatricians typically diagnose based on a physical exam—inspection of the “cottage cheese”-like spots that resist removal, multiple oral sites involved, coupled with a history of antibiotic use, family transmission, or recurrent symptoms.
Further investigations, such as fungal cultures or blood tests, are exceptions—generally reserved for unresponsive or recurrent infections, or for older infants where immune issues might be considered.
Parents play a pivotal role by reporting:
- The pattern and evolution of oral patches
- Feeding and behavioral changes
- Any maternal symptoms (especially among breastfeeding pairs)
- Recent medications or illnesses
How does oral thrush in infants spread within families?
The contagious nature of oral thrush in infants can sometimes catch families off guard. Direct contact—think shared spoons, toys, or pacifiers—facilitates transmission, as does the intimate dynamic of breastfeeding when one party harbors a Candida infection.
It is unhelpful to blame hygiene alone, yet improved cleaning regimes (sterilizing pacifiers, boiling bottle nipples, thorough handwashing) dramatically lower the risk of persistent or recurrent episodes.
Why is recurrence so common? If a breastfeeding mother has undiagnosed or untreated nipple thrush, she and her baby may continuously pass Candida back and forth—explaining why simultaneous treatment is often advised.
Treatment of oral thrush in infants: Science-backed solutions
For most families, a multi-pronged approach delivers the best results:
- Meticulous hygiene: Regularly sterilize pacifiers and bottle nipples (boiling water, steam sterilizers), clean feeding implements scrupulously after every use, and wash hands before and after any oral care.
- Gentle oral care: Wipe your baby’s mouth with damp gauze. This does not cure thrush, but can prevent further irritation and may help with comfort.
- Antifungal medications: Topical treatments such as nystatin oral suspension or miconazole gel are staples in therapy. They are directly applied to lesion sites multiple times daily—consistency and duration matter. Even when symptoms wane, completing the prescribed course ensures eradication.
- Treat both mother and baby in breastfeeding pairs: If nipples display redness, soreness, or skin peeling, topical antifungal creams for the mother—with continued attention to drying and frequent changing of breast pads—are recommended.
- Alternative feeding methods: Should suckling be exceedingly painful, feeding via cup or spoon may bridge the gap until oral thrush in infants resolves.
Unresolved thrush after a week, severe discomfort, reduced feeding or urine output, or evidence of infection spreading beyond the mouth are strong signals to reach out to a specialist.
Preventing oral thrush in infants: Proactive steps for families
In daily life, the routine can blur into monotony. Yet, within that rhythm lies the power of prevention:
- Stringent cleaning and drying of all feeding equipment
- Avoiding unnecessary antibiotic use—always under a physician’s direction
- Monitoring for early signs of infection in both baby and mother
- Supporting gentle, balanced nutrition—while there is no magic diet to prevent oral thrush in infants, healthy habits reinforce immune function
- Addressing diaper rash promptly, as concomitant infections are not rare
Proactive, attentive feeding and hygiene strategies ultimately foster a healthier, more comfortable start.
Myths, realities, and the emotional toll
It is all too common to hear outdated advice or misinformation about oral thrush in infants. Some worry it points to poor parental hygiene or “bad” caretaking, but medical evidence says otherwise: immune immaturity, environmental exposures, and normal microbial transitions are the greater culprits.
Questions about home remedies (bicarbonate-soaked cloths, herbal teas) abound. While some gentle techniques may soothe, unresolved or worsening symptoms absolutely warrant professional, evidence-based intervention—especially in infants.
For many families, the emotional impact of repeated feeds turned battles, or the sight of persistent white patches, is significant. Here, compassion and accessible support services (health providers, lactation consultants, parenting groups) offer not just care, but critical reassurance that resolution is within reach.
When to seek medical intervention: Warning signs and rare complications
While most cases of oral thrush in infants are mild and improve quickly with attention, vigilance is key. Prompt consultation is needed if:
- Your infant is younger than four months and develops thrush
- White patches stubbornly persist past one week of treatment
- There is feeding refusal, signs of dehydration (fewer wet diapers, dry mouth), or poor weight gain
- The infection recurs frequently or spreads beyond the mouth (throat, esophagus, diaper area)
- Associated fever, lethargy, or unusual illness emerge
Severe or widespread infections are rare but should never be ignored—especially in premature or medically fragile infants.
Breastfeeding, bonding, and dual care
Breastfeeding, both a source of nutrition and vital parent-infant connection, can sometimes become fraught with pain in the setting of oral thrush in infants. “Nipple thrush” manifests as soreness, redness, or peeling—symptoms which mirror oral lesions in the baby.
Rather than interrupting the breastfeeding journey, targeted antifungal treatment for both baby and mother, adjustment of feeding positions, and attention to maternal breast care empower continued closeness without undue suffering. Expressed milk may offer a temporary solution if direct nursing becomes too uncomfortable.
Healing, comfort, and parental confidence often return hand-in-hand.
Key takeaways
- Oral thrush in infants is a common, treatable condition resulting from the overgrowth of Candida albicans, often facilitated by antibiotics, immature immunity, or contaminated feeding items.
- Watch for white, creamy lesions that are firmly attached within the mouth, feeding difficulties, or unexplained fussiness. The “wipe test” helps differentiate thrush from simple milk residue.
- Consistent hand hygiene, thorough sterilization of bottles and pacifiers, and treating both mother and baby if breastfeeding reduce recurrence and speed recovery.
- Antifungal medications are effective; always finish the full course even if symptoms improve.
- Feeding, hydration, and growth should resume rapidly with effective care—persistent, severe, or recurrent symptoms require medical evaluation.
- Support and resources exist for every parent; compassionate, evidence-driven advice is always within reach.
- For personalized guidance, health questionnaires, and tailored parenting support, download the Heloa app—a partner in confident, informed parenting.
The journey through oral thrush in infants can feel overwhelming at times, but knowledge, gentle care, and expert support provide a steady path forward. Every challenge navigated is another moment of dedicated, enduring love.
Questions Parents Ask
Can oral thrush in infants go away on its own?
Oral thrush may sometimes resolve itself without treatment, especially if it’s mild and the baby’s immune system is maturing. However, it can often linger or cause discomfort and difficulties with feeding. For this reason, il est important de rester attentif au bien-être de votre bébé. If you notice persistent white patches or feeding troubles, consulting a healthcare professional offers reassurance and a tailored solution for your baby’s comfort.
Is oral thrush in infants contagious to other family members or siblings?
Yes, oral thrush can be shared between family members, particularly through close contact, shared utensils, teething toys, or during breastfeeding if the mother has a yeast infection on the nipples. Rassurez-vous, en adoptant des gestes simples comme le lavage régulier des mains, la stérilisation des biberons et tétines, et en évitant le partage d’objets mis à la bouche, le risque de transmission peut être réduit de façon significative.
What are some gentle ways to support an infant with oral thrush at home?
Supporting your baby gently during an episode of oral thrush is essentiel. You can softly clean your baby’s mouth with a piece of damp gauze or a soft cloth. Maintaining excellent hygiene of all feeding accessories supports recovery and comfort. If your baby seems uncomfortable or feeding becomes difficult, small breaks and cuddles can provide relief. And remember, il importe de demander conseil à un professionnel de santé pour une prise en charge adaptée si la situation persiste.
Further reading: